Low pulse is one of the complaints of patients in cardiology departments. This phenomenon can cause many unpleasant moments, since it is accompanied by fainting states, weakness, cold sweat, dizziness, often being a sign of serious illness. Its systematic occurrence is a reason to seek professional medical help.
In order to find out the cause of a rare pulse, the doctor prescribes comprehensive diagnostic tests to identify existing problems. The pulse is represented by jerky oscillations of the arterial walls, by which the heart rate can be tracked and, having identified their violations, appropriate measures can be taken.
If you look at the accepted indicators of normal heart rate for different ages, you can conclude that it decreases as you get older. This is due to the growth of the muscular middle layer, known as the myocardium. The larger the volume of the heart, the fewer beats it needs to make in order to pump blood.
Causes of low heart rate
Despite the fact that the maximum frequency indicators can be called conditional and individual, depending on a number of factors (undoubtedly, within certain limits), the pulse is below 50 beats/min. - a sign of the presence of a disease. Its reduction to forty beats poses a threat to health and life, since the brain suffers from oxygen starvation. If it does not exceed forty beats within seven days, this is a sign of bradycardia, and with a progressive decrease, you should urgently seek professional medical help.
Almost all initiating factors of a pulse below normal are related to pathological conditions. For convenience, experts divide them into different categories, which can be found in our table.
| Category of reasons | How is it manifested? |
| Physiological | There are a number of natural factors and external influences that initiate a low pulse at normal pressure. Such conditions are not dangerous. This:
|
| Cardiological | The reasons for low blood pressure and low pulse may lie in the weakness of such a vital organ as the heart. They occur in the following diseases:
|
| Toxicological | Low blood pressure and low pulse can develop due to interaction with toxic substances when:
|
| Associated pathological conditions |
|
Low heart rate in the elderly is associated with age-related changes in the body. It often develops due to concomitant diseases or a natural slowdown in the body’s metabolic processes.
Is reducing heart rate the main goal in the treatment of patients with CVD? Cardiology: realities and prospects
Why is heart rate (HR) so important in the treatment of cardiac diseases? A select audience of leading specialists, clinical researchers and practicing cardiologists participated in the discussion of this and other issues related to the treatment of cardiovascular diseases on October 7, 2010 at an organized symposium within the framework of the Russian National Congress of Cardiologists. The abstracts of the most interesting speeches of the symposium participants are offered to the attention of readers.
ON THE. Mazur, Doctor of Medical Sciences, Professor, Head. Department of Cardiology, Russian Medical Academy of Postgraduate Education, Moscow
Rice. 1. The effect of drugs on the release of norepinephrine (Mazur N.A., Nazarov E.A., 1992)
Rice. 2. Study with Obzidan (Mazur N.A. et al., 1982)
Rice. 3. Dynamics of heart rate after a course of antihypertensive therapy (Mazur N.A., Lazareva O.N., 2008)
Rice. 4. SHIFT study (J. Kjekshus, EOC Congress, 2010)
S.F. Sokolov, Ph.D., Institute of Cardiology named after. A.L. Myasnikov FGU RKNPK MHSR RF
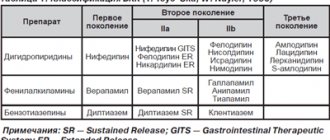
Table. Drugs recommended for rate control in AF
Rice. The effect of a single dose of bisoprolol (Corbis) on the average heart rate throughout the day in patients with persistent AF (squares indicate statistical significance of differences)
Survival of patients with coronary artery disease depending on the magnitude of the risk according to the results of a stress test
Results of the TIBBS study (bisoprolol 10 mg and nifedipine 40 mg)
Differences between monotherapy and combination therapy groups
Effect of 3-month combination therapy (Corbis, Stamlo M, Listril)
Platelet aggregation curves recorded by light aggregometry in a patient sensitive (observation A) and in a patient resistant to clopidogrel therapy (observation B)
Effect of drugs on heart rate and long-term outcomes in patients with cardiovascular diseases
This report presents the results of prospective placebo-controlled studies that demonstrated a positive effect on the so-called hard endpoints (overall mortality and mortality from cardiovascular diseases, including sudden death, as well as the incidence of myocardial infarction and non-fatal stroke). Data from the analysis of results in retrospectively selected groups in accordance with modern requirements of evidence-based medicine are classified as having no evidence.
Heart rate frequency (HRF) is an integral indicator of physical capabilities, general health, life expectancy of a person, including patients with cardiovascular diseases, and also reflects the degree of activity of the autonomic nervous system.
In particular, in patients who have suffered a myocardial infarction, the optimal HR is less than 60 per minute. In our studies, it was found that beta-adrenergic blockers (BABs) had the greatest effect on heart rate when used in targeted doses, reducing the heart rate by 22%, as well as verapamil SR and diltiazem SR, reducing the rhythm by almost 10 and 4%, respectively. ACE inhibitors very moderately (not significantly) reduce the rhythm frequency, while long-acting dihydropyridine calcium antagonists moderately increase it. A decrease in heart rate is combined, according to our data, with a decrease in the release of norepinephrine (NA), and its increase, for example, under the influence of a diuretic or nifedipine, is combined with an increase in the release of NA, determined during a low dose load, which significantly reduces the likelihood of exposure to other irritants from the patient’s environment environment on the content of catecholamines in the blood (Fig. 1).
Numerous studies in patients with coronary artery disease have shown that cardioselective (with the exception of Nebilet) and non-selective beta blockers without internal sympathomimetic action significantly reduce the risk of overall mortality and the risk of developing myocardial infarction. In our study (Fig. 2), which included only patients with a high risk of sudden death, therapy with propranolol (Obzidan) in individually selected doses (from 80 to 320 mg/day), which reduced the heart rate by 15% or more, noted a significant decrease in mortality, compared with the control group of patients under the supervision of clinic doctors.
At the same time, in the COMET study with carvedilol (Dilatrend), which reduces heart rate to a lesser extent than other cardioselective beta blockers without sympathomimetic action, its use at the maximum dose (25 mg 2 times a day) compared with short-acting metoprolol at a low dose (50 mg 2 times a day) there were no advantages in influencing survival, and the mortality rates were the same. It is likely that the lower effectiveness of carvedilol (taking into account the dose/effect indicator) is due to the fact that the drug, in addition to beta-adrenergic blocking, also has an alpha-adrenergic blocking effect, which probably has a stimulating effect on the activity of the sympathoadrenal system.
Pulse-suppressing calcium antagonists in patients with documented coronary artery disease (that is, those who have had an MI), who do not have blood stagnation in the pulmonary and/or systemic circulation, also significantly reduce overall mortality and the risk of sudden death. In studies using amlodipine or nifedipine - GITS, which clearly have anti-ischemic effects, no reduction in mortality was observed.
To understand the mechanism of the positive effect of pulse-lowering drugs, two studies using Coraxan (BEAUTIFUL, SHIFT), which reduces only the sinus rhythm of the heart, without producing other effects that beta blockers and pulse-shortening calcium antagonists have (Fig. 4), are very important. Against the background of standard therapy (blockers, ACE inhibitors, etc.), additional administration of Coraxan did not lead to a decrease in overall mortality, mortality from CVD and the incidence of sudden death. The results obtained by retrospectively identifying groups of patients are not, as is customary today, evidence-based and are of a speculative nature.
The revealed patterns of the influence of beta blockers on the survival of patients with coronary artery disease are of the same nature in patients with heart failure. For example, therapy with bisoprolol in targeted doses reduced overall mortality by one third (p
A comparison of the effectiveness of metoprolol and a thiazide diuretic (MAPHY study), which, according to our data, increases the release of NA in patients with arterial hypertension (AH), demonstrated a significantly more significant effect of beta blockers on patient survival and the incidence of coronary artery disease.
Thus, drugs that have an antiadrenergic effect, which also cause a decrease in heart rate, reduce the risk of death in patients with coronary artery disease, chronic heart failure and hypertension. Isolated inhibition of sinus node function under the influence of Coraxan does not have a positive effect on the survival of patients with coronary artery disease and heart failure.
The importance of heart rate control in patients with atrial fibrillation
The development of atrial fibrillation (AF) has important hemodynamic consequences associated with loss of atrial contraction, irregular ventricular contraction, myocardial ischemia and, most importantly, an increase in heart rate (HR). The latter is due to the fact that in AF, ultra-frequent atrial impulses make the heart rate entirely dependent on the “throughput” of the AV node, which is not provided by nature as a mechanism for adapting the heart rate to the physiological needs of the body and turns out to be excessively high. The consequences of high heart rate, in addition to painful clinical symptoms, is a cascade of pathological changes, the end result of which is hemodynamic disturbances, leading to a decrease in the quality of life and even to the development of acute or chronic heart failure, and in some cases to a specific form of cardiomyopathy.
Treatment of AF involves five main areas: elimination of clinical symptoms, optimal treatment of the underlying cardiovascular disease, prevention of thromboembolic complications, and two more areas that are generally considered as alternative treatment strategies. These are “rhythm control,” which involves eliminating AF and maintaining normal sinus rhythm by pharmacological or non-pharmacological means, and “rate control,” which involves not eliminating AF and treatment aimed at normalizing heart rate.
A large number of studies have been carried out to compare the two indicated strategies (RACE, AFFIRM, AF-CHF, etc.), but none of them revealed significant differences in the final treatment results. In this regard, the choice of strategy seems arbitrary and is significantly influenced by, on the one hand, the desire to use all possibilities to maintain normal sinus rhythm, and, on the other hand, the obvious futility of attempts to eliminate AF and prevent its relapses. It should be taken into account that with each episode of AF, regardless of its form, initial treatment measures should be aimed at normalizing heart rate and only depending on the results obtained can a further decision on the choice of treatment strategy for the patient be made. Moreover, current recommendations for the management of patients with AF require continued prescription of drugs that reduce heart rate, even when choosing a “rhythm control” strategy in case of possible recurrence of arrhythmia.
In this regard, the question becomes important to what extent it is necessary to reduce the heart rate in AF so that the treatment effect can be considered achieved. Different studies make different recommendations, so two directions can be distinguished: the use of “soft” and “hard” criteria of effect. The first involves a simple decrease in heart rate at rest below 100–110 imp/min, while the second involves a decrease in heart rate at rest below 80 imp/min and, in addition, the use of Holter ECG monitoring and exercise testing to control heart rate. However, direct comparisons of treatment outcomes using these two measures of effect indicate no significant differences in the final treatment outcome. In this regard, it is recommended to use “soft” criteria for asymptomatic or minimally symptomatic AF, and to use “hard” effect criteria for severe symptoms.
The main means of reducing heart rate in AF are drugs that have a negative dromotropic effect on the AV node. These include beta-blockers (BAB), an important property of which is the ability to reduce heart rate during exercise, non-dihydropyridine Ca2+ antagonists (NAC), cardiac glycosides (CG) and amiodarone. The choice of drugs depends on the patient’s physical activity and his underlying disease. With an inactive lifestyle, the administration of cardiac glycosides alone may be sufficient. With an active lifestyle, in the case of the idiopathic form of AF and its occurrence against the background of arterial hypertension, the first choice drugs are beta blockers, followed by NAC and SG, as well as combinations of the above drugs. In the presence of heart failure, the use of beta blockers and SG and their combination is recommended. For patients with chronic obstructive pulmonary diseases, NACs are the first choice drugs, but the use of SG and β1-selective beta blockers is not excluded. Recommended medications are presented in the table.
It is noteworthy that in the recommendations of the European Society of Cardiology in 2010, bisoprolol was included in the list of beta blockers for the first time, even despite the fact that there are no large randomized trials of this drug for the indication in question. Bisoprolol, being a β1-selective beta blocker and effectively reducing heart rate in AF, has pharmacokinetic properties that make it very convenient for use in long-term treatment. With a single dose in the morning, its maximum effect occurs in the daytime, precisely when a decrease in heart rate, determined by physical activity, is required. At night, when inhibition of conduction through the AV node is fraught with the development of excessive bradycardia, its effect is less pronounced.
These properties of the drug were confirmed in our study, in which the effect of bisorolol (Corbis®) in doses of 5 and 10 mg per day with a single oral dose was studied in 20 patients with persistent AF. The figure clearly illustrates the effective decrease in heart rate under the influence of the drug during the daytime with the virtual absence of an additional and optional decrease in heart rate at night.
The role of control of myocardial ischemia with the help of pulse-lowering and non-pulse-lowering drugs in the treatment of patients with angina pectoris
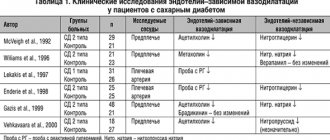
Our report presents the results of clinical studies that demonstrated the prognostic role of myocardial ischemia, as well as the effect of pulse-lowering and non-pulse-lowering drugs on ischemia and long-term outcomes in patients with angina (see table).
Treatment of patients with stable angina involves highlighting the following objectives: influence on prognosis, control of ischemia and improvement of quality of life. To reduce the severity of ischemia and reduce the symptoms of the disease, the European Society of Cardiology recommends 4 classes of antianginal drugs: 1) beta-adrenergic receptor blockers, 2) calcium channel blockers, 3) drugs that increase the formation of nitric oxide, 4) a potassium channel activator (nicorandil). The most effective therapy should be considered the one that, along with the antianginal effect, will increase the survival rate of patients with coronary heart disease. The mechanisms of antianginal action of these groups of drugs differ significantly in the degree of influence on neurotransmitter activity; drugs have different effects on vascular resistance, smooth muscle cell tone and heart rate.
The criteria for the anti-ischemic effectiveness of the drug, which correlate with a significant increase in quality of life, are the prevention or significant reduction (by 50–70% or more) in the degree of ST segment depression and its later (2–3 min) occurrence during a stress test.
All groups of drugs in appropriate doses have a comparable anti-ischemic effect. The “oldest” antianginal drugs – nitrates – have the most pronounced effect (EOC, 2006). However, there is no data on the effect of nitrates on mortality in patients with stable angina. It is especially important to ensure a reduction in the risk of complications and a reduction in mortality. In the studies conducted, the greatest amount of evidence of benefit was obtained regarding the use of beta blockers. Prescribing them to patients who have had a myocardial infarction reduces the likelihood of death by 22% and reduces the risk of recurrent myocardial infarction by 27%, and for patients with a high risk of sudden death, it was reduced by 30–50%. In the 1980s, a number of studies were conducted (DAVIT I, DAVIT II, CRIS, INTERCEPT) demonstrating the positive effect of pulse-lowering calcium antagonists on the incidence of recurrent MI and sudden death in patients with coronary artery disease without signs of congestive heart failure. Dihydropyridine calcium antagonists (amlodipine, nifedipine - GITS) do not have an effect on overall mortality, despite the proven anti-ischemic effect (Fig. 1).
A potassium channel activator (nicorandil) has an antianginal effect, but there is no convincing evidence of a positive effect on prognosis (IONA study).
In real practice, patients with stable angina often have concomitant arterial hypertension, diabetes mellitus, and atherosclerotic lesions of peripheral arteries, which requires the selection of appropriate therapy.
Our study examined the anti-ischemic effectiveness of bisoprolol (Corbis) therapy in patients with angina pectoris in combination with hypertension and atherosclerosis of peripheral arteries. The selection of patients with angina pectoris required the presence of documented ST segment depression in CM and atherosclerotic plaques in the arteries of the lower extremities. Of the included patients, 75% of patients had concomitant hypertension, 20% had type 2 diabetes mellitus. Atherosclerotic damage to peripheral vessels was recorded in all patients, and in some of them it was severe (22%). At the same time, atherosclerotic plaques were recorded in the brachiocephalic arteries in all patients. All patients took bisoprolol (Corbis), in the absence of sufficient antianginal and hypotensive effect, a second drug was added - dihydropyridine AK - Stamlo M; if the combination was ineffective, lisinopril (Listril) was added. A quarter of patients were on Corbis monotherapy, more than half (58%) were taking a combination of Corbis and Stamlo M and 17% were taking 3 drugs.
The mono- and combination therapy groups differed significantly from each other in clinical data (Table 2). In the combination therapy group, 30% of patients had a history of myocardial infarction, all patients had concomitant hypertension, 26% had type 2 diabetes mellitus, and there were also signs of severe damage to peripheral arteries (1/3 had severe stenosis of the brachiocephalic arteries and a quarter had intermittent lameness).
Therapy for 3 months led to a significant decrease in heart rate (more than 10 beats/min) and a decrease in blood pressure, the number of episodes of ST depression decreased threefold, and the duration of ischemia and the total ischemic index decreased by 4 times. When comparing the effectiveness of combination and monotherapy, heart rate and blood pressure decreased equally significantly, the number of ischemic episodes decreased by 3–4 times, and indicators such as duration and total ischemic index decreased by 4 and 5 times, respectively. The pulse wave velocity in the peripheral arteries decreased significantly in the combination therapy group, but did not change significantly in the aorta. Changes in pulse wave velocity in the arteries of the lower extremities were mainly observed in the group of patients with initially unchanged ABI.
The data obtained showed that therapy with the drugs used in patients from real practice had a pronounced anti-ischemic, hypotensive effect and no negative effect on peripheral blood flow according to volumetric sphygmography (Table 3).
Thus, antianginal drugs from different groups, although they reduce the severity of myocardial ischemia, do not improve the prognosis of life to the same extent, since the effect on survival is associated not only with the anti-ischemic effect, but also with other effects of the drugs (decrease in SNS activity, effect on organs -targets and electrophysiological properties of the myocardium).
Disaggregant therapy in patients with coronary heart disease
Disaggregant therapy is a mandatory component of modern drug treatment of coronary heart disease (CHD) and other vascular diseases caused by atherosclerosis. The introduction of coronary angioplasty with stent implantation into the practice of treating patients with coronary artery disease and the results of studies on the prognosis after such interventions have provided colossal factual observational material on this problem. Clinical and laboratory studies of the state of aggregation in various pathologies, primarily in ischemic heart disease, and the experience of using glycoprotein IIb/IIIa inhibitors in acute myocardial infarction have contributed to strengthening the understanding of the role of disaggregants in the treatment of ischemic heart disease. The role of acetylsalicylic acid in the primary and secondary prevention of coronary artery disease was outlined, and the value of clopidogrel was established as the optimal means to date for achieving a long-term disaggregant effect in mono- and combined (double disaggregant) therapy. Numerous studies assessing the effect of antiplatelet agents on the course of CVD have shown an unconditional positive effect of therapy in reducing the incidence of myocardial infarction, stroke, and overall mortality.
Despite the widespread use of antiplatelet therapy, some important aspects of antiplatelet drug treatment remain poorly developed.
Among the urgent tasks that need to be addressed in the coming years are the following:
- development of a generally accepted and practical algorithm for identifying patients resistant to therapy;
- achieving agreed decisions on the use of laboratory methods for assessing the effect of antiplatelet agents;
- achieving consensus on the issue of clopidogrel dosages;
- the problem of the optimal duration of antiplatelet therapy and the problem of thienopyridine withdrawal syndrome at the outpatient stage;
- bleeding when using antiplatelet agents and prevention of bleeding.
Solving these problems represents a task of varying levels of complexity. Some of them can be solved today, others require additional research. The increasing use of coronary angioplasty of the coronary arteries requires increased “aggressiveness” of therapy. With endovascular angioplasty, two or three component antiplatelet therapy is most often used - the so-called double (acetylsalicylic acid + clopidogrel) and triple (with the addition of IIb/IIIa receptor blockers in the acute period); in some cases, a combination of ASA with thienopyridine and warfarin is used. The current trend is to use higher loading doses of clopidogrel. For acetylsalicylic acid, a dose range has been experimentally established at which the best results in terms of preventing complications are observed - 100–375 mg/day. It has been empirically established that increasing the dose does not lead to an improvement in these indicators, and a decrease below 75 mg/day is accompanied by a loss of any preventive effect.
The effect of antiplatelet agents is individual and depends on many factors (see figure). It has been established that approximately 30% of patients with coronary artery disease during an in-depth study show insufficient effectiveness of disaggregants, which in the literature is called resistance to disaggregants (aspirin, clopidogrel). Among the mechanisms for the development of resistance, various factors can be indicated: the state of the receptors on which the disaggregant should act, genetically determined features that determine the functioning of the receptor (gene mutations, receptor polymorphism), the state of other blood cells, the presence of ongoing inflammatory processes, accelerated destruction and formation of platelets in the body , smoking, non-compliance with medication regimen by patients.
Considering the fairly large number of resistant patients, it can be assumed that many of them receive ineffective treatment (ineffective?). Such treatment, instead of potential benefits, may bring a potential risk of side effects; at the same time, neither the doctor nor the patient is aware of this, since assessing the effect of disaggregants based on subjective sensations is impossible. New drugs with more powerful effects are expected on the pharmaceutical market. However, clopidogrel remains a convenient drug for long-term therapy. New drugs may reduce the number of resistant patients, therapy will become more effective, which could potentially provoke an increase in the incidence of side effects, especially in conditions of uncontrolled use. Increasing dosages for long-term use may lead to a decrease in the number of resistant patients, but will contribute to an increase in bleeding.
Clinical manifestations of low heart rate
A moderate decrease in pressure most often does not lead to the development of clinical manifestations and is not accompanied by circulatory disorders. However, with a heart rate of no more than forty beats per minute, the following are observed:
- dizziness;
- weakness;
- semi-fainting and fainting;
- feeling of constant fatigue;
- labored breathing;
- pain symptoms in the chest area;
- blood pressure surges;
- inability to concentrate;
- forgetfulness;
- visual impairment.
Symptoms with a low pulse correspond to circulatory disorders that appear against its background. So, if it is slowed down, the brain suffers from a lack of oxygen and hypoxia develops (that is, oxygen starvation). As a result, the patient is susceptible to convulsions and loss of consciousness, lasting from several seconds to one minute. Such conditions are life-threatening and can cause respiratory arrest and therefore require immediate medical attention.
Types of bradycardia
There are several types of bradycardia:
- Absolute – with a steadily reduced heart rate, which does not increase even with physical activity;
- Relative – the pulse increases in proportion to the degree of load or against the background of infectious diseases;
- Moderate - at rest, the pulse does not exceed 40 beats per minute.
Even if a decrease in heart rate does not bother a person or cause any discomfort, it is necessary to identify the cause of such changes in order to prevent the risk of dangerous complications.
Diagnosis of low heart rate
Determining the causes of a pathologically low pulse requires a comprehensive diagnosis. First of all, the doctor listens to the patient’s complaints, collects anamnesis and conducts an examination. If bradycardia (i.e., decreased heart rate) is detected, the patient is prescribed a consultation with a cardiologist. As for diagnostic studies, they are as follows:
- Electrocardiography;
- Daily Holter monitoring;
- Ultrasound scan of the heart;
- EchoCG;
- Bicycle ergometry.
In addition, if necessary, TEE can be performed, which allows one to study the conduction pathways of the heart and determine the organic or functional nature of the disease.
Treatment for low heart rate
A moderate decrease in heart rate that occurs without symptoms does not require therapy. However, if it exists, the underlying pathology must be treated. The strategy depends on the underlying disease, but in any case is aimed at:
- Elimination of symptoms of low heart rate;
- Eliminating the risk of heart rhythm disturbances;
- Prevention of thrombosis development.
If the problem arose as a result of uncontrolled use of pharmacological drugs, their dose is adjusted - or, if they are not needed, completely canceled.
Symptoms
If the pulse decreases significantly, the person experiences:
- weakness of the body as a whole;
- headache of varying strength;
- numbness in the limbs and a decrease in their temperature;
- problems with vision, attention, concentration.
Once again, it is worth emphasizing that symptoms are not always immediately visible, so it is worth, especially in old age, to measure your pulse immediately after waking up.
How to quickly increase your heart rate?
If a rare pulse is not a symptom of heart disease and appears for physiological reasons, you can speed it up and eliminate unpleasant symptoms by using simple remedies available in almost every home. Before starting activities, it is important to take into account the circumstances under which the heart rate decreased.
| Initiating factor | How and with what is it manifested? |
| Stress, shock, nervous disorders | If the heart rate decreases to forty beats per minute or below, you can take sedatives:
|
| Decreased blood pressure and pulse | The best option is to take decoctions for:
|
| Increased blood pressure and decreased heart rate | The best solution would be:
|
| Pregnancy |
|
If a person is sufficiently resilient and healthy, physical activity (from running, jumping and squats to cardio exercises) would be a good option.
Prevention of rare pulse
Preventive measures boil down to timely treatment of organic heart lesions, elimination of the effects of toxic substances on the myocardium, competent selection of doses of pharmacological drugs and their administration under medical supervision. Don't forget to make regular preventive visits to your therapist and cardiologist.
Make an appointment with CELT specialists and find out the reasons for your rare pulse without delay.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions