Unpleasant in appearance and bitter in taste, bile was perceived by many peoples in the past as the cause of a person’s bad character. There is indeed some truth in this: diseases of the gallbladder may well poison the life of a person and everyone around him at the same time. But under normal conditions, bile performs a number of important functions in the body, most of which are related to digestion.
It is this that creates an environment in the intestine that is favorable for pancreatic enzymes. With its help, cholesterol, bilirubin and a number of other substances that are not filtered by the kidneys are removed from the body. It activates enzymes necessary for the digestion of proteins. The acids it contains break down fats...
Bile is produced in the liver, some of it accumulates in the gallbladder. When a person eats, bile from the liver and gallbladder flows through the ducts into the small intestine. But sometimes problems arise with the evacuation of bile - it stagnates in the gallbladder. As a result, an inflammatory process develops in this organ - cholecystitis.
The causes of inflammation can be different, but the most common is the presence of stones in the gallbladder. Doctors call this form of the disease calculous cholecystitis. This is one of the types of gallstone disease.
Chronic calculous cholecystitis
Gallstones are a constant source of inflammation. But in the chronic stage this process is weakly expressed, the disease only periodically makes itself felt.
Manifestations of chronic calculous cholecystitis: frequent aching pain in the right hypochondrium;
- paroxysmal pain that occurs after eating fatty, salty or fried foods;
- nausea and belching with a bitter aftertaste;
- isolated attacks of vomiting with bile.
However, at this stage of the disease, the symptoms may be so mild that they are not perceived as signs of severe pathology. The patient may regularly experience “just” a feeling of heaviness in the right side, suffer from flatulence, diarrhea, heartburn, belching, feel bitterness in the mouth...
At times, chronic calculous cholecystitis is manifested by attacks of hepatic colic. In this case, there is severe stabbing pain in the right hypochondrium, which is sometimes accompanied by vomiting. During an attack, the tongue becomes dry and the stomach is tense. However, a blood test does not reveal any abnormalities, and the gallbladder and liver are not enlarged.
An attack of colic can last from several minutes to several hours.
Diagnostics
Diagnosis of cholelithiasis is based on the clinical picture, as well as data obtained during an instrumental examination. To make a diagnosis with sufficient accuracy, it is enough to perform an ultrasound of the upper abdominal cavity. With its help, you can identify stones in the ducts, gall bladder, determine the size of the bladder, its walls, the condition of the pancreas and liver. Gastroduodenoscopy is also performed to determine the condition of the mucous membrane of the stomach, esophagus and duodenum. If there are complications, retrograde cholangiography or transgastric ultrasound of the bile ducts is prescribed to detect choledocholithiasis.
Acute calculous cholecystitis
The cause of the acute form of calculous cholecystitis is stones that obstruct (clog) the neck of the gallbladder. In this case, the outflow of bile stops, and an infection develops in the bladder itself. The disease manifests itself as sharp pain in the right hypochondrium, nausea, repeated vomiting, and weakness.
An attack of acute calculous cholecystitis has some differences from “ordinary” hepatic colic. First of all, this is an increase in temperature, signs of inflammation in a blood test - neutrophilic leukocytosis, increased erythrocyte sedimentation rate, changes on ultrasound.
If it is not possible to achieve the effect of conservative therapy in the first day or two, the patient has to be operated on. Emergency surgery is more complex and has a greater risk of complications.
Etiology (causes)
Stones that form in the lumen of the gallbladder are insoluble compounds. They are mineral salts, bacterial cells, bile salts, they are glued together by thick mucus. The process of their formation is provoked by various reasons, as well as provoking factors, these include:
- Hereditary predisposition.
- Gender – in women, the metabolic processes of the liver are different, so the produced bile has a thicker consistency and is prone to the appearance of sediment.
- Poor nutrition - eating at different times, indulging in fatty, fried foods, and alcohol provoke changes in the chemical composition of bile.
- Increased body weight, which affects the intensity of metabolic processes in the liver, as well as the state of bile.
- Chronic inflammatory process of the mucous membrane of the hepatobiliary system, leading to disruption of the processes of secretion and concentration of bile.
Cholelithiasis, calculous cholecystitis can develop over a long period of time, and the stones increase in size. Also, their number may vary.
Treatment of acute calculous cholecystitis
In the first hours after the onset of an attack of acute calculous cholecystitis, conservative measures are taken:
- starvation;
- cold on the stomach;
- anesthesia;
- intravenous administration of antispasmodic drugs, antibiotics;
- detoxification therapy to normalize liver and kidney function.
All these actions can relieve the symptoms of an exacerbation, but in no case help eliminate the cause - the disease itself. The only reliable method of treating calculous cholecystitis, as well as cholelithiasis in general, is surgical removal of the gallbladder.
Gallstone disease (calculous cholecystitis) - symptoms and treatment
In the mid-twentieth century, the following method of treating cholelithiasis was studied in animal experiments: the gallbladder was cut, the stones were taken out, and sutured back. However, over time, the stones formed again, which is understandable, since gallstones are only a manifestation of the disease, and not the disease itself. Chronic inflammation of the gallbladder did not disappear, which led to relapse of the disease.
The next attempt to cure cholelithiasis without surgery was shock wave lithotripsy (similar to the treatment of urolithiasis). But this type of treatment caused rupture of liver tissue or the wall of the gallbladder with the formation of abscesses, hematomas and peritonitis. Fragments of stones, even if they were crushed, migrated into the ducts, causing choledocholithiasis and obstructive jaundice. The method had to be left in the past.
Some gastroenterologists recommend their patients take various choleretic drugs, as well as different types of “dubages” for the purpose of conservative treatment of cholelithiasis. Under the influence of this therapy, stones can easily migrate from the gallbladder into the extrahepatic bile ducts, causing choledocholithiasis and obstructive jaundice, which in turn will require emergency surgical intervention.
Thus, the only method of radical cure for gallstone disease is its removal - cholecystectomy.[3]
Initially, this operation was performed through a traditional (laparotomy) approach, which led to a large number of complications both in the early and late postoperative period. With the development of new technologies, the operation began to be performed laparoscopically.[7]
Cholecystectomy is performed as follows:
- through a centimeter incision above the navel, a tube (trocar) and a laparoscope are inserted into the abdominal cavity, the abdominal cavity is filled with carbon dioxide, thus forming a space for surgery;
- additionally install another centimeter and 25 mm trocars;
- with the help of special instruments, the gallbladder is mobilized, separated from the bed, the cystic duct and the artery are clipped with titanium clips;
- The gallbladder is removed through periumbilical or epigastric access.
The operation is performed under general anesthesia and lasts on average for an hour. Thanks to the low-traumatic laparoscopic approach, postoperative pain is minimal, and already in the evening on the day of surgery the patient can get up and walk without experiencing severe pain.
If the postoperative period is smooth, the patient can be discharged the next day after surgery, which is especially important for people of working age. The cosmetic defect of the operation is minimal; already a month after the operation, the scars become almost invisible.[6]
In parallel with laparoscopic cholecystectomy, cholecystectomy from a minilaparotomy approach arose. However, due to the difficulty of visualizing the elements of the hepatoduodenal ligament and the high risk of trauma to neighboring organs, this approach is practically not used.
Relatively recently, laparoscopic cholecystectomy began to be performed from a single approach. When performing this operation, a single incision 3-4 cm long is made above the navel. This access is especially relevant if the patient has an umbilical hernia, as it allows you to solve two problems through one incision.
NOTES surgery—operations through natural orifices—is gaining increasing popularity. Thus, laparoscopic cholecystectomy can be performed through an incision in the vagina or rectum, which does not leave scars on the abdomen, but is fraught with infectious and other complications.
Treatment of the disease
General principles of therapy:
- taking antibiotics;
- diet;
- physiotherapy;
- symptomatic therapy to alleviate the general condition.
In the chronic form of cholecystitis, treatment can be not only medicinal, but also surgical. Complex drug therapy includes the following groups of drugs:
- choleretic;
- antibiotics;
- digestive enzymes;
- prokinetics;
- non-steroidal anti-inflammatory drugs;
- antispasmodics;
- lacto- and bifidobacteria.
Surgical treatment is used when acute inflammation cannot be relieved with medications. In this case, the affected part of the gallbladder is removed.
Causes of the disease
The main cause of the pathology is infection and impaired bile outflow. The pathogenic pathogens include staphylococcus, streptococcus, E. coli, hepatitis viruses, lamblia and even roundworms. They penetrate the gallbladder area through the blood and lymph, causing inflammation.
Bile flow disorders can cause:
- cholelithiasis (in adults it accompanies cholecystitis in 80-95% of cases);
- biliary dyskinesia - weakening of the evacuation function of the gallbladder;
- dyslipidemia (disorders of fat metabolism);
- structural anomalies and various neoplasms that impede the drainage of bile - cysts, tumors, scars, narrowing and curvature of the ducts;
- valve dysfunction;
- dyscholia – a change in the composition of bile with an increase in its viscosity;
- alcohol and smoking abuse - provoke spasm and dyskinesia of the gallbladder;
- hormonal changes - reduce smooth muscle tone.
Among the inflammatory factors, it is worth mentioning allergic reactions and chronic diseases of the digestive and endocrine systems - diabetes, gastritis, pancreatitis. In particular, pancreaticobiliary reflux - the reflux of pancreatic enzymes into the gallbladder - provokes the development of enzymatic cholecystitis.
Symptoms of the disease appear against the background of psychological stress, poor nutrition, and physical inactivity.
Attention!
In the megacities of developed countries, the diagnosis of cholecystitis tends to rejuvenate. This is caused by unhealthy lifestyles and high levels of constant stress among the working population.
Diagnostic methods
Diagnosis begins with a visit to a gastroenterologist, who collects an anamnesis of the disease and life, and examines the patient. Further laboratory tests are prescribed:
- general urine analysis;
- several blood tests:
- biochemical;
- for sugar;
- for cholesterol;
- for pancreatic amylase;
- for antibodies to parasites;
- clinical.
- stool tests - coprogram, for antibodies to parasites.
To clarify the diagnosis and identify possible concomitant pathologies, the gastroenterologist may prescribe additional examinations:
- Ultrasound of the abdominal cavity;
- ECG;
- ERCP (endoscopic technique);
- MRI or CT with contrast;
- bilioscintigraphy;
- endoscopic ultrasound;
- duodenal intubation;
- bile culture;
- X-ray of the abdominal organs.
Treatment
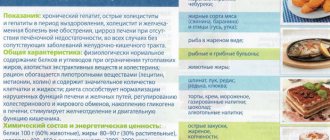
- Diet therapy (exclusion of foods that provoke symptoms of the disease: carbonated drinks, fatty foods, alcohol)
- Medications:
- Antispasmodic drugs: buscopan, dicytel, atropine, platifillin, no-spa
- Sorbents (activated carbon, enterosgel, smecta)
- Deoxycholic acid preparations (ursofalk, ursosan)
- Gastroenterological herbal collections
- Antibiotics: metronidazole, cephalosporins, fluoroquinolones
In case of acute cholecystitis, surgical intervention is required - emergency cholecystectomy.