Some people are sure that cystitis occurs due to hypothermia, others believe that it is due to microbes. Both are simultaneously right and wrong. Because both conditions are important for the development of the disease: the presence of a pathogen and a decrease in the body’s defenses.
Medical expert at the laboratory of personalized medicine LabQuest Nadezhda Bezemskaya.
This disease is considered to be “female,” but in fact, everyone can get cystitis, regardless of gender and age. However, women actually experience this disease 8 times more often than men.
Profitable loyalty
There is an objective anatomical reason for the fact that cystitis is predominantly female. After all, in the fair sex, the urethra is much shorter and wider than the male one, so the path upward to the bladder for pathogenic microbes becomes shorter and easier. However, for a disease to occur, the penetration of microbial agents alone is not enough. After all, the protective forces of the bladder mucosa, guarded by beneficial lacto- and bifidobacteria, are usually sufficient to give a worthy rebuff to the infection. But if local immunity is weakened, then it’s a different matter. The protective forces of the mucous membrane can be negatively affected, for example, by hypothermia, injury, stress, excessive alcohol intake, promiscuous sex life, poor intimate hygiene, chronic diseases, etc.
By the way, frequent changes of sexual partners for women (and especially young girls with unsettled hormonal levels and not fully formed intimate microflora) are even more harmful than for men. And we’re not just talking about sexually transmitted diseases. After all, the female intimate flora is forced to adapt to the partner’s flora each time (after all, men’s intimate organs normally contain streptococci and other opportunistic flora). At some point, the adaptation process may be disrupted, and then the female microflora will suffer, and against this background, candidiasis, cystitis, and other troubles may arise. Therefore, it is especially important for girls to remain faithful to their only sexual partners, and it is better for very young ladies not to rush into “adult” life.
Not to the pharmacist, but to the doctor!
When customers at a pharmacy ask a pharmacist to sell them “something for cystitis,” they often do not understand that they are doing it to their detriment. After all, this disease (if it really is one) can be different. For example, cystitis can be primary and secondary (that is, arising on its own or as a result of another disease). It can also be infectious and non-infectious. In one case, it is caused by microbes, and in another, inflammation of the bladder mucosa may be associated, for example, with allergies, medications, chemical or thermal damage. In addition, cystitis can be acute and chronic.
In each of these cases, treatment must be strictly individual. And even infectious cystitis can be treated with different drugs, depending on the microbe that caused the infection. An incorrectly chosen medicine or an incorrectly selected dose will lead, at a minimum, to ineffective treatment, and at maximum, to the development of antibiotic resistance in microbes. For this reason, it will be extremely difficult to subsequently cope with microbial inflammation. In addition, such pseudo-treatment can transform acute cystitis into chronic, which is much more difficult and expensive to identify and treat. Therefore, the first rule for cystitis is no self-medication!
Etiology
The causative agent of acute uncomplicated cystitis in most cases (about 80–90%) is Escherichia coli
and much less often - other pathogens of urinary infection:
Staphylococcus saprophyticus, Klebsiella spp., Proteus spp.
and others [4].
Currently, multicenter clinical studies are regularly conducted around the world to monitor UTI pathogens and their antibiotic resistance. The largest international study, ECO-SENS, involving 4,734 patients from 252 clinics in 16 countries in Europe and Canada, which ended in 2003, revealed the following patterns: in 77.7% of patients, UTIs were caused by E. coli
, in 5.2% -
Proteus mirabilis
, in 2.8% -
Klebsiella spp
., in 3.9% - other representatives of the
Enterobacteriaceae
, in 4.6% -
S. saprophyticus
and in 5.8% - other microorganisms.
29.8% of the isolated strains of microorganisms were insensitive to ampicillin, 29.1% to sulfamethoxazole, and 14.8% to trimethoprim. E. coli
strains to ciprofloxacin, the combination of amoxicillin and clavulanic acid, nitrofurantoin, gentamicin and fosfomycin trometamol was observed in less than 3% of patients [5].
In Russia, under the leadership of Professor L.S. Strachunsky, similar studies were conducted: UTIAP I (1998–1999), UTIAP II (2000–2001) and UTIAP III (2004–2005). During these studies, it was found that in Russia, acute cystitis was caused by E. coli
, in 6% -
Klebsiella spp
., in 1.8% -
Proteus spp.,
in 1.6% -
S. saprophyticus
, in 1.2% -
Pseudomonas aeruginosa
etc.
E. coli
resistant to ampicillin were found in 22.7-44% of cases, to co-trimoxazole - in 16.2-26.9%, to nitroxoline - in 6.8-7.9% of cases.
Resistance of E. coli
to norfloxacin, ciprofloxacin and nitrofurantoin was noted in less than 3% of patients with acute cystitis [6, 7].
The multicenter study "DARMIS-2011" showed that among the causative agents of UTIs, the proportion of representatives of the family Enterobacteriaceae
amounted to 83.5%.
At the same time, E. coli
was detected in 63.5% of patients.
In general, the frequency of pathogen isolation did not differ significantly between patients with complicated and uncomplicated UTIs [8]. In the DARMIS-2018 study, the detection rate of E. coli
in the group of patients with uncomplicated infection was 74.6%, complicated - 67.2%,
Klebsiella pneumoniae
- 9.6% and 12.7%;
P. mirabilis -
3% and 4.6%;
Enterococcus faecalis -
5% and 6.3%;
Staphylococcus spp.
— 2.3% and 1.2%, respectively;
the proportion of P. aeruginosa
that was detected in complicated UTIs was 1.7%.
E. coli
strains to ampicillin (57.7%), amoxicillin/clavulanate (43%) and trimethoprim/sulfamethoxazole (36.9%) was recorded; a decrease in sensitivity to ciprofloxacin (60.6%) was also noted, which was significantly lower than 7 years ago (79.9%). Compared with the previous study, according to DARMIS-18, the number of pathogenic microorganisms producing extended spectrum β-lactamases increased statistically significantly - from 8.5% to 27% [8].
Doesn't tolerate delay
The symptoms of acute cystitis are known to everyone: pain in the lower abdomen, frequent painful urination, sometimes even blood in the urine. There are also severe pains that radiate to the anus or perineum. If, in such a situation, you immediately contact a therapist and quickly get tested to confirm the diagnosis, and then begin antibacterial treatment, then within a week you can forget about the disease.
If you delay visiting a doctor, then after 14 days acute cystitis will turn into a chronic form, which can occur with mild symptoms: that is, without severe pain and significant discomfort. And those minor ailments that may occur, many patients courageously endure. Sometimes - for years. Even establishing the correct diagnosis in this case is a big problem, and even more so getting cured. The danger is also that prolonged inflammation in chronic cystitis can eventually lead to cell degeneration and the development of bladder cancer. Therefore, you should go to the doctor as soon as you feel sick, and not sometime later, when there is a rush at work. Or when it gets easier.
Before and after tests
According to standards, treatment of cystitis with antibiotics is prescribed immediately. Before treatment, only a general urine test is required to detect signs of inflammation. And if it is not possible to take it to the laboratory, you can use an express test strip. Next, antibiotics are prescribed. In more than 80% of cases, cystitis is caused by the bacterium E. coli, or Escherichia coli. But opportunistic bacteria (Klebsiella, ureoplasma, streptococcus, staphylococcus) can also be causative agents. They themselves do not cause the disease, but weaken the body’s immune defense, and against this background pathological flora - fungi, bacteria - joins.
And after a course of antibacterial therapy, it is recommended to do a bacterial culture of the urine to make sure that there is no causative agent of the disease, which means that the infection has been cured.
Treating cystitis with folk remedies is less effective than antibiotics. Therefore, warm heating pads, herbs and cranberry juice are best used only in addition to treatment. And also only with the permission of a doctor, because any drugs, even herbal ones, can cause allergies or have individual intolerance. However, medicine knows cases of spontaneous healing of cystitis, when a strong immune system managed to cope with the inflammation on its own. However, playing “roulette” with a disease is quite dangerous, especially if there are effective medications.
Treatment with folk remedies for cystitis
When undergoing a course of treatment for cystitis with tablets prescribed by a doctor, you can use folk remedies as an auxiliary therapy.
Any treatment for cystitis, both tablets and folk remedies, must be prescribed by a doctor. Even harmless, at first glance, techniques should not be used independently, without consultation. This can only worsen the course of the disease.
There are several traditional methods for treating cystitis that are easy to use at home. At the same time, they have a good effect. Here are the most popular and proven:
- Every day, drink a decoction of dill seeds, which has an analgesic effect and relieves symptoms of inflammation. You can make an infusion of dill by pouring boiling water over the crushed seeds. People with low blood pressure and gallbladder pathologies should not drink dill decoction and infusion.
- Regular millet has a good effect in treating cystitis. To prepare the drink, pour 2 tablespoons of millet into 2 cups of boiled water, then boil for another 5 minutes. Leave the decoction for 5 minutes, drain the water, drink a tablespoon of the decoction every day during the first day of illness, on the second day increase the dose to 3 tablespoons every hour, on the third day drink half a glass every hour. Cystitis can be treated with this remedy for up to 7 days.
- A decoction of chamomile also has a positive effect on cystitis. To prepare it, you need to pour 1 tablespoon of flowers with a glass of boiling water and leave for a quarter of an hour. Drink a third of a glass three times a day, on the eve of meals. Medicinal chamomile is not only a traditional medicine; it is included in many drugs, dietary supplements, and is used in homeopathy.
- Regular parsley effectively treats cystitis. Prepare an infusion from the seeds, pour a teaspoon of crushed seeds into two glasses of cool water. Leave the product for 10 hours. Then throughout the day, drink the infusion in small sips. You can eat parsley seeds without preparing an infusion, only before doing so they must be thoroughly chopped.
- Very good results can be achieved by drinking tea and infusions from lingonberry leaves. To prepare the infusion, you need to pour a tablespoon of lingonberry leaves into a glass of boiling water, leave the product for an hour, and then drink half a glass of it three times a day.
- You can treat cystitis with soda. Dissolve a tablespoon of soda in a liter of boiled water. Drink this solution one tablespoon three times a day. With this product you can wash the perineum and douche the urinary tract, and, if necessary, the vagina.
Cystitis is often treated with homeopathic remedies. They should also be prescribed by a doctor specializing in homeopathy and monitor the therapy process.
It's time to start an investigation
But sometimes even treatment according to all the rules does not help. Therefore, if cystitis has not gone away within 7 days, it is necessary to undergo further examination, and, perhaps, begin to actively look for concomitant diseases. Among them may be, for example, other diseases of the genitourinary system (such as colpitis, bacterial vaginosis, pyelonephritis, urolithiasis, prostatitis in men), as well as genital infections (trichomoniasis, chlamydia). Patients with diabetes mellitus are also predisposed to cystitis (“sweet” urine promotes the growth of bacteria).
To identify the circle of “suspects,” the doctor must collect an anamnesis. And for this, you need to find out whether cystitis occurred for the first time or not, whether there was hypothermia before the exacerbation, whether all this was preceded by unprotected sex, whether the patient underwent aggressive treatment (chemotherapy, radiation therapy), whether he took medications and what kind, etc.
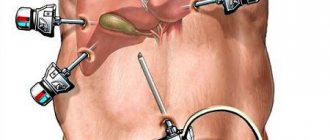
Depending on this, the doctor can refer the patient to a gynecologist and urologist, and also prescribe a list of necessary studies. As a rule, for chronic cystitis, the following are necessary: ultrasound of the pelvic organs and invasive cystoscopy (a tube with light is inserted into the urethra, and the condition of the mucous membrane is assessed).
Among the tests, you may need a urine sample according to Nechiporenko (helps to exclude or confirm the diagnosis of “pyelonephritis”) and the so-called two-glass urine sample (needed to make a differential diagnosis between cystitis and urethritis).
Along the beaten track
Judging by statistics, every second woman after the first episode of the disease develops a relapse within a year. And half of them have exacerbations more than 3 times a year. This happens because the initial treatment of acute cystitis was incorrect, and also because, when faced with a new case of the disease, many women, out of habit, take the medicine that helped them the last time. This is a huge mistake! The class of antibiotic must be changed, otherwise harmful bacteria, a small part of which could remain in the bladder, will develop resistance to the drug, and this will lead to the drug no longer working, and cystitis itself becoming chronic.
Therefore, a good doctor, before prescribing an antibacterial medicine, will definitely ask the patient how long ago and what kind of antibiotic he recently took.
BY THE WAY
In the West, cystitis is an inflammatory disease of the bladder and urethra. And in Russia, the disease is divided into cystitis and urethritis. In the first case we are talking about inflammation of the bladder, in the second – about inflammation of the urethra. And although these are details, we will adhere to the domestic view of the disease.
Services and diseases
Cystitis is an infectious and inflammatory disease of the bladder wall with primary damage to its mucous membrane.
Epidemiology. Women get sick more often than men, in a ratio of 3:1, which is due to:
- anatomical and physiological features of the female genitourinary system (short and wide urethra, proximity of the genital tract and rectum)
- gynecological diseases
- changes in hormonal levels during pregnancy, when taking hormonal contraceptives, in the postmenopausal period (microcirculation disorders leading to weakening of local immunity, atrophy of the vaginal mucosa, decreased mucus formation)
Cystitis is an infectious and inflammatory disease of the bladder wall with primary damage to its mucous membrane.
Epidemiology. Women get sick more often than men, in a ratio of 3:1, which is due to:
- anatomical and physiological features of the female genitourinary system (short and wide urethra, proximity of the genital tract and rectum)
- gynecological diseases
- changes in hormonal levels during pregnancy, when taking hormonal contraceptives, in the postmenopausal period (microcirculation disorders leading to weakening of local immunity, atrophy of the vaginal mucosa, decreased mucus formation)
In men, this disease is much less common and can be caused by inflammatory processes in the prostate gland, seminal vesicles, epididymis and urethra. A common cause of secondary cystitis in men is bladder outlet obstruction with chronic urinary retention as a result of urethral strictures and tumor diseases of the prostate gland.
Etiology and pathogenesis. The most common cause of cystitis is a bacterial infection. In addition, the causative agents of the disease can be viruses, mycoplasmas, chlamydia, and fungi. Most often, in patients with cystitis, Escherichia coli, Staphylococcus, Enterobacter, Proteus, Pseudomonas aeruginosa, and Klebsiella are detected in the urine. The leading microbial pathogen in acute cystitis is Escherichia coli (80–90% of observations), which is explained by the high pathogenic and adaptive capabilities of this microorganism (adhesion phenomenon, high reproduction rate, production of ammonia, which weakens the immune system and disrupts the function of smooth muscle fibers of the urinary tract).
Symptoms and clinical course. Acute cystitis is characterized by a sudden, violent onset caused by some provoking factor (hypothermia, endoscopic intervention, trauma), and rapid regression in the case of timely prescribed therapy. The severity of symptoms increases during the first two days.
Patients complain of frequent painful urination, pain in the lower abdomen and the appearance of blood at the end of urination (terminal hematuria). The inflammatory reaction and swelling of the bladder wall are accompanied by irritation of the nerve endings. Even a slight accumulation of urine causes the muscular wall of the bladder to contract, and the patient feels a very strong urge to urinate. The more pronounced the pathological process, the shorter the intervals between urinations. In severe cases, this time period is reduced to 15–20 minutes, which is extremely exhausting for the patient. Urgent urinary incontinence is characteristic, that is, the imperative (imperative) urge to urinate is so strong that the patient loses urine before reaching the toilet.
Cystitis is accompanied by pain in the bladder and perineum area of varying degrees of intensity. The pain syndrome is characterized by constancy, which disrupts a person’s usual life activities and rest, since it does not stop at night.
Terminal hematuria is also a very characteristic sign of the disease. It appears at the end of urination in the form of a clearly visible impurity or even drops of blood. Urine with cystitis loses transparency due to the presence of a large number of microorganisms, blood cells, epithelial cells and salts. It becomes cloudy and acquires an unpleasant odor.
There is no increase in temperature during cystitis, which is due to the reduced ability of the bladder wall to absorb substances, including inflammatory toxins. Normally, this mechanism prevents the products of nitrogen metabolism from concentrated urine from entering the blood.
Severe forms of acute cystitis – phlegmonous, gangrenous, hemorrhagic, ulcerative – occur extremely rarely. They are characterized by severe intoxication, high body temperature, and oliguria.
A recurrent course of acute cystitis is said to occur when symptoms of the disease appear at least twice in six months or three times in a year. The cause of cystitis in this case is reinfection, that is, repeated infection with pathogenic microflora, the source of which is both a nearby focus of chronic infection and a sexual partner. Also, the risk of relapse is increased by interrupted treatment, uncontrolled use of antibiotics and failure to comply with personal hygiene rules.
Chronic cystitis , as a rule, is a consequence of a previous inflammatory or predisposing disease and is secondary in nature. Inflammation of the bladder develops and is maintained as a result of:
- bladder outlet obstruction (sclerotic changes in the bladder neck, benign hyperplasia, prostate cancer, narrowing of the urethra, phimosis)
- UCD (bladder stones)
- bladder tumors
- bladder diverticula
In the absence of the above pathological conditions and chronic cystitis resistant to therapy, it is necessary to exclude specific diseases, primarily genitourinary tuberculosis.
The clinical symptoms of chronic cystitis repeat those of the acute form. The difference lies only in the degree of their expression. The course of the disease is characterized by periodic exacerbations, which are clinically very similar to acute cystitis and are treated in the same way. A stable course of chronic cystitis with a minimal set of complaints and constant laboratory signs, such as leukocyturia and bacteriuria, is also possible.
Diagnostics. The rapid onset of the disease with characteristic symptoms allows one to immediately suspect acute cystitis. As a rule, no pathological changes are observed in clinical and biochemical blood tests.
Urine is cloudy and has an odor. When examined, its reaction is often alkaline, a large number of leukocytes and bacteria are always determined, red blood cells, epithelium, cylinders may be present, and false proteinuria is noted, that is, caused by the breakdown of a large number of blood cells.
Bacterioscopy allows you to visually (using a microscope) determine the presence of an infectious pathogen. Urine culture with determination of bacterial culture and antibiotic sensitivity test is more informative. The disadvantage of this method is the duration of its implementation, therefore, with a clinically confirmed diagnosis of cystitis, antibacterial therapy with broad-spectrum drugs is started without waiting for culture results.
It is important to note that in acute cystitis, invasive diagnostic methods, primarily cystoscopy, are contraindicated.
Firstly, this procedure does not provide significant information, secondly, in the presence of acute inflammation it is extremely painful and, thirdly, it can lead to reinfection and/or aggravate the course of the infectious process. Cystoscopy is possible and indicated for chronic cystitis; it can be used to identify areas of hyperemia, pronounced vascular patterns, fibrinous deposits, ulcers, leukoplakia, stones, etc.
Differential diagnosis. In acute cystitis, the diagnosis is usually beyond doubt. Chronic cystitis, especially in cases where there are no characteristic clinical symptoms and treatment is ineffective, should be differentiated primarily from tuberculosis and bladder tumors.
Distinctive signs of tuberculous cystitis are the acidic reaction of urine and the absence of microbial growth when inoculated on ordinary media. Repeated microscopy of urine sediment for Mycobacterium tuberculosis and its inoculation on special media are necessary. The most characteristic sign of bladder tumors is total painless gross hematuria. The diagnosis can be made by sonography, CT and cystoscopy with a biopsy of the bladder wall.
Treatment. Therapeutic tactics for acute cystitis include prescribing antibacterial therapy; rest, plenty of fluids, and warmth in the lower abdomen are recommended; spicy and extractive foods are excluded from the diet. Currently, there are a number of effective antibiotic treatment depending on the duration of use: a single dose, three-day and seven-day courses. The clinical effectiveness of short-term courses of treatment for women of reproductive age has been proven.
The best single-use drug is fosfomycin (monural). This is a broad-spectrum antibiotic, effective against Escherichia coli, Staphylococcus, Proteus, Pseudomonas aeruginosa, Klebsiella, etc. The resistance of microflora to this drug is insignificant. In the treatment of uncomplicated cystitis, a single dose of 3 g of fosfomycin is indicated, the effect of which lasts for 5 days. Its use is justified for bacteriuria in pregnant women, as well as as a prophylaxis before invasive studies (cystoscopy) and surgical interventions. A single dose of levofloxacin at a dose of 250 mg also has a good effect; cure after it reached 95% of patients.
A longer course of antibiotic therapy is indicated for the treatment of cystitis in patients with risk factors for recurrent and chronic infection. These include:
- acute cystitis in men
- cystitis in women over 65 years of age
- persistence of clinical symptoms for more than 7 days
- pregnancy
- diabetes mellitus and other metabolic disorders
- use of diaphragms and spermicides
For these patients, it is most appropriate to prescribe fluoroquinolones, 3rd and 4th generation cephalosporins and protected penicillins.
From the point of view of the combination of such qualities of drugs as effectiveness, low cost and low probability of relapse, fluoroquinolones are currently the drugs of choice. Having a wide spectrum of action and having been present on the pharmacological market for quite a long time, they are still characterized by the lowest level of microflora resistance. From this group, ciprofloxacin, levofloxacin, norfloxacin and ofloxacin are usually prescribed. A standard seven-day course of these drugs allows you to completely relieve the symptoms of cystitis and eliminate the pathogen.
Cephalosporins have worked well in the treatment of urinary tract infections. They are highly effective against almost all gram-negative (Proteus, Klebsiella, Enterobacter) bacteria, including nosocomial strains resistant to many antibiotics, and many gram-positive (staphylococci, streptococci) microorganisms.
Semi-synthetic penicillins (Augmentin, Amoxiclav) contain clavulanic acid, which neutralizes the enzymatic defense of gram-positive bacteria.
In addition to antibiotics, the positive effect of uroantiseptics . Representatives of this group are nitrofurantoin (furadonin) and furazidin (furagin).
Symptomatic therapy. Pain can be relieved by prescribing nonsteroidal anti-inflammatory drugs that have anti-inflammatory and analgesic effects (solpadeine, diclofenac, lornoxicam, etc.). Antispasmodics include no-spa, baralgin, cystenal, platifillin, etc.
The criteria for cure of cystitis are the complete absence of clinical symptoms, the absence of leukocyturia and the growth of bacterial colonies in urine culture after the end of antibacterial therapy. You should take a control general analysis and urine culture for microflora at least a week after stopping antibiotics.
Treatment of chronic cystitis is more complex and lengthy. Therapy consists of taking antibiotics for 7–14 days, and sometimes several weeks. It is especially important to eliminate the cause of the chronic infectious-inflammatory process, to sanitize foci of chronic infection and correct the immunodeficiency state.
In the prevention of cystitis, compliance with the rules of personal hygiene, timely treatment of inflammatory diseases and urodynamic disorders, prevention of hypothermia, and adherence to asepsis during endovesical examinations and bladder catheterization play an important role.