Acute short-term complications of diabetes mellitus
Ketoacidosis
Diabetic ketoacidosis DKA is an acute insulin deficiency. If diagnosed late without treatment, it can lead to coma and death. It can develop in any type of diabetes, but is more common in type I.
Reasons for development
Without insulin, glucose does not enter cells. Instead, the body begins to break down fats as a source of energy. As a result, toxic ketone bodies are formed in excess. Within a few days they enter the blood and urine.
Early signs of pathological process:
- dry mouth, thirst, dry skin;
- high blood sugar level – 13 mmol/l and above;
- constant fatigue;
- frequent urination;
- weight loss.
When the level of ketone bodies in the body becomes critical, acute ketoacidosis develops. Its symptoms:
- abdominal pain, nausea and vomiting;
- a characteristic fruity smell from the mouth (usually felt by others, and not by the patient himself);
- high levels of ketone bodies in the blood and urine;
- drowsiness, lethargy;
- frequent, deep, sometimes difficult breathing;
- inability to concentrate;
- disturbance of consciousness.
From the moment vomiting appears, the pathology begins to progress rapidly to a life-threatening condition. If these symptoms appear, you should urgently call a doctor or an ambulance.
Therapeutic tactics for symptoms of DKA
First, blood glucose levels are measured. If it is 13 mmol/L or higher, measure the level of ketone bodies in the urine using test strips.
If this indicator is normal:
- short-acting or ultra-short-acting insulin is administered;
- Prescribe plenty of fluids - an average of 1 l/hour;
- monitor blood sugar levels and the level of ketone bodies in urine every 4-6 hours (the interval is determined by the doctor);
- treat concomitant pathologies (if any);
- limit physical activity to the minimum possible (it promotes more intense formation of ketone bodies).
If the level of ketone bodies is higher than normal, infusion therapy is indicated (carried out in a hospital or at home under the supervision of a doctor).
Hyperosmolar coma
Hyperosmolar diabetic coma is an extreme degree of metabolic disorder without ketoacidosis and background critical hyperglycemia (33 mmol/l and above). The body becomes dehydrated, and the levels of nitrogen, sodium and chlorine in the blood increase. With late diagnosis and treatment, mortality in hyperosmolar coma is 30-50%.
Causes of the condition:
- blood loss;
- a significant increase in the volume of urine excreted - due to the use of diuretics or other medications, dialysis, administration of saline solutions;
- diarrhea and vomiting;
- acute circulatory disorders;
- injuries and burns;
- severe infectious diseases.
Aggravating factors are increased blood glucose levels and the addition of concomitant diseases.
Signs of hyperosmolar coma
For 5-14 days before the attack, there is increased thirst and appetite, frequent and/or excessive urination, loss of strength and muscle weakness, up to the complete cessation of physical activity.
What to do
It is necessary to call an ambulance - treatment is carried out in the intensive care unit or intensive care unit. Treatment tactics include:
- rehydration - drip intravenous administration of medicinal solutions under the control of venous and blood pressure, the level of dehydration and the level of electrolytes in the blood plasma;
- insulin therapy.
Hypoglycemia
A decrease in blood glucose levels below 3.9 mmol/l. In a relatively mild form it is not dangerous: the patient himself can restore normal sugar levels. Severe forms of hypoglycemia damage brain cells and are life-threatening.
The condition occurs:
- due to insulin overdose;
- overdose of glucose-lowering drugs;
- increased insulin sensitivity due to exercise;
- local heating, massage, excessive depth of injection;
- increasing the interval between insulin and food;
- skipping meals;
- lack of carbohydrates;
- fasting;
- slowing down the evacuation of stomach contents;
- drinking alcohol.
Signs of hypoglycemia
Most patients feel an increase in hypoglycemia - they develop warning symptoms:
- shiver;
- heartbeat;
- pallor;
- fatigue;
- inability to concentrate;
- anxiety;
- sweating;
- increased appetite;
- sensory disturbances - goosebumps, numbness, etc.;
- nightmares.
As the sugar level decreases, dizziness, speech and vision disturbances, and convulsions are added. In a hypoglycemic coma, a person loses consciousness.
Treatment
In case of hypoglycemia, it is important to restore normal blood glucose levels. For relatively mild forms, it is enough to eat sugar, candy, a piece of chocolate, or honey. In severe forms, you need to call a doctor or an ambulance. Dextrose or glucan is administered intravenously to the patient.
Lactic acid coma
A sharp increase in the level of lactic acid in the blood.
Causes
Develops due to oxygen deficiency in tissues due to anemia, shock, carbon monoxide poisoning, alcohol or certain medications. It may occur against the background of kidney, liver, bone marrow, or bleeding diseases. The cause may also be myocardial infarction, serious illness or excessive physical activity.
Signs of lactic acidotic coma
The condition develops rapidly, within a few hours. The main manifestations are chest pain, diarrhea, noisy breathing, abdominal pain and vomiting, drowsiness or insomnia. Reflexes may disappear and motor activity may be impaired - muscle activity decreases or, on the contrary, involuntary movements appear. The patient's body temperature drops, urine ceases to be excreted, the contractility of the heart muscle decreases, blood clots form and even necrosis of the fingers.
Treatment
- Drip administration of a solution of soda, methylene blue or triamine, as well as small doses of insulin in 5% glucose.
- In severe cases, connection to an artificial kidney apparatus is indicated.
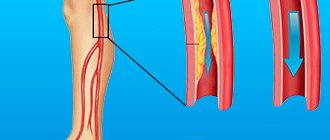
Damage to small vessels in diabetic angiopathy
When small vessels are damaged, changes occur in their walls, blood clotting is disrupted and blood flow slows down. All this creates conditions for the formation of blood clots. Mainly small vessels of the kidneys, retina, heart muscles, and skin are affected. The earliest manifestation of diabetic angiopathy is damage to the lower extremities.
The processes occurring in blood vessels are of two types: thickening of the walls of arterioles and veins or thickening of capillaries. Initially, under the influence of toxic products that are formed during incomplete utilization of glucose, the inner layer of blood vessels swells, after which they narrow. The first manifestations of diabetic angiopathy are small hemorrhages under the nail plate of the big toe. The patient feels pain in the limbs, notices that the skin becomes pale, spots appear on it, nails become brittle, and the muscles of the legs “shrink out.” The pulse in the main arteries of the lower extremities does not change, but in the foot it may be weak.
Changes in the arteries of the retina may be detected and protein may appear in the urine. A specific painless bubble filled with bloody fluid appears on the skin of the feet. It heals on its own without forming a scar, however, microorganisms can enter the tissue and cause inflammation.
The following research methods are used to diagnose diabetic angiopathy:
- capillaroscopy;
- infrared thermography;
- introduction of radioactive isotopes;
- laser flowmetry;
- polarography or oxyhemography.
Late chronic types of complications of diabetes mellitus
Diabetic micro- and macroangiopathy
Damage to the walls of large vessels and capillaries, accompanied by a violation of the functional state of the blood.
Causes
Occurs during decompensation of diabetes - with large daily fluctuations in the levels of glucose, proteins and fats. Aggravating factors of development are obesity, hypertension, smoking.
Signs
Due to metabolic disorders, the vessels of target organs are affected - the heart and limbs, the retina and the renal glomeruli. Because of this, the supply of oxygen to tissues is reduced, hormonal balance and metabolic processes are disrupted.
As a result:
- visual functions deteriorate;
- cardiovascular and renal failure develops;
- brain activity and nerve conduction are disrupted;
- Trophic ulcers develop on the arms and legs.
Without treatment, angiopathy progresses and can lead to complete blindness, amputations of limbs, heart attacks and intoxications, and deterioration of mental abilities.
Treatment
Diabetic angiopathy requires correction of the treatment regimen, as well as normalization of weight and blood pressure, and cessation of smoking. In addition, the doctor may prescribe drugs that strengthen the vascular wall - flavonoids, venotonics and phlebotonics.
Diabetic polyneuropathy
Damage to nerve endings up to complete ischemia - loss of sensitivity in the affected areas.
Causes
Develops with elevated blood sugar levels - when the drug or dose is chosen incorrectly.
Signs
Manifested by pain, loss of sensitivity, numbness, and night cramps. If large nerve fibers are damaged, loss of balance may occur.
Treatment
The goal of treatment is compensation of diabetes mellitus. Also indicated are drugs that improve neuromuscular conduction and symptomatic drugs for pain and cramps.
Diabetic encephalopathy
Damage to brain structures - mainly neurons and white matter. It develops slowly and imperceptibly, so it often appears in the later stages.
Causes
Typical metabolic disorders associated with long-term diabetes mellitus. In addition, risk factors are atherosclerosis, hypertension, and increased levels of C-peptide in the blood.
Signs
- deterioration of mental activity – mild to moderate (dementia rarely develops);
- emotional instability;
- increased anxiety;
- tendency to depression;
- chronic fatigue syndrome.
Treatment
Regular cognitive screenings and maintaining normal blood sugar levels. To improve brain activity, nootropic, antioxidant, antiplatelet and vasoactive drugs, vitamins B, E and alpha-lipoic acid are prescribed.
Diabetic foot syndrome
Purulent-necrotic and ulcerative lesions of the feet.
Causes
The condition occurs due to complex changes against the background of diabetic pathologies of blood vessels, nerves and tissues.
Signs
It manifests itself as increased trauma and infection of tissues, purulent-necrotic processes, which may require amputation.
Treatment
- control and correction of blood glucose levels;
- control and correction of blood pressure and cholesterol levels;
- professional foot care, monthly examinations by a podiatrist;
- unloading the foot;
- antiseptics and antibiotics for signs of wound infection;
- painkillers;
- drugs that improve nerve conduction;
- medications that improve blood flow.
When phlegmons and abscesses form, surgical opening is indicated. According to indications, angioplasty and stenting are performed. In extreme cases, gentle resections or amputations may be necessary.
Diabetic nephropathy
Damage to kidney structures due to diabetic metabolic disorders.
Causes
Elevated blood sugar levels cause increased pressure in the glomeruli. Because of this, the kidneys begin to excrete protein in the urine. Over time, this causes fibrosis of the kidney tissue. A factor that worsens the prognosis is concomitant atherosclerosis.
Signs
The disease remains asymptomatic for years and eventually leads to kidney failure. Its symptoms are a sharp decrease in daily urine volume and critical disruption of urinary processes.
Treatment
Selecting the correct treatment regimen allows you to prevent the process and even cause its reverse development in the early stages of the disease. Specific treatment is carried out with ACE inhibitors or angiotensin receptor blockers. Nephroprotectors are often prescribed; in severe cases - hemodialysis.
For elevated cholesterol levels, statins are indicated, and for hypertension, antihypertensive drugs are indicated. Diabetics with nephropathy are prescribed a diet with moderate restriction of animal protein. It is also important to normalize your weight and quit smoking.
Diabetic retinopathy
Damage to the vessels of the retina of the eyeballs.
Causes
Develops due to decompensation of diabetes. Due to increased blood glucose levels, the barrier properties of the retinal tissues decrease, the lumen of the vessels and the blood flow in them increase, the inner wall of the vessels is damaged, and the capillaries become permeable. Due to repeated hemorrhages, degeneration of the ocular structures develops.
Signs
Diabetic retinopathy is manifested by deterioration of vision up to complete blindness. Possible eye pain.
Treatment
Annual examination by an ophthalmologist specializing in diabetes, monitoring of sugar levels and dietary therapy. Animal fats are replaced with vegetable fats, fast carbohydrates are excluded, and lipotropic foods are introduced into the diet - fish, oatmeal and cottage cheese - to normalize cholesterol levels.
The menu also includes more fruits and vegetables (except starchy ones). Vitamin therapy and angioprotectors are often prescribed. At stages 3 and 4 of diabetic angiopathy, laser photocoagulation may be recommended.
Methods for diagnosis and treatment of diabetic macroangiopathy
P
According to the International Diabetes Federation, there are currently 4.9 million patients with type 1 diabetes mellitus (DM) in the world and an increase is expected to 5.3 million by 2011, while the number of patients with type 2 DM in the world is 151 million, and by 2011, 213 million are expected [1].
This disease is a significant and independent risk factor for atherosclerosis. According to modern concepts, the clinical course and individual prognosis for the development of diabetes mellitus depend on the degree of prevalence and severity of vascular disorders in this disease [1,2]. Most patients with diabetes die from cardiovascular complications
, with coronary heart disease (CHD) occupying a leading position among the causes of death. The risk of developing coronary artery disease and obliterating atherosclerotic lesions of the arteries of the lower extremities in people with diabetes is increased by 3–5 times [3]. IHD develops earlier against the background of diabetes than in its absence, and the course of the disease is more often complicated by unstable angina, myocardial infarction, threatening rhythm disturbances, and congestive heart failure develops faster. Chronic obliterating diseases of the arteries of the lower extremities (COLD) in patients with diabetes are characterized by a more severe course, occurrence at a younger age, lack of distribution by gender, symmetry of the lesion, more frequent involvement in the pathological process of the deep artery of the femur, popliteal artery and vessels of the leg [4 ]. The disease is often complicated by the appearance of trophic disorders of the distal parts of the foot, the development of gangrene and painless forms of the disease [5].
Changes in the arterial bed in diabetes mellitus of both types 1 and 2 are systemic in nature, all vital organs are involved in the pathological process, and disturbances predominate at the level of microcirculation. The timely receipt of any objective additional data on the state of the arterial bed in patients with diabetes cannot be overestimated. Currently, it is generally accepted that patients with diabetes are more likely than the general population to develop widespread atherosclerosis of the great arteries.
[3,6,7]. Diagnosis of these diseases against the background of diabetes is often difficult, since with this combination of coronary artery disease and COPD are often asymptomatic, even painless forms. Therefore, people suffering from diabetes should more actively conduct screening studies for coronary artery disease and COPD, especially with associated risk factors, for early detection of atherosclerotic lesions - before the clinical manifestations of the disease.
All patients with diabetes should undergo routine and imaging stress tests, and 24-hour ECG monitoring. In cases of verified coronary artery disease, the presence of diabetes should be considered as an additional factor in favor of coronary angiography for visualization of the coronary bed. A study conducted at the Cleveland Clinic showed that 90% of patients who underwent routine coronary angiography before surgery on the vessels of the lower extremities had varying degrees of coronary atherosclerosis, and 28% had severe three-vessel coronary heart disease [8].
In order to study hemodynamics in the arteries of the lower extremities and topical diagnosis of lesions of the arterial bed, the following instrumental research methods are used: Doppler ultrasound sphygmomanometry, treadmill test, ultrasound angioscanning, including duplex, transcutaneous oximetry and radiopaque aortoarteriography.
Dopplerography and segmental Doppler manometry
allow you to determine the degree of ischemic lesions, the level and extent of occlusion, as well as assess the condition of the collateral vascular bed.
The captured Doppler signal is used to measure segmental systolic pressure and analyze the tape-recorded Doppler waveform. The calculation of indices contributes to greater objectification of measurement, i.e. relative indicators. The most commonly used is the ankle-brachial index (ankle pressure index) - ABI, calculated as the ratio of arterial systolic pressure in the anterior or posterior tibial artery to this indicator in the brachial artery. Normally, the ABI is between 1.0 and 1.5. A decrease in this index below 1.0 indicates damage to the artery proximally or at the measurement site. An increase in the index to 1.3 indicates the presence of neuropathy. Higher numbers of systolic pressure and ABI in the lower leg and foot in diabetes mellitus are associated with a decrease in the elasticity of the tibial arteries and arteries of the feet (due to Mönckeberg's sclerosis), which counteract the compression of the vessels by the cuff. In this regard, measuring ABI in patients with diabetes is a less informative test in assessing the degree of limb ischemia than in the general population. The results obtained do not always reflect the clinical picture of the disease. Sometimes ABI values in patients with diabetes do not differ from normal values even with III–IV degrees of limb ischemia. digital systolic pressure is informative.
(PSD). The middle tunica of the digital arteries usually remains intact, which allows reliable research results to be obtained. Normally, PSD is slightly lower than in the brachial artery, and is 60% or more of the expected systolic pressure in the arteries of the leg. However, it is not possible to measure PSD in all patients with diabetes due to trophic changes in the distal foot [4].
In some cases, stress tests can be additionally used to verify the diagnosis of obliterating atherosclerosis of the arteries of the lower extremities. Standard treadmill test
carried out for no more than 5 minutes or until discomfort in the heart area, shortening of breathing, shortness of breath or severe pain in the legs appears. The tonometer cuff for determining the pressure in the arteries of the leg, applied before the examination, remains on the patient throughout the examination. Immediately after the end of the stress test, after 2.5 and 5 minutes, the pressure in the arteries of the lower leg is measured [9].
Ultrasound duplex scanning
. The advantage of the method is the possibility of non-invasively obtaining an image of a vessel in real time with registration of the Doppler curve in a selected area of the vessel in any plane. The method allows you to determine the diameter of the vessel and the thickness of its walls, visualize additional echo formations in the lumen, evaluate hemodynamic parameters - linear and volumetric blood flow velocities, resistance indices.
Duplex scanning combines 2 modes: two-dimensional gray scale echography - B-mode and one of the Doppler modes. The study of the arteries of the lower extremities is carried out with a linear sensor operating in the frequency range from 5 to 10 (15) MHz. Increasing the scanning frequency is advisable for studying the vessels of the distal sections - the foot [10].
The atherosclerotic process is accompanied by structural and functional changes in the tissues of the heart and peripheral vascular system. A marker for early diagnosis of the preclinical stage of the atherosclerotic process is the thickness of the intima-media complex of the carotid arteries (IMC). In a large epidemiological study, the Atherosclerosis Risk in Communities
(ARIC), which included more than 14,000 men and women aged 45–64 years, the IMT thickness of patients with diabetes was 0.08 mm greater than that of persons without carbohydrate metabolism disorders matched by gender, age, nationality, smoking habit, and BMI . Also, in patients with fasting hyperglycemia and hyperinsulinemia without diabetes, the IMT thickness was 0.02 mm greater than in the healthy population [11].
Another indicator determined using duplex ultrasound scanning and reflecting the early stages of the atherosclerotic process is Young’s Modulus, which allows you to evaluate the elastic-tonic properties of the arterial wall. G.I. Kuntsevich et al. showed that Young's Modulus and IMT can serve as markers of the development and progression of the atherosclerotic process in patients with diabetes [2,12].
In the last decade, there has been great interest in studying the vasoregulatory function of the endothelium in atherosclerosis and its risk factors (obesity, arterial hypertension). To assess the vasodilatory function of the endothelium, two methods are currently used in clinical studies. The first method is chemical stimulation of endothelial muscarinic receptors with acetylcholine, which is injected into the artery and causes endothelium-independent vasodilation (EIVD), measured using veno-occlusive plethysmography (VOP). The second method is mechanical stimulation of the endothelium with increased blood flow, which is assessed by changes in the diameter of the artery (usually the brachial artery) using high-resolution ultrasound. The essence of the first method is to assess forearm blood flow with the help of a VOP when endothelium-stimulating drugs (acetylcholine, methacholine, substance P) and direct vasodilators (nitroglycerin, sodium nitroprusside) are introduced into the brachial artery. However, this invasive method is less convenient for repeated studies of the dynamics of endothelial dysfunction, as well as for early detection of impaired endothelial function in individuals with risk factors, even before the appearance of clinical signs of the disease [13].
The one developed by Celermajer et al. has found widespread use. in 1992, a non-invasive method for determining the vasoregulatory function of the endothelium by flow-induced dilatation using high-resolution ultrasound
compared with endothelium-independent vasodilation (ENIVD) after sublingual nitroglycerin administration [14,15,16]. It is based on the fact that, under the influence of a physical or chemical stimulus, the endothelium regulates vascular tone by releasing vasoconstrictor and vasodilator substances, such as endothelin and nitric oxide, respectively. Mechanical stimulation of the endothelium of the brachial artery in a test with reactive hyperemia gives an idea of the state of EDVD. Flow-induced vasodilation is assessed by changes in brachial artery diameter. A decrease in endothelial dysfunction reflects endothelial dysfunction, which is usually associated with the presence of risk factors for CAD.
Table 1 lists several clinical studies examining EDVD in patients with diabetes [17]. Most studies have found impaired brachial artery EDVD along with preserved EDVD in response to nitrates, but some studies have found impaired endothelial response in both cases. Isolated damage to the endothelial response at the onset of diabetes, which is accompanied by impairment of the smooth muscle cell response as the disease progresses, may explain the differences in the results obtained. This hypothesis is confirmed by the detection of endothelial dysfunction in individuals with metabolic syndrome (insulin resistance). Detection of vasoconstriction during a test with reactive hyperemia in patients with diabetes may indicate the presence of structural pathology of the heart and blood vessels and left ventricular hypertrophy and/or atherosclerotic lesions [18].
A significant event in the development of duplex ultrasound scanning was the use of color duplex mapping, which makes it possible to obtain information about blood flow in those vessels that cannot be visualized using duplex scanning. The diagnostic value of the method increases by an order of magnitude [19,20].
Transcutaneous oximetry (Tc pO2)
refers to methods for assessing microhemodynamics.
Transcutaneous measurement of oxygen tension makes it possible to assess the functional state of the vascular system, i.e. the presence of adequate collateral blood flow, determine the degree of tissue ischemia, and make the right choice between conservative and surgical treatment. Knowing the degree of oxygen saturation, it is possible to predict the possibility of healing of an ulcer (Table 2) [4]. The accuracy of the test depends on a complex of systemic (fractional oxygen concentration in inspired air, the state of the pulmonary system, blood hemoglobin level and cardiac output) and local (skin thickness, capillary bed architecture and the presence or absence of inflammation and edema) factors. The idea of bloodless measurement of oxygen content in the skin was first implemented in 1951 by M. Baumberger and R. Goodfriend, who used a mercury drop-shaped electrode in a heated buffer solution into which the patient’s finger was placed.
At the same time, it was possible to discover that the oxygen tension (pO2) in the buffer solution approaches the pO2 value of arterial blood. However, due to its complexity and insufficient accuracy of the data obtained, this technique was not used in clinical practice at that time. Its new possibilities opened up after the invention of monitors with a modified Clark-type electrode for long-term determination of pO2 with a special heating device. The local reactive hyperemia created with the help of heat causes a local increase in blood circulation and diffusion of gases through the electrode membrane. The transcutaneous oxygen tension (Tc pO2) measured by such an electrode reliably correlates with arterial blood pO2 in both newborns and adults, and quantitatively characterizes skin blood flow. The ability to study skin blood flow and its changes using these devices has contributed to the widespread use of this technique in the examination of patients with obliterating diseases of the vessels of the lower extremities. In 1978, A. Tonnesen found that with lesions of the peripheral arteries of the lower extremities, there is a significant decrease in Tc pO2 compared to arterial blood pO2. In addition, he revealed a correlation between the severity of chronic arterial insufficiency and Tc pO2 [9]. In 1984, Hauser et al. supplemented the method for measuring Tc pO2 [21]. The results obtained in patients with limb ischemia in the standing, supine, and leg elevation positions were compared to determine the severity of the lesion, predict the likelihood of healing of the ulcer, and select the level of amputation required. The local perfusion index (RPI) was calculated for each extremity, which is defined as the ratio of the transcutaneous oxygen tension in the lower extremity to the indicator on the chest, multiplied by 100. The study showed that in patients with asymptomatic COPD, the elevated position was more reliable. limb, while in patients with 3–4 tbsp. ischemia, no significant difference in the results was obtained. The advantage of the method of measuring Tc pO2 compared to the method of measuring segmental pressure in the arteries of the leg in patients with diabetes mellitus was also revealed.
The previously widely used method of rheovasography is currently recognized as uninformative, and conducting this study in patients with diabetes mellitus is inappropriate.
«The gold standard
Radiocontrast angiographic examination
remains the only method for diagnosing obliterating diseases of the vascular bed .
With its help, it is possible to accurately determine the location, extent, degree and nature of stenosis, the multiplicity of occlusive lesions of the main arteries of the lower extremities, assess the condition of the collateral bed, predict the nature and volume of reconstructive surgery, and also monitor the effectiveness of treatment and surgery. Also recently, magnetic resonance angiography
, which has high resolution, has become widespread.
Treatment of macroangiopathy
Since diabetes is a combination of several cardiovascular risk factors (hyperglycemia, dyslipidemia, arterial hypertension, smoking, overweight), it is believed that measures to eliminate and correct them should begin early and more actively. The principle of actively influencing risk factors applies to both non-pharmacological preventive measures and the prescription of medications. An indispensable basic condition for conservative and surgical treatment is compensation of carbohydrate metabolism.
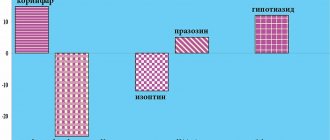
One of the most important tasks in the treatment of patients with ischemic heart disease and diabetes is antianginal therapy.
. Prevention/elimination of painful attacks in patients with stable angina pectoris significantly improves the quality of life of patients. Currently, drugs from the group of nitrates, b-blockers, and calcium antagonists are used. Traditionally, treatment of angina begins with the administration of nitrates, which improve exercise tolerance. With the advent of new selective beta-blockers (nebivolol), their previously described negative effects (deterioration of the lipid profile, smoothing out the sensation of hypoglycemia) are usually insignificant, and at present, diabetes is not considered a contraindication to the use of this group of drugs. It should be noted that nebivolol differs markedly from a number of traditional b-blockers in that it stimulates the synthesis of endogenous NO in endothelial cells, thereby causing relaxation of smooth muscle cells in the arteries and physiological vasodilation.
The next important step in the treatment of diabetic macroangiopathy is the correction of lipid metabolism disorders
. Monitoring serum lipid levels should be carried out upon initial consultation with a doctor, if a normal lipid spectrum is detected - annually, and if hyperlipidemia is detected - once every 3 months. If, while following a diet with limited animal fats, losing weight, eliminating risk factors, achieving compensation for carbohydrate metabolism, the level of total cholesterol exceeds 4.8 mmol/l, and triglycerides exceed 1.7 mmol/l (European Diabetes Policy Group, 1998–1999), then taking lipid-lowering drugs is recommended. Currently, there are several groups of drugs that normalize the lipid spectrum of the blood (Table 3).
Radical therapy for treatment-refractory hyperlipidemia includes surgical methods (small intestinal bypass, LDL plasmapheresis) [22].
The next important step is the correction of blood coagulation disorders
. Due to the increased risk of thrombosis and thromboembolism in diabetes, in cases where there are indications for prescribing anticoagulant therapy to patients with diabetes, it should be carried out taking into account all indications and contraindications and monitoring the progress of treatment. Such a common drug as acetylsalicylic acid has good antithrombotic properties. In light of the currently available data, antiplatelet therapy using acetylsalicylic acid, which inhibits the production of thromboxane by platelets, is the most accessible means of preventing thrombotic complications. Other drugs that affect the rheological properties of blood include pentoxifylline and dipyridamole. Data from multicenter studies show that the use of antiaggregation therapy as a strategy for secondary prevention of the development of coronary artery disease and COAD will reduce the incidence of cardiovascular diseases by 25%, myocardial infarction by 30%, and mortality by 15%, respectively [23]. In recent years, therapy with prostanoids (alprostadil) and anticoagulants (heparin, sulodexide, fraxiparin) has become widespread. The widely used early heparin is a direct anticoagulant that directly affects blood coagulation factors and reduces platelet aggregation. It belongs to a group of drugs with antithrombin activity, the action of which is mediated by endogenous cofactors, mainly AT III. Antithrombins are prescribed to prevent the development of thrombotic complications. Currently, much attention is paid to the use of low molecular weight heparins (sulodexide, fraxiparin) in the treatment of blood coagulation disorders in patients with diabetes. They have complex anticoagulant activity (blockade of the coagulation cascade at earlier stages, inhibition of von Willebrandt factor release, increased release of tissue factor inhibitor), which allows us to hope for their higher effectiveness. In patients with diabetic macroangiopathy, who are at high risk of thrombotic complications, low molecular weight heparins are the mainstay of treatment with an antithrombin mechanism of action.
A highly effective method of conservative treatment of patients with COPD and DM of the foot is intravenous administration of prostaglandin E1
. The drug has a vasodilating effect, reduces platelet aggregation, and increases the fibrinolytic activity of plasma. About 60% of patients report marked clinical improvement during treatment. If the phenomena of critical ischemia are stopped by the primary course, then the patient is transferred to standard disaggregant therapy. Moreover, indications for long-term infusion of prostaglandin E1 preparations (for up to 30–40 days) arise very often in patients with an ischemic form of diabetic foot against the background of total occlusion of the arteries of the leg and foot, when it is not possible to perform standard reconstructive surgery on the main arteries of the limb. Based on this, the possibility of using prostaglandin E1 drugs in terms of preventing amputation and in complex therapy of patients with damage to the main arteries of the lower extremities becomes clear.
The presence of diabetes, a consequence of the diffuse nature of arterial lesions, the high frequency of restenosis after stenting and occlusion of bypasses, worsens the surgical and postoperative prognosis for coronary angioplasty, coronary artery bypass grafting (CABG), percutaneous balloon angioplasty, stenting and prosthetics of lower extremity vessels. According to the results of retrospective studies, it is preferable to undergo CABG in patients with diabetes and coronary artery disease.
. If the patient has iliac artery stenosis, transluminal angioplasty is performed. Prolonged stenoses or occlusions with preserved outflow tracts are an indication for standard bypass operations: aorto-femoral, femoral-popliteal, femoral-tibial bypass. With a distal form of damage to the arterial bed of the limb, patients can undergo arterialization of the venous blood flow of the foot.
In conclusion, it should be emphasized the need for early diagnosis of diabetic macroangiopathy and timely administration of adequate pathogenetic therapy in order to prevent the progression of the atherosclerotic process.
Treatment of diabetic macroangiopathy should be comprehensive. Along with the correction of metabolic disorders (hyperglycemia, dyslipidemia), strict control of blood pressure levels, the prescription of combination antihypertensive therapy to achieve the target blood pressure level, the exclusion of other risk factors for the progression of atherosclerosis, and the use of drugs that improve the rheological properties of blood are necessary. Literature:
1. Dedov I.I., Shestakova M.V. Diabetes mellitus.//Universum publishing Moscow, 2003.
2. Kuntsevich G.I. Ultrasound diagnostics in abdominal and vascular surgery//Minsk, 1999.
3. Stamler J, Vaccaro O, Neaton DJ. et al.//Diabetes Care, –1993; –16, –pp. 434 – 444.
4. Dedov I.I., Antsiferov M.B., Galstyan G.R., Tokmakova A.Yu. Diabetic foot syndrome.//M.: Federal Diabetology Center of the Ministry of Health of the Russian Federation, 1998.
5. Jude EB, Oyibo SO, Chalmers N, Boulton AJM. Peripheral arterial disease in diabetic and nondiabetic patients.//Diabetes Care, –2001; –24, –pp. 1433 – 1437
6. Kannel CW et al. Fibrinogen and risk of cardiovascular disease: The Framingham Study.//JAMA, –1997; –258, –pp. 1183–1186.
7. TransAtlantic Inter–Society Consensus (TASK). Management of peripheral arterial disease.//J Vasc Surg, –2000; –1 (suppl) 1 – 296.
8. Hertzer NR, Beven EG, Young JR, et al. Coronary artery disease in peripheral vascular patients: a classification of 1000 coronary angiograms and results of surgical management.//Ann Surg, –1984; –199, –pp. 223 – 233.
9. Levin and O'Neal's. The foot diabetic. – 6th edition/ edited by JH Bowker, MA Pfeifer. 2001.
10. Lelyuk V.G., Lelyuk S.E. Ultrasound angiology.//M.: Realnoe Vremya, 1999.
11. Folsom AR, Eckfeldt JH, Weitzman S, et al. Relation of carotid artery wall thickness to diabetes mellitus, fasting glucose and insulin, body size, and physical activity.//Stroke, –1994; – 25, –pp. 66 – 73.
12. Kuntsevich G.I., Barabashkina A.V. Assessment of the condition of the arterial bed in patients with diabetes mellitus using color Doppler mapping and pulsed Dopplerography.//M., 1998.
13. Zateyshchikova A.A., Zateyshchikov D.A. Endothelial regulation of vascular tone: research methods and clinical significance.//Cardiology, –1998; – 9, –s. 68–80.
14. Celermajer DS, Sorensen KE, Gooch VM et al. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis //Lancet, –1992; –Vol. 340, – pp. 1111–1115.
15. Celermajer DS, Sorensen KE, Spiegelhalter DJ et al. Aging is associated with endothelial dysfunction in healthy men years before the age–related decline in women //J. Amer. Coll. Cardiology, –1994; –Vol. 24, –pp. 471–476.
16. Corretti MC, Anderson TJ, Benjamin EJ, Celermajer D, Charbonneau F, Creager MA, Deanfield J, Vallance P, Vita J, Vogel R. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery. A Report of the International Brachial Artery Reactivity Task Force.//J Am Coll Card, –2002; –vol 39, – pp. 257 – 265.
17. Storey AM, Perry CJ, Petrie JR. Endothelial dysfunction in type 2 diabetes.//The British J of Diabetes and Vascular disease, –2001; –Vol 1, Issue 1, –pp. 22 – 27.
18. Karpov R.S., Koshelskaya O.A., Tarbokova A.Yu., Efimova E.V., Atroshenkov A.V., Gruzdeva O.V., Semina E.A. Macrovascular reactivity in patients with type 2 diabetes mellitus in combination with arterial hypertension.//Diabetes mellitus, –2001; –2, –s. 37 – 39.
19. Hatsukami TS, Primozich SF, Zierler RE. Color Doppler imaging of infrainguinal arterial occlusive disease//J Vasc Surg, –1992; 16, –pp. 51 – 56.
20. Vascular Surgery//Ed. R. B. Rutherford. – Philadelphia: WB Saunders. – 1995. – Vol. 1–2. – 2033 p.
21. Hauser CJ, Klein SR, Hehringer CM, et al. Superiority of transcutaneous oximetry in noninvasive vascular diagnosis in patients with diabetes.//Arch Surg, –119: 690, – 1984.
22. Aronov D.M. Treatment and prevention of Atherosclerosis // M.: Triad X, 2000, – p. 18–21.
23. Colwell JA. Aspirin therapy in diabetes [position statement].//Diabetes Care, –1997; – 20, –pp. 1772 – 1773.
Prevention of diabetes complications:
- correct treatment regimen - correctly selected drug and dose (sugar levels are always normal);
- fulfilling all doctor's orders;
- weight normalization;
- normal motor activity;
- sufficient sleep;
- balanced diet;
- regular examinations by an endocrinologist, vascular surgeon, neurologist, ophthalmologist, podologist, nephrologist.
Professional medical supervision, patient self-discipline and a healthy lifestyle can reduce diabetes complications to a minimum or even prevent them altogether.
Damage to large vessels in diabetic angiopathy
In diabetic angiopathy, medium and large vessels can be affected. The inner membrane thickens in them, calcium salts are deposited and atherosclerotic plaques form.
The manifestations of the disease in this case are similar to those that occur with damage to small arteries. Pain in the feet bothers you, they become cold and pale, the nutrition of the tissues is disrupted, and they die over time. Gangrene of the fingers and then the feet develops. Diabetic angiopathy of internal organs
In diabetes mellitus, the pathological process most often affects the vessels of the retina and internal organs. This occurs due to the formation of toxic products due to incomplete “burning” of glucose. Almost all patients with high blood glucose levels have a retinal disease called retinopathy. With this disease, visual acuity first decreases, and then blood flows into the retina, and it peels off. This leads to complete loss of vision.
The second target organ whose vessels are affected in diabetes mellitus is the kidneys - nephropathy develops. In the initial stages, the disease does not manifest itself in any way; changes can only be detected during examination of the patient. Five years later, kidney function is impaired and protein appears in the urine. If changes are identified at this stage, they may still be reversible. But in the case when treatment is not carried out, the pathological process in the vessels of the kidneys progresses, and after ten years visible signs of the disease appear. First of all, a large amount of protein begins to be excreted in the urine. There is less of it in the blood, and this leads to the accumulation of fluid in the tissues and swelling. Initially, swelling is visible under the eyes and on the lower extremities, and then fluid accumulates in the chest and abdominal cavities of the body.
The body begins to use its own protein substances for life, and patients lose weight very quickly. They feel weak and have a headache. Also at this time, blood pressure rises, which stubbornly remains at high levels and does not decrease under the influence of medications.
The final stage of diabetic kidney angiopathy is the final stage of renal failure. The kidneys almost completely fail, they do not perform their function, and urine is not excreted. The body is poisoned by products of protein metabolism.