This site was made by experts: toxicologists, narcologists, hepatologists. Strictly scientific. Tested experimentally.
Author of this article, expert: gastroenterologist Daniela Sergeevna Purgina
This article was edited by gastroenterologist Daniela Sergeevna Purgina.
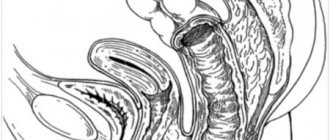
Sphincter of Oddi dysfunction (SDO) is a disease in which adequate contractile activity of the sphincter, which is located at the junction of the common bile and pancreatic ducts into the duodenum, is disrupted.
Why do we need the sphincter of Oddi
The bulk of bile is produced in the liver, and then passes through the ducts to the gallbladder. During food intake, the gallbladder contracts and the accumulated bile enters the duodenum through the ducts, where it is mixed with food and then goes to the small intestine, where the main processes of digestion occur. The timeliness of bile entering the duodenum is controlled by the sphincter of Oddi.
Being constantly in a state of increased tone, the sphincter prevents bile and pancreatic juice from entering the small intestine (although a small amount of discharge is observed even between meals). As soon as partially processed food begins to flow from the stomach into the small intestine, the sphincter of Oddi relaxes, directing small portions of the contents of the ducts into the lumen of the duodenum.
This smooth muscle can perform its function from a few seconds to a minute. The duration of work is affected by the intensity of digestion. In addition, the closed passage prevents the entry of small intestinal contents into the pancreatic and bile ducts.
What causes dysfunction?
With Oddi dysfunction, the flow of bile and pancreatic secretions is disrupted, resulting in a disorder of the digestive mechanism. Why could this happen? For different reasons. Pathology can be of different nature:
- Organic. Disruption of the functioning of an organ of an organic nature occurs due to inflammation, as well as pathologies such as hyperplasia or fibrosis of the duodenal mucosa, strictures of the biliary tract, and undiagnosed stones of the common bile duct.
- Functional.
Functional reasons may include:
- gastritis;
- diseases of the liver and biliary tract;
- pancreatitis;
- peptic ulcer;
- intestinal diseases;
- diabetes;
- autoimmune diseases;
- treatment of diseases with hormonal drugs;
- pathologies of the adrenal glands;
- thyroid diseases;
- postoperative period after removal of part of the intestine, stomach.
Very often, this complication occurs after cholecystectomy: surgery to remove the gallbladder. The reason is that after such a surgical intervention, a significant increase in pressure occurs in the entire biliary tract, even with a weak contraction of the sphincter of Oddi.
Either a spasm of this smooth muscle can occur, or vice versa, constant relaxation, in which bile enters the lumen of the duodenum all the time (and not just when needed).
Symptoms of the disease
Symptoms of this disorder can manifest in different ways. Most often, patients are concerned about:
- pain in the stomach (epigastric region) and right hypochondrium. The pain may last for 30 minutes or more in a row, alternating with pain-free periods;
- over the course of 12 months, the patient has experienced at least one such pain attack (or more);
- persistent pain makes it difficult to do any work and requires seeing a doctor;
- however, there are no structural changes in organs that could explain the development of pain. Ultrasound of the liver, pancreas, gall bladder shows normal.
Patients note that the first attacks of pain appear 2–3 hours after eating food.
Literature
- McNally P.R. Secrets of gastroenterology. Moscow. "Publishing house BINOM". 1999. P. 359.
- Brandstatter G, Schinzel S, Wurzer H. Influence of spasmolytic analgesics on motility of sphincter of Oddi. Dig Dis Sci 1996;41:1814-8.
- Geenen JT, Hogan J, Dodds WJ, et al. The efficacy of endoscopic sphincterotomy in post-cholecystectomy patients with sphincter of Oddi dysfunction: Results of a four year prospective study. N Engl J Med.
- Hogan W.J. Clinical manifestations and diagnosis of sphincter of Oddi dysfunction. UpToDate.com, 1999.
- Hogan WJ, Geenen JE. Biliary dyskinesia. Endoscopy 1988;20(Suppl.1):179-83.
- Khuroo MS, Zargar SA, Yattoo GN. Efficacy of nifedipine therapy in patients with sphincter of Oddi dysfunction: a prospective, double-blind, randomized, placebo-controlled, cross-over trial. Br J Clin Pharmacol 1992;33:477-85.
- Luman W, Williams AJ, Pryde A, et al. Influence of cholecystectomy on sphincter of Oddimotility. Gut 1997;41:371-4.
- Prajapati ND, Hogan WJ Sphincter of Oddi dysfunction and other functional biliary disorders: evaluation and treatment. Gastroenterol Clin N Am 32 (2003) 601–618.
- Rolny P, Geenen JE, Hogan WJ. Post-cholecystectomy patients with 'objective signs' of partial bile outflow obstruction: clinical characteristics, sphincter of Oddi manometry findings, and results of therapy. Gastrointest Endosc 1993;39:778-81.
- Rosenblatt ML, Catalano MF, Alcocer E, et al. Comparison of sphincter of Oddi manometry, fatty meal sonography, and hepatobiliary scintigraphy in the diagnosis of sphincter of Oddi dysfunction. Gastrointest Endosc 2001;54:697-704.
- Sherman S, Troiano FP, Hawes RH, et al. Frequency of abnormal sphincter of Oddi manometry compared with the clinical suspicion of sphincter of Oddi dysfunction. Am J Gastroenterol 1991;86:586-90.
- Toouli J, Roberts-Thomson IC, Dent J, et al. Manometric disorders in patients with suspected sphincter of Oddi dysfunction. Gastroenterology 1985;88:1243-50.
- Varadarajulu S., Hawes R. Key issues in sphincter of Oddi dysfunction Gastrointest Endoscopy Clin N Am 13 (2003) 671-694.
- Wehrmann T, Seifert H, Seipp M, et al. Endoscopic injection of botulinum toxin for biliary sphincter of Oddi dysfunction. Endoscopy 1998;30:702-7.
Forms of the disease
Doctors divide patients with DSO into 2 large groups:
- With dysfunction of the bile segment. Such patients make up the majority.
- With disorders of the pancreatic segment of the mucous membrane.
For a long time, doctors have identified the following types of sphincter of Oddi dysfunction:
- Biliary I - characterized by moderate or severe pain that spreads to the right shoulder, back, and sometimes neck. The duration of the attack is at least 20 minutes. With ERCP (endoscopic retrograde cholangiopancreatography, joint examination with a probe and radiography), an increase in contrast release time is diagnosed: more than 45 minutes. The common bile duct becomes wider by 12 mm or more, and the level of transaminases and (or) alkaline phosphatase increases by 2 times.
- Biliary II - sphincter dysfunction according to biliary type II is characterized by a classic attack of biliary pain, as well as the manifestation of one or two signs of type I. The presence of both structural and functional disorders is noted. According to a manometric study, this variant of DSO is diagnosed in 50–63% of cases.
- Biliary III - characteristic attacks of biliary pain without other signs. Only functions are impaired, without any more severe deviations. This is the rarest variety.
- Pancreatic - pain typical of chronic pancreatitis (in the stomach area, radiating to the back). When bending forward, the pain decreases. There is a high level of amylase and lipase enzymes in the blood plasma. This type, according to manometric studies, is detected in 39–90% of patients.
In 2021, the IV revision of the Rome criteria for functional disorders of the biliary tract took place. As a result, of the three biliary subtypes of DSO, only one was left: the second, as the most typical and most treatable. However, some doctors continue to use the expanded classification for convenience and greater accuracy.
Pancreatic DSO
Clinically it can manifest itself as recurrent chronic pancreatitis. For this form of DSO, 3 types have also been identified [11].
- The first type: pain of a pancreatic nature, amylase or lipase is 1.5-2 times higher than normal, dilatation of the pancreatic duct is more than 6 mm in the head and 5 mm in the body of the pancreas.
- The second type: pain of a pancreatic nature and 1 of the following signs - amylase or lipase is 1.5-2 times higher than normal, dilatation of the pancreatic duct is more than 6 mm in the head and 5 mm in the body of the pancreas.
- Third type: only a typical attack of pancreatic pain.
What examinations need to be completed
Dysfunction of the sphincter of Oddi is diagnosed by excluding other causes that may cause such symptoms: cholelithiasis, choledocholithiasis, pancreatitis.
Laboratory research methods include:
- Biochemical blood test: ALT, AST, GGTP, alkaline phosphatase, bilirubin, total and pancreatic amylase.
- Fecal elastase to exclude exocrine pancreatic insufficiency.
Instrumental research methods:
- Ultrasound examination It is possible to perform ultrasound with a sample, but this is technically difficult to perform, since such accurate visualization is often difficult. Using this method, you can determine the size of the common bile duct and pancreatic duct. Measurements are recorded every 15 minutes, the total time period is 1 hour. A clear sign of sphincter of Oddi dysfunction will be an expansion of more than 2 mm.
- Cholescintigraphy, which is used to determine the period of movement of the isotope with bile from the liver to the small intestine. With DSO, a delay in this transit is diagnosed.
- ERCP (retrograde cholangiopancreatography). The patient is injected with contrast using a probe, after which an x-ray is taken. If an expansion of the common bile duct is detected by more than 12 mm, and the release of the contrast takes more than 45 minutes, then the diagnosis is confirmed.
- Endoscopic manometry of the sphincter of Oddi is the most accurate method for directly measuring sphincter tone. If the pressure in the common bile duct is 10 mm Hg. higher than the pressure in the duodenum, then the pathology is not diagnosed, this is the norm. In the case of spastic contraction of the sphincter, the pressure rises to approximately 110 mm Hg. This method is technically complex, complications are possible after implementation, and there are also a number of contraindications, so it is used infrequently.
- The “gold standard” is MR cholangiography, which allows for a detailed assessment of the patency of the bile ducts.
Treatment
The approach to the treatment of such patients must be differentiated because the patient group is very heterogeneous. The main clinical manifestation of the syndrome is pain, and it is by its reduction that the success of treatment can be judged. Because In a number of patients with DSO, the occurrence of pain syndrome is associated with the intake of fatty foods and alcohol; it is rational to prescribe a diet similar to that for cholelithiasis. Drug treatment consists of prescribing nitrates and calcium channel blockers. For example, nifidepine proved its effectiveness in a placebo-controlled study [6]. Nitrates reduce the tone of the sphincter of Oddi in humans and animals [2], however, I have not seen any controlled studies of the effectiveness of this group of drugs in DSO. Recently, we have been trying to make wider use of antispasmodics that selectively act on the sphincter of Oddi - dicetel and duspatalin in standard dosages. They solved the unwanted cardiovascular effects inherent in the first two drugs, but there is not enough information about the degree of their effectiveness in DSO. From personal experience, the drugs lead to relief of the symptoms of “biliary” and “pancreatic” pain in a number of patients with the dyskinetic form of DSO. The positive effect of these drugs may be associated with their effect on intestinal smooth muscles, given that the combination of DSO with other dysmotor disorders of a functional nature is very likely [13]. In addition, a positive clinical effect is sometimes achieved by prescribing lyolytic therapy with ursodeoxycholic acid drugs at a dosage of 10 mg/kg body weight per day for 3-6 months. One of the possible explanations for the positive result of using this drug is the dissolution of microliths that are not detected by ultrasound.
Endoscopic sphincterotomy (EST). This is a very effective intervention that greatly facilitates the lives of patients, provided that patients are selected correctly. It is absolutely indicated for patients of group 1 and patients of groups 2-3, subject to increased basal pressure of the sphincter of Oddi. This conclusion was made based on a study of the effectiveness of PST in patients of different groups. Thus, in patients of group 1, a positive effect from sphincterotomy is observed in the vast majority of cases and, interestingly, was observed even in patients of this group with normal basal pressure in the sphincter [9]. In patients of group 2 and with increased basal pressure in the sphincter of Oddi, PST led to a positive clinical result in approximately 90% of cases; in the absence of this criterion, the intervention was ineffective [3]. Geenen JT et al. randomized patients with elevated and normal sphincter pressure to PST and “sham” PST. The percentage of patients with improvement after real and sham PST in the normotensive group did not differ significantly (42% and 33%, respectively), whereas in patients with pressure above 40 mm H2O, sphincterotomy resulted in a much higher percentage of clinical improvement than sham sphincterotomy (91% and 25% respectively) [3]. Patients in group 3 have the lowest effectiveness of PST, even with increased pressure in the sphincter [13]. Because In our work, we have decided on the possibility of measuring pressure, then in the 2nd groups we perform PST when strictures are detected on RCP or when the emptying of the common bile duct is slowed down, as well as in patients of this group with ineffective drug therapy and severe pain. We try not to perform PST in patients of the 3rd group (considering that in this group the percentage of cases of increased basal pressure in the sphincter of Oddi is small and, therefore, only a small part of patients will benefit from performing PST; in addition, they have a higher risk of developing pancreatitis and less effective PST). As for the pancreatic form of DSO, we perform PST only if biliary-pancreatic reflux is detected.
We have not used surgical sphincterotomy, sphincteroplasty and sphincter excision, described as a treatment for DSO, in our practice. In any case, only manometric data that accurately verifies DSO and the ineffectiveness of all the methods described above can justify such highly invasive interventions.
Injection of botulinum toxin into the sphincter can be effective in a number of patients [14]. However, the question of the degree and duration of the positive effect remains open.