Pain in the right hypochondrium, acute or periodic, manifests itself in some form in approximately a third of the population of our planet. Very often, patients are interested in what is on the right side of a person and why there is pressure, tugging, aching or pain in the right hypochondrium. According to medical statistics, in approximately ninety percent of cases, pain is a consequence of pathological changes in internal organs. Thus, most often these symptoms are caused by diseases of the biliary tract and gall bladder, and the second most common place is occupied by liver pathologies and the development of liver edema in case of circulatory disorders.
Causes of heaviness in the hypochondrium
Biliary dyskinesia
Heaviness under the ribs on the right is a typical manifestation of the hypokinetic-hypotonic variant of JP. An unpleasant sensation bothers a person constantly and intensifies 40-60 minutes after eating food. Patients experience a feeling of fullness in the stomach, mild aching pain in the right hypochondrium. If there are errors in the diet, belching and bitterness in the mouth appear. Heaviness in the hypochondrium decreases when following a low-fat diet, after taking choleretic drugs.
Hepatitis
Regardless of the etiological factor, with acute inflammation of the liver, overstretching of its capsule occurs, which is manifested by severity and moderate pain in the right hypochondrium. Symptoms are observed constantly, without any visible connection with a violation of the diet. The uncomfortable feeling intensifies when the body is tilted to the right, when palpating the projection area of the organ. Aching pain worsens with physical activity.
In addition to heaviness in the side, signs of dyspepsia are troubling: nausea and vomiting, poor appetite or lack thereof, unstable stool. Yellowness of the skin, mucous membranes, and sclera is often noticeable. The disease is accompanied by fever and asthenovegetative symptoms. This clinical picture is determined by different types of hepatitis: viral, autoimmune, alcoholic.
Cholecystitis
Violation of the outflow of bile provokes discomfort and heaviness in the area of the right hypochondrium, which intensifies half an hour to an hour after finishing a meal. Such symptoms are characteristic of the chronic course of inflammation of the gallbladder, mainly for its acalculous form. With calculous cholecystitis, in addition to heaviness in the hypochondrium, patients experience intense pain similar to biliary colic, which develops after eating fatty and heavy foods.
Heaviness in the hypochondrium
Parasitic infections
Heaviness in the projection of the right hypochondrium is noted with the invasion of helminths that affect the liver parenchyma. These include echinococcosis and alveococcosis. At the first stage, when the parasite invades the liver, patients feel slight discomfort and heaviness in the hypochondrium after a heavy meal. Dyspeptic disorders are not detected at this stage.
An enlarged hydatid cyst leads to increased symptoms. Patients complain of constant heaviness, bursting sensations, loss of appetite, nausea and vomiting. After finishing eating or exercising, there is a dull pain in the liver area. Diarrhea associated with disorders of bile formation and bile excretion occurs periodically. With a complicated course and rupture of the cyst, acute pain appears.
Liver neoplasms
Benign liver tumors are mild in severity with discomfort in the right abdomen. They grow slowly and do not interfere with digestion. Large cysts cause a feeling of fullness in the hypochondrium, which intensifies after eating. Liver cancer is characterized by early onset of dyspeptic disorders, lack of appetite, and sudden weight loss in patients. As the tumor grows, heaviness in the hypochondrium is replaced by constant dull pain.
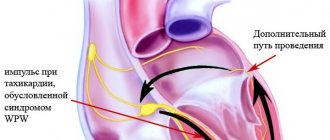
Cardiac diseases
Right ventricular heart failure is accompanied by stagnation in the systemic circulation, which causes a feeling of fullness and heaviness in both hypochondriums. Patients notice an enlarged abdomen, difficulty bending the body, and rapid fatigue when walking. Symptoms may occur with more rare cardiac pathologies - mitral-tricuspid disease, tricuspid stenosis, post-pericardiotomy syndrome.
Spleen diseases
Heaviness in the left hypochondrium most often develops against the background of diseases of the spleen. In this case, the unpleasant symptoms are not associated with errors in nutrition, but intensify during bending and physical activity. Heaviness, moderate aching pain are manifestations of splenomegaly caused by infections (malaria, leishmaniasis, mononucleosis), hemoblastoses (leukemia, lymphogranulomatosis), autoimmune processes (SLE, periarteritis, vasculitis).
Rare causes
- Diseases of the respiratory system
: lower lobe pneumonia, exudative pleurisy. - Rare hepatobiliary pathologies
: liver peliosis, perihepatitis, amoebic liver abscess. - Vascular damage
: portal vein thrombosis, splenic vein thrombosis, Budd-Chiari syndrome. - Congenital diseases
: Crigler-Najjar syndrome, Gilbert's disease, hereditary anemias (microspherocytosis, thalassemia).
Syndrome after cholecystectomy in the practice of a general practitioner and gastroenterologist
The problem of recurrent pain that develops or recurs after cholecystectomy has appeared recently in historical terms, just as the first cholecystectomy was recently performed - in 1882 by the German surgeon C. Langebuch. At the same time, he formed the concept that made it possible to carry out this operation: “The gallbladder should be removed not because it contains stones, but because it produces them.” The attractiveness of this concept is that it creates a false impression of the therapeutic effect of removing the gallbladder, and not of the costs that the disease leads to and which force the removal of a very important functional organ. Already 40 years after the start of surgical removal of the gallbladder, it became clear that not all patients experience improvement (in some patients, pain persists, in others new sensations appear that worsen the quality of life). In 1926 [1], the French surgeon Mally-Guy proposed the term “postcholecystectomy syndrome” (PCES), which included purely surgical aspects (surgical injury to the ductal system of the liver; leaving a long stump of the cystic duct, operations in the “acute period” of the disease, etc. .). The very experience of that time (6000 cholecystectomies), when 497 reoperations were required (which amounted to 8.1%), led to the understanding that even in a purely surgical concept, PCES is heterogeneous. In addition to surgical heterogeneity, functional disorders began to be recorded, based not on surgical errors, but on the operation itself [1]. It became clear that some of the reasons were associated with insufficient preoperative examination of patients and after surgery the clinical manifestations returned again, some of the manifestations worsened, and new ones appeared. Recent statistics (Zvyagintseva T.D., Shargorod I..I., 2011 [7]) show that only 46.7% of operated patients experience improvement, in 25% the operation does not bring relief, and in 28% a return is recorded attacks [7]. PCES began to increasingly take on general medical significance, and not only surgeons, but also gastroenterologists and therapists began to be involved in its study [2–4]. From today’s point of view, “postcholecystectomy syndrome” is a collective concept that unites a variety of pathological conditions that arise directly or indirectly after cholecystectomy and sometimes have no causal connection with the absence of a gallbladder in the patient, but are accompanied by chronic recurring pain without a clear source [5, 6] . At the same time, the Rome Consensus II (1999) proposes to consider postcholecystectomy syndrome as a purely functional disorder, characterized by dysfunction of the sphincter of Oddi (SDO), caused by disturbances in its contractile function, complicating the normal outflow of bile into the duodenum in the absence of organic obstacles.
From this time on, a new (therapeutic) period begins in the study of PCES and successes in its treatment begin to largely depend on pharmacotherapeutic effects.
What makes up and what explains the physiology of bile movement:
If you have a gallbladder
- hepatic secretion;
- rhythmic activity of the sphincters of the terminal part of the common bile duct;
- normal functioning of the gallbladder sphincter;
- normal operation of the cystic duct valve;
- absorption function of the mucous membrane of the gallbladder and ducts.
All these anatomical and functional formations participate in the formation (form) of the pressure gradient, which is the engine of bile. The movement of bile through the duct system also depends on the phase of digestion:
- outside the digestion phase, bile enters the gallbladder at the moment of closure of the sphincter of Oddi (SO), while in small portions it also enters the duodenum, so the SO is not permanently closed;
- during the digestion phase, the CO opens, the gallbladder contracts and bile enters the duodenum, participating in the emulsification of fats and the activation of digestive enzymes, triggering intraluminal digestion [8, 9].
With the removal of the gallbladder from the system that forms the pressure gradient, a very important link in this important (to a large extent) self-regulating system is excluded and the entire system begins to function according to the laws of pathophysiology.
The main pathogenetic links are represented by the following provisions:
- A necessary condition for ensuring local self-regulation is the presence of CO and the gallbladder.
- In the absence of the gallbladder (cholecystectomy), the process of regulation and self-regulation is disrupted, the main self-regulating formation becomes the SO, which, in the absence of the gallbladder, shows constant readiness for dysfunction.
- The work of the CO begins to largely depend on the pressure gradient (liver, ducts, duodenum).
- With low CO tone, bile is constantly discharged into the duodenum and in a short time chronic biliary insufficiency develops with indigestion of fats.
- In some patients, RS tends to spasm, which forms pain symptoms (paroxysmal, constant).
- At different periods of time, SO dysfunction can be of a different nature and form different clinical symptoms.
- In some patients, at different times after cholecystectomy, bacterial overgrowth syndrome (BOS) develops, leading to duodenal hypertension, changing the pressure gradient and passage of bile (with stagnation in the ducts).
- In some patients, duodenal hypertension develops due to chronic biliary insufficiency and intestinal digestion disorder, leading to intestinal hypertonicity.
- In some patients, impaired intestinal tone and abdominal hypertension lead to duodenogastric reflux and reflux gastritis.
Based on the above and the recommendations of the Rome Consensus II and III, which recommended considering PCES as a consequence of dysfunction of the sphincter of Oddi, the following options for PCES can be distinguished:
- spastic variant;
- variant with CO deficiency, chronic biliary insufficiency and fat digestion disorders;
- option with SIBO, duodenal hypertension, DSO, stagnation of bile in the ducts;
- option with CO dysfunction, with chronic biliary insufficiency, fat digestion disorders, intestinal hypertension, CO spasm;
- the same with duodenogastric reflux, reflux gastritis [9].
Based on the above and relying on the recommendations of the Rome Consensus II and III, the recommendations of the Society of Gastroenterologists, we proposed our own definition of PCES in 2012.
PCES should be interpreted as a functional disorder that develops after cholecystectomy and is largely associated with dysfunction of the sphincter of Oddi, not only of the biliary type, but also of the pancreatic type. PCES also includes other functional disorders (duodenostasis, chronic biliary insufficiency, bacterial overgrowth syndrome, functional intestinal disorders, duodenogastric reflux).
From our point of view, this definition has greater practical significance, since it clearly defines the nature of treatment and allows all factors influencing the formation of PCES to be divided into two main groups:
- Contributing (sphincter of Oddi dysfunction).
- Allowing:
— bacterial overgrowth syndrome; - duodenal hypertension; — chronic biliary insufficiency; - intestinal and abdominal hypertension; - duodenogastric reflux.
Identification of these factors allows you to most adequately create an examination program, formulate a diagnosis and prescribe treatment.
Statistics
- Every year, about 2.5 million planned and emergency operations are performed on the biliary tract around the world.
- There are 600,000 cholecystectomies performed annually in the United States.
- In Russia, until 2012, 340,000 cholecystectomies were performed. In the last 2 years, 500,000 cholecystectomies have been performed.
- Postcholecystectomy syndrome develops in 5–40% of operated patients (both are correct and depend on the time of group formation and the nature of the operations) [10].
The statistics presented are very important, because they, unfortunately, indicate an increase in operations for cholelithiasis, which, in turn, leads to an increase in the number of patients suffering from PCES.
Since the main factor contributing to the formation of PCES is SO dysfunction, we would like to present in this report the recommendations of the Rome Consensus II and III on this disorder. The Rome Consensus II (2002) proposes to distinguish two clinical types of DSO:
- biliary;
- pancreatic.
The biliary type has three subtypes.
The first is characterized by an attack of pain in the right hypochondrium (with or without irradiation) in combination with the following three signs:
a) an increase in AST and (or) alkaline phosphatase by 2 or more times with double measurements (during an attack); b) delayed release of contrast agent during endoscopic retrograde pancreatocholecystography (ERCP) (more than 45 minutes); c) expansion of the common bile duct more than 12 mm.
The second is an attack of pain with one or two signs.
The third is characterized only by attacks of pain.
The pancreatic type of DSO can be represented by classic pancreatitis with epigastric pain and increased serum amylase and lipase. In less severe forms of pain there is, but no increase in enzymes.
In cases where ERCP excludes the absence of stricture pathology, manometry of the biliary and pancreatic sphincters is indicated.
The Rome Consensus III (2006) retained the main types of dysfunction, but recommended excluding instrumental studies as more dangerous than the pathology itself (ERCP, manometry).
In this regard, the diagnostic range of studies should include:
- transabdominal ultrasonography;
- esogastroduodenoscopy with targeted examination of the FS;
- ultrasound examination (ultrasound) with assessment of the functional state of the mucus (nutritional and pharmacological tests);
- endoscopic ultrasonography;
- dynamic echography;
- dynamic cholecystography with T 99;
- hydrogen test;
- X-ray examination (if gastroduodenostasis syndrome is suspected, the clinical manifestations of which are heaviness and pain in the epigastric region with possible irradiation to both the right and left hypochondrium, a feeling of nausea, rapid satiety, vomiting, which brings relief).
X-rays show an increase in the volume of the stomach and duodenal bulb, and impaired evacuation from the stomach, mainly due to low muscle tone. The lumen of the duodenal bulb is expanded, the progress of contrast is slow, the backflow of contents from the duodenum into the stomach is recorded, peristalsis is sluggish, propulsive ability is sharply reduced [11].
Establishment of biliary insufficiency. Biliary insufficiency (BI) is a symptom complex of digestive disorders that develops either as a result of a decrease in the production of bile and bile acids, or as a result of irreplaceable losses of bile acids. BN is recorded by measuring the amount of bile and the decrease in bile acids entering the intestine 1 hour after the introduction of the irritant.
For patients after cholecystectomy, we proposed dynamic ultrasonography with food load. The technique for doing it is as follows.
- The diameter of the common bile duct (CBD) is searched and determined on an empty stomach.
- A food load is given: 20 grams of butter, cheese, sweet tea - 6.5 g/sugar, white bread.
- 30 minutes after the food load, the CBD diameter is searched and determined.
- 1 hour after the food load, search and determine the CBD diameter again.
- Clinical symptoms, their appearance, increase, duration or absence are also recorded. All these data are entered into the study protocol [8].
Interpretation of the research results:
30 minutes after the food load.
1. Dilation of the common bile duct after a food load may indicate either a spasm of the CO or organic stenosis. 2. A reduction in the diameter of the common bile duct indicates the normal functioning of the CO (an increase in bile synthesis after a food load changes the pressure gradient, and the CO opens - a physiological reaction). 3. The absence of fluctuations in the diameter of the common bile duct after a food load may indicate either CO hypotension or CO due to the adhesive process.
60 minutes after the food load:
4. The dilation of the duct increases, pain appears and intensifies. This is most likely evidence of SO stenosis. 5. The original diameter of the common bile duct is preserved, or the existing expansion is preserved without pairs (confirms point 2 - normally functioning CO). 6. Preserved original diameter of the common bile duct.
This study fully meets the requirements of the Rome Consensus III (so that the study itself is no more dangerous than the pathology that is being diagnosed) and provides information sufficient to make a treatment decision.
After establishing (suspicion) the presence of chronic biliary insufficiency, its degree is determined. The characteristics are presented in table. 1.
The importance of this definition is related to the physiological role of bile in digestion.
- Neutralization of acidic food gruel coming from the stomach into the duodenum.
- Activation of intestinal and pancreatic enzymes.
- Emulsification of fats, due to which the action of lipase is carried out over a larger surface.
- Activation of lipase, which promotes hydrolysis and absorption of fat digestion components.
- Facilitates the dissolution in water and absorption of fat-soluble vitamins A, D, E, K.
- Bilirubin, cholesterol, metabolic products of sex hormones, the thyroid gland and adrenal glands are removed from the blood with bile.
- Activation of intestinal motility.
- Excretes salts of heavy metals, poisons, medicinal and other substances.
Since duodenal intubation after cholecystectomy is associated with technical difficulties, this interpretation can be based on the clinical equivalents presented in Table. 2.
Our experience in diagnosing and treating patients with PCES
We studied 140 patients in whom pain in the right hypochondrium, epigastric region or left hypochondrium persisted, appeared, intensified, or changed at different times after cholecystectomy (from 6 months to 19 years, mostly women 110/30, age from 19 to 74 years). The nature of the survey is presented above.
As a result of the study, it was established:
- 60 patients had either SO spasm or its insufficiency (according to the prevailing clinical and instrumental symptom complex);
- 50 patients had a predominant failure of the mucous membrane with chronic biliary insufficiency;
- in 20 patients, in addition to DSO, gastroduodenostasis and SIBO were recorded;
- 40 patients - DSO, biliary insufficiency, indigestion (mainly fats), intestinal dysfunction with increased intra-abdominal pressure, gastroduodenostasis, reflux gastritis.
The research results and analysis of clinical manifestations allowed us to make the following diagnoses (within the framework of one nosology - PCES).
- Postcholecystectomy syndrome: spastic dysfunction of the sphincter of Oddi.
- Postcholecystectomy syndrome: hypokinesia of the sphincter of Oddi, chronic biliary insufficiency I, II, III degrees.
- Postcholecystectomy syndrome: dysfunction of the sphincter of Oddi (biliary 1, 2, 3; duodenogastrostasis, bacterial overgrowth syndrome 1st, 2nd, 3rd stage).
- Postcholecystectomy syndrome: DSO (biliary type), chronic biliary insufficiency, digestive disorder (mainly fats), intestinal functional disorder with a predominance of hypertension, duodenostasis.
- Postcholecystectomy syndrome: dysfunction of the sphincter of Oddi with a predominance of hyperkinesia, duodenogastrostasis, reflux gastritis.
After the diagnosis has been made and its pathogenesis has been deciphered, treatment is prescribed, the general principles of which can be reduced to the following provisions.
- Dietary therapy is considered an important component of treatment. In terms of timing - diet of the early postoperative period: split 6 meals a day with the last meal before bed, limiting fat, adding foods containing fiber to the diet, vegetables and fruits must be thermally processed. The diet of the period of functional adaptation preserves the fragmentation of nutrition with the restoration of existing restrictions. Diet for the period of uncompensated biliary insufficiency and impaired digestion of fats. It is necessary to restore fats in the diet in combination with replenishment of bile acids and enzymes.
- Pharmacotherapy depends on the form and severity of PCES (both main and associated symptoms are taken into account):
- anticholinergics;
- nitrates;
- calcium channel blockers;
- myotropic antispasmodics;
- “motor regulators”;
- anti-inflammatory (mainly antibiotics, antibacterial drugs are non-absorbable when SIBO is established);
- ursodeoxycholic acid preparations (if chronic biliary insufficiency (CBF) is established, the dose of which depends on the degree of CBI);
- enzyme preparations (for indigestion, mainly fats).
- Therapy should be permanent (duration and intensity are developed individually).
Own data
The first 2 variants of PCES - 60 patients (30 men, 30 women), age from 20 to 77 years. The duration of cholecystectomy ranges from 6 months to 19 years. All patients had pain in the right hypochondrium or epigastric region associated with eating. Pain occurred at different times after cholecystectomy, in 3 patients it was progressive in nature (in some patients the pain was paroxysmal, in some it was constant, aching, worsening after eating).
The patients underwent an ultrasound of the abdominal organs (with food load), and it was found that in 23 patients the common bile duct was 1.1–1.2 cm; in 37 patients the common bile duct was 0.5–0.6 cm.
Results of the study of the CBD after a food load:
| A) after 30 minutes 1 - 25 patients 2 - 21 patients 3 - 14 patients | B) after 60 minutes 4 - 4 patients 5 - 34 patients 6 - 22 patients |
Thus, spasm of the sphincter of Oddi or its organic stenosis was detected in 38 patients, which amounted to 60.38%; in the remaining 22 patients, insufficiency of the sphincter of Oddi was detected. This group of patients had no signs of gastroduodenal stasis and SIBO. It should be noted that the tendency of the CO to spasm is typical for patients in the early stages after cholecystectomy (the early period after surgery is the 1st year and the initial period of adaptation is 1–3 years; in subsequent years, CO deficiency was more often recorded).
Treatment of patients with the 1st variant of PCES - spastic
Choice of myotropic antispasmodic
The characteristics of drugs that have an antispasmodic effect are presented in Table. 3. It also shows the zone of distribution of the effect, which is important for treatment, since the drug should be characterized by the most selective effect.
As can be seen from the table presented, hymecromone (Odeston) has this effect.
Odeston (hymecromone) is a synthetic analogue of umbealopherin found in anise and fennel fruits, which are used as antispasmodics (papaverine-like effect). The second effect is related to its relationship with cholecystokinin (it affects the gallbladder and ducts as an antagonist, and has a synergistic effect on the sphincter of Oddi).
The initial dose of Odeston was 200 mg (1 tablet) × 3 times with a possible dose increase to 1200 mg/day, the duration of treatment was 3 weeks (as monotherapy). In 34 patients, pain decreased significantly during the 1st week of treatment; 11 patients subsequently required an increase in the dose of the drug to 800–1000 mg/day. In 4 patients, despite treatment, pain persisted. The lack of effect was regarded as a consequence of organic stenosis. They conducted a contrast study of the biliary ducts, established stenosis of the common bile duct (or the terminal part of the common bile duct), and performed papillosphincterotomy with effect.
These data allowed us to conclude that:
- Ultrasound with food load in patients after cholecystectomy makes it possible to establish the type of DSO and select an adequate antispasmodic.
- Odeston is a selective antispasmodic in relation to SO and is most effective for the treatment of type 1 PCES (spastic).
- The lack of effect of treatment with Odeston is the basis for a contrast study of the biliary ducts in order to establish organic stenosis and its degree and subsequent surgical treatment.
Treatment of patients with the 2nd variant of PCES (hypokinetic dysfunction of CO and chronic biliary insufficiency)
This group included 22 patients who, in addition to hypokinesia SO and CBN, had no signs of indigestion, SIBO and gastroduodenostasis. The treatment used was the motility regulator Itomed (Czech Republic), the mechanism of action of which is the blockade of D2 receptors and blockade of cholinesterase (thereby potentiating the effect of acetylcholine). Acting throughout the gastrointestinal tract, it affects the pressure gradient, restoring the passage of bile and increasing the tone of CO. Ursosan, a preparation of ursodeoxycholic acid (URDC) (Czech Republic, Pro-Med), was used to replenish bile acids. The daily dose of Itomed was 50 mg × 3 times, the dose of Ursosan depended on the degree of biliary insufficiency (7 patients had a mild degree - they received 500 mg/day, 15 patients had a moderate degree of biliary insufficiency - the dose of Ursosan was 750 mg/day, which they received in one reception at night). The duration of treatment is 3 weeks.
As a result of the treatment, pain (discomfort in the epigastric region and right hypochondrium) was relieved by the 10th day of treatment. Patients receiving 750 mg of Ursosan had an effect within the same time frame, but it was characterized by greater stability.
Discussion . Considering the impossibility of changing the anatomical and functional situation and the failure of the SO, therapy with “motor regulators” should be resorted to when pain appears. The duration of their use should be determined by the stability of pain relief. Biliary insufficiency requires constant replenishment with bile acid preparations. The present period of time is characterized by the development of doses and duration of administration. We are studying similar options (10 days of each month, a month of each quarter, constant use of small doses of 250–500 mg/day). Each of these regimens may be sufficient for a particular patient. The criterion for the effectiveness of treatment is the absence of progression of biliary insufficiency and the absence of signs of impaired digestion of fats.
Treatment of patients with the 3rd variant of PCES
CO dysfunction (according to the predominant component), duodenogastrostasis, SIBO. The observation group consisted of 40 patients (mostly women 30/10), age from 40 to 70 years. Alpha Normix was used as a basic therapy in a daily dose of 200–400 mg (every 8–12 hours), the dose of the drug and duration of treatment depended on the severity of SIBO (1st, 2nd, 3rd degree), duration of treatment 7 -10 days. The effectiveness of treatment was monitored using a hydrogen test. The convenience of the test is the speed of obtaining an answer. Since SO dysfunction was multidirectional, Trimedat (trimebutine), which belongs to the group of opiate peptides and is an agonist of peripheral μ-, δ- and κ-opiate receptors, was used as a motility regulator. Since these receptors form multidirectional effects, the overall effect is regulatory in nature. In this version of PCES, the objects of influence are DSO, duodenogastrostasis, formed and maintained by SIBO. In addition, the drug changes visceral sensitivity, which is important in the treatment of functional disorders. The daily dose of Trimedat was 600 mg (3 tablets). The total duration of treatment is 3 weeks.
Efficacy: pain, discomfort, rapid satiety, bloating of the upper abdomen and bowel disorders were relieved within 10 days. The speed of onset of the effect depended on the relief of SIBO, which, in all likelihood, maintained gastroduodenostasis and provoked DSO.
Thus, the basic drug in the treatment of the 3rd option is a non-absorbing antibiotic (Alpha Normix), which stops microbial contamination in the stomach and duodenum and helps relieve gastroduodenostasis. “Motility regulators” can be used as a means of restoring motility, and the drug of choice is Trimedat, which restores the tone of the CO and upper gastrointestinal tract.
The hydrogen test was carried out by department employees V. A. Loginov and M. A. Kruchinina.
Treatment of patients with the 4th variant of PCES
DSO, chronic biliary insufficiency, digestive disorder (mainly fats), duodenogastrostasis, intestinal functional disorder with a predominance of hyperkinesia.
The observed group consisted of 20 patients. The complex of drugs used: Duspatalin 600 mg/day (mebeverine hydrochloride, the advantage of which is a predominant effect on intestinal tone, without a significant effect on peristaltic activity); Ursosan - 500–750 mg/day; Pangrol is an enzyme preparation containing 10,000 and 25,000 IU of lipase (we used 25,000 × 3 times per meal). Normalization of intestinal microflora, sufficient enzyme and “bile acid replacement” led to the restoration of pressure in the stomach and duodenum and the restoration of CO tone. Subsequently, maintenance treatment with UDCA and enzyme preparations should be permanent. This eliminates risk factors for DSO and prevents recurrence of pain in the epigastrium and right hypochondrium. A sufficient maintenance dose of Pangrol is 10,000 units, and Ursosan is 500 mg/day with the development of the rhythm of administration.
Treatment of patients with the 5th variant of PCES
DSO, duodenogastrostasis, reflux gastritis.
There were 20 patients under our supervision. This option, in addition to the accepted examinations, requires studying the acid-producing function of the stomach (endoscopic pH-metry is sufficient) and, if hypersecretion is established, introducing it into a treatment complex that includes motility regulators Trimedat, Itomed, Ursosan, and also gastric secretion blockers. The basic drug in this situation is Ursosan, which, on the one hand, compensates for the lack of bile acids, and on the other, converts the synthesis of bile acids to increase the production of non-toxic ones, since the main damaging factors are bile acids, lysolecithin and pancreatic enzymes thrown into the stomach. The effect of treatment (elimination of pain and gastric dyspepsia is recorded by the end of the 1st week of treatment). UDCA drugs are used as maintenance therapy.
General conclusion
We must agree with the conclusion of the Rome Consensus II and III that the development of PCES is based on dysfunction of the sphincter of Oddi. The basis of this dysfunction is the removal of the gallbladder, an organ that is very important functionally. Surgical errors in the operation can hardly be the basis of PCES, since they are not directly related to dysfunction of the CO, which maintains the pressure gradient and normal passage of bile through the ductal system. Also, diseases that developed before surgery are not directly related to this.
Our materials show that there are several variants of PCES (we have identified 5), and they are formed as a result of various functional disorders that directly or indirectly lead to disruption of bile passage (gastroduodenostasis, indigestion, dyskinesia, intestinal dysfunction, SIBO, reflux gastritis). These disorders are risk factors for DSO and its maintenance. The therapeutic approach and the choice of pharmacotherapy that most adequately relieves the exacerbation of PCES depends on their presence.
Essentially, work on studying the therapeutic approaches of PCES and treatment has just begun, it needs to be continued and intensified with the hope of obtaining the desired effect.
Literature
- Malle-Guy P., Kestels P. J. Syndrome after cholecystectomy. M., 1973.
- Lazebnik L. B., Konanev M. I., Ezhova T. B. Comparative study of the quality of life in patients with cholelithiasis and postcholecystectomy syndrome. Materials of the 5th Slavic-Baltic Scientific Forum, St. Petersburg, Gastro-2003, p. 93.
- Kovalev A.I., Sokolov A.A., Akkuratova A.Yu. Postcholecystectomy syndrome: causes. Tactics of surgical treatment // News of surgery. 2011, vol. 19, no. 1, p. 20–21.
- Ilchenko A. A. Why does cholecystectomy not always improve the quality of life? // Pharmateka. 2012, 17, p. 23–29.
- Zimmerman Ya. S., Kuisman T. G. Postcholecystectomy syndrome: a modern view of the problem // Clinical medicine. 2006, no. 8, pp. 4–11.
- Sheptulin A. A. Roman criteria for functional disorders of the gallbladder and sphincter of Oddi: controversial and unresolved issues // Russian Journal of Gastroenterology, Hepatology, Coloproctology. 2005, No. 4, p. 70–74.
- Zvintseva T. D., Shargorod I. I. Postcholecystectomy syndrome: dysfunction of the sphincter of Oddi // Faces of Ukraine. 2011, no. 2, p. 100–106.
- Minushkin O. N., Maksimov V. A. Biliary-hepatic dysfunction. Toolkit. M., 2008.
- Minushkin O. N. Use of the drug “Odeston” in clinical practice, M., 2014.
- Vetshev P. S., Shkrob O. S., Beltsevich D. G. Cholelithiasis. M., 1998.
- Sokolov L.K., Minushkin O.N., Savrastov V.M., Ternovoy S.K. Clinical and instrumental diagnosis of diseases of the hepatopancreatoduodenal zone. M., 1987.
- Maksimov V. A. et al. Biliary insufficiency. M., 2008. P. 232.
O. N. Minushkin, Doctor of Medical Sciences, Professor
FSBI UMTS UDP RF, Moscow
Contact Information
Diagnostics
Patients with complaints of heaviness in the hypochondrium are examined by a gastroenterologist, who, if necessary, gives a referral to specialized specialists (hepatologist, oncohematologist). During the initial examination, the doctor palpates the liver and spleen, determines their size, and examines the skin for the presence of jaundice, spider veins, and dilated superficial vessels. A full diagnostic complex is prescribed, which includes:
- Ultrasound of the liver.
With an ultrasound examination, the doctor evaluates the size and structure of the organ parenchyma, identifies focal processes (cysts, abscesses, tumors), and detects signs of hepatitis or fibrous changes. The scan is complemented by Doppler ultrasound to check blood flow in the hepatic vessels. - ERCP.
Endoscopic examination is recommended for a comprehensive diagnosis of the state of the biliary system, finding stones, and deformations of the organ. To assess the contractile function of the bladder and obtain a bile sample for analysis, fractional duodenal intubation is performed. - Radiography.
On a survey image of the abdominal cavity, hepatosplenomegaly and displacement of neighboring organs are possible. To exclude damage to the respiratory system as the cause of heaviness in the hypochondrium, a chest x-ray is performed in two projections. - Biopsy of liver tissue.
Based on the results of histological analysis of biopsy specimens, the doctor differentiates benign and malignant neoplasms and establishes a diagnosis of parasitic infestations. The method is informative for assessing the prevalence of fibrosis and diagnosing autoimmune hepatitis. - Laboratory methods
. In a biochemical blood test for liver pathologies accompanied by heaviness in the hypochondrium, the content of cytolysis enzymes (ALT and AST) increases and the levels of bilirubin and cholesterol increase. To confirm infectious hepatitis, ELISA and PCR are performed. Hematological problems are excluded based on hemogram and coagulogram data.
In modern hepatology, static scintigraphy is used to clarify the diagnosis and assess the functional activity of the liver. Elastography is a widely used non-invasive method for studying the degree of fibrosis of the liver parenchyma. To identify a tumor process of the spleen or liver, MSCT of the abdominal organs is informative. In difficult situations, doctors resort to diagnostic laparoscopy.
Ultrasound of the liver
Does the liver hurt with hepatitis C?
The organ does not contain pain nerve endings. The development of pain in the localized area (right hypochondrium) is a consequence of stretching of the organ capsule. The capsule (Glissonian capsule) contains nerve endings. The pain develops as a result of its stretching, which develops due to the enlargement of the organ during the inflammatory process. Pain can also be the result of a pathological process in the structures of the hepatobiliary system (gallbladder and bile ducts), in particular inflammation and the presence of stones in it.
Treatment
Help before diagnosis
To reduce discomfort, patients are advised to follow a diet. Fatty and spicy foods, smoked foods, and spices are excluded from the diet. The best ways to prepare food are steaming, stewing, baking in the oven. Alcohol consumption is prohibited. Self-administration of medications is unacceptable, since heaviness in the hypochondrium has hundreds of causes that must be diagnosed and treated by a specialist.
Conservative therapy
If there is heaviness in the hypochondrium, etiotropic and pathogenetic medications are selected for the underlying disease that caused the symptom. Treatment is carried out on an outpatient basis, but during the period of exacerbation of chronic pathology, it is recommended to undergo a course of inpatient therapy. As a rule, the following groups of drugs are used:
- Choleretic agents
. Improving the outflow of bile during its stagnation quickly eliminates heaviness and discomfort in the right side and eliminates dyspeptic disorders. Medicines of the group of choleretics and cholekinetics, medicinal mineral waters are used. - Antibiotics
. Indicated for exacerbation of inflammatory processes in the hepatobiliary zone in order to prevent purulent complications. For infectious cysts, specific antiparasitic drugs are needed. - Antiviral drugs
. Prescribed to patients with chronic viral hepatitis to reduce the number of copies of the pathogen in the blood and prevent complications. For effective treatment, long courses are selected (at least 3 months). - Hepatoprotectors
. They protect the liver from damage by toxins and free radicals, improve the functional activity of the organ and promote cell regeneration. Usually they complement the main treatment of the pathology that caused heaviness under the right ribs. - Anti-inflammatory drugs
. Nonsteroidal anti-inflammatory drugs are used to eliminate discomfort and pain in the hypochondrium. Glucocorticoids quickly relieve autoimmune conditions that lead to the development of hepatomegaly or splenomegaly.
To eliminate signs of inflammation and reduce subjective symptoms, physiotherapy is performed. In chronic cholecystitis, UHF, inductothermy, and the administration of drugs to the affected area by electrophoresis show a good effect. To reduce the manifestations of gastric dyskinesia, diadynamic therapy, low-frequency pulsed currents, and SMT therapy are effective.
Surgery
In the calculous form of cholecystitis, a planned laparoscopic cholecystectomy is performed to prevent an attack of biliary colic. Impaired outflow through the hepatic or splenic veins is an indication for the application of artificial anastomoses to restore blood flow. For echinococcal cysts, surgical excision of the space-occupying lesion or endoscopic drainage is prescribed. In case of tumor processes, the volume of intervention is determined taking into account the degree of their benignity and spread.
Where does the liver hurt with hepatitis?
The word hepatitis refers to an inflammatory process that develops as a result of damage to liver cells (hepatocytes). A number of reasons lead to the inflammatory reaction of the organ, one of which is the C virus, which parasitizes the genome (genetic material) of hepatocytes. This process may be accompanied by the development of pain, its localization is in the area of the right hypochondrium (upper abdomen under the costal arch on the right). Therefore, the answer to the question whether the liver can hurt is negative, since the tissues of the organ do not contain sensitive nerve endings.
Signs of liver problems
We have found out where a person’s liver is located and how it hurts; now we should talk about the symptoms. Liver diseases manifest themselves in different ways. There are external and internal symptoms of liver disease. Let's take a closer look at each group.
External manifestations
- The appearance of spider veins
. Spider veins are a pronounced capillary network of dilated small vessels located in the superficial layers of the skin. This symptom is characteristic of serious liver dysfunction associated with intoxication, viral and alcoholic hepatitis, and cirrhosis. Spider veins most often appear on the lower torso, but sometimes appear on the cheeks and back. - Changes in pigmentation of the skin and mucous membranes
. With liver diseases, regardless of the cause, a person experiences jaundice syndrome. For example, in the acute form of hepatitis, the skin acquires a yellowish tint already 2–3 days after the onset of the disease. The color of the mucous membranes may change even earlier. This occurs due to the fact that the concentration of liver pigment fractions (bilirubin) greatly increases in the blood of an infected person. - Change in color of palms and soles
. A symptom of liver disease is also pronounced pigmentation in places of physiological folds. As a rule, it has a bronze or smoky tint. - Hair loss
. Accelerated hair loss is often observed with liver disease. The liver processes almost all nutrients that enter the body. If liver function suffers, then the body’s supply of “building materials” for growing tissues also suffers. For example, wounds heal more slowly or hair may fall out faster. - The appearance of a rash
. Along with changes in skin color, rashes appear in liver diseases. They can be of a very different nature. Pustular elements (folliculitis and furunculosis) are caused by an immune imbalance due to a decrease in the liver’s ability to synthesize immunoglobulin. An allergic rash (papules and spots) occurs due to a violation of the detoxification function of the liver. This reaction is triggered even to familiar environmental conditions. Hemorrhagic rash (small hemorrhages on the surface of the skin) appears when the synthetic function of the liver decreases. Patients have an increased tendency to form hematomas (“bruises”) even with minor injuries.
Internal manifestations
- Asthenia
. It is characterized by general weakness and lethargy, drowsiness, fatigue, and decreased performance. These symptoms are usually the first to appear when the liver is damaged. Their occurrence is due to the inability of the organ to completely neutralize the products of nitrogen metabolism, which affect the functioning of the brain. - Dyspepsia
. In case of liver diseases, dyspeptic manifestations may be observed in the form of belching, nausea and vomiting, diarrhea or constipation, a feeling of heaviness after eating, and bloating due to increased flatulence. Due to impaired digestion and absorption of fats, qualitative changes in stool occur. Steatorrhea (“fatty stools”) is observed. Any liver disease is usually accompanied by changes in peristalsis (motor activity of the intestines) and the secretion of intestinal glands. - Cytolysis.
The first sign of liver damage is cytolysis—the destruction of hepatocytes. When liver cells (hepatocytes) are destroyed, the level of enzymes such as ALT and AST increases in the blood. If these enzymes are elevated in a biochemical blood test, this indicates an inflammatory process in the liver tissue. - Increased body temperature
. Often, people with constant pain in the liver area experience a slight rise in temperature (up to 37.8 °C). With cirrhosis, thermometer readings can reach 38 °C. In some cases, fluctuations are observed throughout the day, but most often appear in the evening. A higher temperature (from 39 °C) is a symptom of purulent processes in the gallbladder or bile ducts and is not associated with liver disease. Accordingly, treatment is prescribed for another organ.
To learn more about the causes of pain in the liver area and what to do when it occurs, you should consult a specialist. He will conduct an examination, based on which a diagnosis will be made and treatment will be prescribed. In most cases, the main minimum recommendation from doctors is to avoid drinking alcohol and junk food.