Getting rid of cancer is the cherished dream of all cancer patients; most patients are willing to pay a high price for a long life after cancer. Few people assume that life after treatment will be different in terms of pathophysiological sensations.
After radical treatment of stomach cancer (successful, because surgery is not always possible), the patient is faced with a new problem in the first days. Before the operation, the doctor will tell you that most of the stomach with the tumor will be removed. Typically, three-quarters, or the entire stomach, is removed. With these quarters, the ability to eat three times a day as usual will go away, but the patient has not yet thought about this loss. After surgery, a condition may arise that makes it impossible not only to eat normally, but also to feel normal after eating. We are talking about post-resection syndrome, which appeared due to the removal of part of the stomach. The condition is also called dumping syndrome from the English “dumping” - reset.
What do surgeons do with the stomach?
Stomach surgery is a surgical technique that has been clearly tested on thousands of patients, allowing the removal of some part or the entire organ with minimal losses. The smallest losses when removing part of the stomach means maximum preservation of the anatomical and physiological path of movement and digestion of food masses. Depending on the location of the tumor in the stomach, subtotal distal and proximal resections are performed, and complete removal of the stomach - gastrectomy - is still often performed.
Treatment
If we talk about the mild stage, then a diet based on high-calorie foods and vitamins comes to the rescue. But fluid intake must be limited. The same prescription applies to carbon consumption.
If the syndrome manifests itself in a moderate form, it is recommended to take special medications that reduce intestinal dysfunction. General strengthening therapy plays a significant role.
The severe form of the syndrome with insufficient therapy requires surgical manipulation, the essence of which is the interposition of part of the intestine.
Billroth operations and gastrectomy
The first surgeon who not only removed a part of the stomach affected by cancer on January 29, 1881, but also came out of a patient after a serious operation, was the Austrian Christian Albert Theodor Billroth. Later he was invited to see the great surgeon Pirogov, who was dying of oral cancer, and he also operated on the poet Nekrasov. The most important gastric operations, used to this day, were developed by Billroth and bear his name.
Gastric resection according to Billroth I consists of connecting the remainder of the stomach with the duodenum “end-to-end”. This does not correspond to human nature, which has formed a tightly closed muscular junction between the stomach and intestines. Evacuation of food masses from the operated stomach occurs quickly, however, the stomach partially plays the role of a reservoir for food. The mucous membrane of the stomach does not come into contact with the mucous membrane of the small intestine, which protects the latter from chronic ulcerations.
During gastric resection according to Billroth II, the remaining part of the stomach is sutured side-to-side with the jejunum, and the duodenum is excluded from circulation, which is not at all physiological. Subtotal gastrectomy according to Billroth II is very common in oncology; surgical tactics are determined by the cancerous tumor. It is with this option that dumping syndrome often develops.
Gastrectomy - complete removal of the stomach - necessarily leads to dumping syndrome. The esophagus is connected to the intestine, there is no reservoir for temporary storage of food with simultaneous digestion, the role of which was regularly performed by the stomach, food immediately enters the intestine, which is not adapted to unprepared food masses.
Do not smoke.
Smoking after gastric bypass will cause stomach ulcers. Note that we do not say: may cause or increase risk.
If you smoke, you will get ulcers. It's a question of time.
Don't do this, at least for the sake of your stomach. And although the risk of gastric ulcers is not as acute after gastric banding, these patients should also give up this habit for the sake of overall improvement in health and quality of life.
Find out about the medications you are not allowed to take. One of the patients arrived at the clinic’s emergency department at 2 a.m., after her own wedding. Three years after the operation, she forgot about the ban on taking NSAIDs and took Ibuprofen for a couple of days before the wedding to combat a headache. As a result, on the first night of her honeymoon, she developed a stomach ulcer - and she spent her first night as a wife in a clinic, instead of lying in a jacuzzi in a luxury hotel room next to her young husband.
Remember this story - no matter how much time has passed since the operation, you will never be able to take certain medications.
Medicines that may be harmful to your stomach (do not take any medicines without talking to your doctor):
- Aspirin
- Voltaren
- Ibuprofen
- Indomethacin
- Ketoprofen
- Prednisolone
- Tetracycline
- Celebrex
- Erythromycin and others.
If you have any doubts about the safety of any medicine, do not hesitate to call your doctor. A phone call will take a couple of minutes, but can prevent very big problems.
Patients after gastric banding and gastroplasty may not be as strict about the list of approved medications, but after gastric banding, another problem arises - the size of medications. Large tablets - even those that are quite normal size - can get stuck. It is very good if patients bring medications with them to the consultation before surgery so that the surgeon can assess their actual size. In general, if your medicine has a liquid form, then it is better to choose that one. If there are no such forms, then perhaps the tablet can be broken or ground into powder, but remember that long-acting drugs cannot be broken.
A pharmacist at your pharmacy can help you choose the right replacement for your medication and can give you lots of helpful advice before surgery. Some clinics have a pharmacist who communicates with patients before surgery, but even if your clinic does not have such a specialist, do not despair, experienced pharmacists work in any pharmacy.
Manifestations of dumping syndrome
With stomach cancer, such pronounced biochemical disturbances occur in the patient’s body that even at the end of the last century, a quarter of patients died after surgery for unknown reasons. Today, the modern science of caring for postoperative patients has made it possible to forget about this sad quarter, however, the biochemical processes in the body of a gastric patient have not become smaller.
Rapid evacuation of food into the intestine leads to serious disturbances in biochemical processes, which affect the patient’s condition. A few minutes after eating, the patient literally becomes weak. The intensity of weakness is very different, from short-term and fundamentally not interfering with life and work, to a state of complete powerlessness.
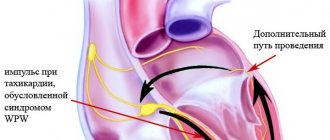
Weakness is accompanied by strong palpitations and even pain in the chest, but these are not anginal pains caused by impaired myocardial nutrition - ischemia, but cardialgia, that is, as if pain in the heart. But it's not the heart that really hurts. With true heart pain, it hurts behind the sternum, the pain radiates to the arm, shoulder, jaw. But in especially severe cases of dumping syndrome, transient changes such as myocardial ischemia are noted on the ECG.
There are surges in blood pressure. My hands are shaking, my head is spinning, my ears are ringing. The patient is pale or, on the contrary, his face turns red, and he almost always sweats profusely. There is often a urge to urinate. Worries include nausea and vomiting, abdominal pain, loud rumbling, belching, the urge to defecate, even diarrhea. The clinical picture is very varied, it is clear that the person is very ill, some require bed rest for a couple of hours after each meal.
The patient experiences fear, the symptoms are so unpleasant and varied. He may lose consciousness, which he does not always remember afterwards. Oddly enough, memories during dumping syndrome also do not always correspond to reality; amnesia after an attack is also possible. In this regard, they even identified an episodic variant, when the syndrome develops immediately after eating, accompanied by fear, which the patient does not remember well. The paroxysmal variant occurs a couple of hours after eating and leads to loss of consciousness and amnesia. And there is an objective biochemical reason for all this.
Possible complications
If the clinical picture of the syndrome is ignored for a long time, additional symptoms appear:
- Diseases of the gastrointestinal tract: peptic ulcer, enteritis, colitis, pancreatitis.
- Hypoglycemic conditions that provoke hormonal imbalance and the development of diabetes.
- Cachexia. The patient loses weight, which ultimately leads to significant weight loss and general exhaustion. Advanced pathology can lead to death.
Treatment of dumping syndrome without re-operation is possible provided emergency medication prescriptions are followed by an experienced specialist.
How often is dumping syndrome observed?
This picture can appear after each meal, but during breakfast it is more pronounced, at lunch it appears a little less, and at dinner even less. Symptoms may last a few minutes or may last up to three hours. This is not all, because the patient also experiences weakness the rest of the time, but not so intense, and over time, asthenia develops, including a decrease in potency.
The frequency of development of dumping syndrome is unknown, in the specialized literature different figures are indicated - from 10 to 80%, it all depends on how focused the team of authors who wrote the article is in treating it. If the authors of the article are involved in the treatment of post-resection complications, then the frequency is high - they specifically collect such patients. If the scientific material was prepared by surgeons, then a full statement of dumping syndrome in operated patients is far from ideal and real; as a rule, only a severe course is monitored.
In most cases, the syndrome is mild with partially blurred clinical signs; a severe course is typical for women who have undergone surgery. Again, it is not really known how many patients there are with a severe syndrome; options range from one to ten per hundred operated on. Some operated patients who experience weakness after eating do not even suspect the presence of mild dumping syndrome, which could be corrected if a diagnosis were made.
Symptoms
Dumping syndrome develops gradually and has the following symptoms:
- The appearance of weakness, fever, and a feeling of a full stomach after eating. This is how a mild form of pathology manifests itself, which develops after consuming milk or sweets.
- The average severity of this disease manifests itself as increased fatigue, decreased vision, sweating and drowsiness, hunger, and decreased performance. In the event of an attack, patients feel increased heart rate and tingling of the limbs, shortness of breath, rhinitis, diarrhea, and increased urination.
- In severe Dumping syndrome, patients suffer from incoordination of movements, tachycardia, increased sweating, clouded consciousness, hypertension, and collapse. Patients rapidly lose weight because they often refuse to eat, and the body becomes exhausted.
- In the interval between attacks, patients' memory and performance decrease, they are tormented by a state of depression and weakness, and there are regular mood swings from irritated to apathetic.
Consequences of Dumping syndrome:
- decreased quality of life;
- erosions and ulcers on the gastric mucosa;
- adhesions in the abdominal cavity;
- hypoglycemia and anemia;
- acid-base imbalance;
- chronic inflammation of the pancreas or intestines;
- hypovitaminosis and metabolic disorders;
- bile duct dyskinesia;
- anorexia and extreme exhaustion of the body;
- protein deficiency;
- loss of ability to work and social activity.
Why is it developing?
In the development of dumping syndrome, the leading role belongs to the rapid evacuation of food through what remains of the stomach, and the equally rapid filling of the jejunum with unprocessed food. Reflex signals from the jejunum swollen with food cause blood flow to the internal organs; on the periphery, the volume of circulating blood, on the contrary, decreases. The internal organs do not need blood in large quantities at all, so it is deposited, while the brain experiences real starvation.
Nutrients that enter the intestine without prior proper processing pass through the membranes of mucosal cells into the blood. In the experiment, stretching of the jejunum leads to the release of biologically active substances into the blood, mainly the “joy hormone” serotonin and acetylcholine. Hence weakness, palpitations, redness of the face and sweating, fluctuations in blood pressure.
An increase in the level of adrenaline secreted by the adrenal glands was detected, and the process of its secretion is triggered by the pituitary gland, which received information from the enterochromatophyte cells of the mucous membrane of the small intestine. These cells also stimulate the vomiting center of the brain. Stretching the intestine causes peristalsis - contraction of the intestines, which results in diarrhea, in which fluid, proteins and microelements are lost, which aggravates weakness and decreased blood pressure.
Rapid absorption of glucose in the jejunum disrupts metabolic processes in the pancreas, which releases more insulin into the blood than necessary. The concentration of sugar in the blood decreases below normal levels, which is also accompanied by severe weakness, hunger, and trembling. This mechanism is associated with delayed dumping syndrome, which develops a couple of hours after eating. Each patient develops all these pathophysiological changes to varying degrees, which ultimately lead to a decrease in the patient’s already low weight, the development of anemia and vitamin deficiencies, and most importantly, an uncomfortable life.
Alcohol.
Alcohol is not prohibited after surgery, but there are some things you should pay attention to.
First of all, after gastric bypass surgery, alcohol has a much stronger effect on a person, since it is absorbed much more efficiently and quickly. Even a small amount of alcohol can affect you much more than before the operation and the intoxication will last longer. This is very bad. Firstly, alcohol removes inhibitions - and we are not talking about the fact that you will dance on the table, but that you will not be able to resist dessert.
If the above does not impress you, then keep in mind: such an ultra-efficient process of alcohol absorption greatly increases its harmful effects on the body, primarily on the liver. Plus, you now weigh less, which further increases your risk of drunken accidents (car accidents and everything in between). If you could easily drive after a glass of wine with dinner before surgery, now do not do this under any circumstances.
Don't forget that alcohol is high in calories - just like the ingredients in traditional cocktails, tonic water or cola - making these drinks a killer concoction. All those extra calories can contribute to weight gain without providing any nutritional value. If you are on a low-calorie diet after surgery, every calorie you eat counts. It's very sad to see how 150 calories from a glass of beer replaces a normal meal that contains the nutrients your body needs.
Avoid drinking alcohol during the first year after surgery, it will also be beneficial from a psychological point of view. Often patients substitute their addictions. If you used to eat some of your feelings, now it is very important to learn to cope with them, and not replace food with another bad addiction.
Clinical picture
Patients are concerned about pain and heaviness in the right hypochondrium, accompanied by vomiting of bile, after which the pain decreases.
In mild cases, these phenomena occur once every 2 weeks, in moderate cases - 2-3 times a week, in severe cases - several times a day, while the amount of bile reaches 500 ml, which causes rapid exhaustion of the patient.
An objective examination can reveal asymmetry of the abdomen due to bulging of the right hypochondrium, which disappears after profuse vomiting. Sometimes there is a slight yellowing of the sclera. X-ray reveals an atonic adductor loop - a barium suspension can remain in it for up to 2 hours.