Detailed description of the study
Pancreatic lipase is a water-soluble enzyme that catalyzes the reactions of digestion of neutral fats (triglycerides) in the initial part of the small intestine - the duodenum. The biochemical feature of lipase is that this enzyme can perform its function without coenzymes - derivatives of vitamins, nucleotides, heme, etc.
The process of digestion of triglycerides begins in the lumen of the stomach with the help of lingual lipase, which is produced in the glands of the tongue and enters the stomach along with saliva. However, the main stage of digestion of neutral fats begins in the small intestine. Pancreatic lipase is formed in the pancreas and, as part of pancreatic juice, is secreted through the duct into the lumen of the duodenum together with colipase. This protein indirectly accelerates the action of lipase, so that fats begin to break down faster.
Before digestion, fats sequentially pass through the emulsification stage. Bile produced in the liver directly produces this process - the integrity of the neutral fat molecule is disrupted, as a result of which triglycerides are repeatedly mixed with water in the lumen of the small intestine and crushed into small fat droplets. After this, the process of hydrolysis begins with the participation of pancreatic lipase.
With pancreatitis, the outflow of pancreatic juice into the duodenum is disrupted. The large amount of lipase and other enzymes remaining in the gland, which have pronounced biological activity, leads to inflammation of the “self-digestion” type - the enzymes destroy the anatomical structure of the pancreas and become the main cause of the development of inflammation. In this case, a significant part of the lipase begins to enter the blood. In addition, lipase together with calcium leads to extensive damage to the pancreas (pancreatic necrosis).
Another enzyme, alpha-amylase, is also a marker of pancreatitis. This protein is formed in the cells of the salivary glands and pancreas; it is involved in the hydrolysis of carbohydrates. With pancreatitis, the pancreatic form of amylase in the blood increases, and salivary amylase levels remain within normal values. Accordingly, hyperfermentemia (increased lipase or amylase in the blood) by more than three times is one of the key signs of acute pancreatitis.
In the context of diagnosing acute pancreatitis, lipase is a more specific enzyme than amylase. An increase in the level of lipase in pancreatitis is observed approximately 4-8 hours after the onset of the disease, amylase - 2-12 hours. In this case, the level of lipase in the blood, as a rule, increases to a greater extent and can remain elevated much longer compared to amylase (7-10 days / 3-4 days). It has also been found that in about 20% of patients, the concentration of serum amylase can remain within normal limits. This property is not typical for lipase.
Also, the level of serum pancreatic lipase may be increased in diseases of the hepatobiliary region and systemic diseases leading to secondary damage to the pancreatic gland.
Indications
The main indications for assessing the level of digestive enzymes are symptoms of acute pancreatitis:
- pain in the left hypochondrium, spreading to the entire abdomen and lower back,
- uncontrollable vomiting,
- a sharp increase in temperature.
People who have been diagnosed with chronic pancreatitis or a tumor of the pancreas should also regularly undergo lipase concentration assessments. The test results will help the doctor evaluate the effectiveness of the prescribed treatment, as well as exclude exacerbation of the inflammatory process or rapid growth of the tumor.
It is also necessary to take a lipase test if symptoms of the following diseases appear:
- cholecystitis, other gallbladder pathologies,
- renal failure,
- liver cirrhosis.
Lysosomal acid lipase deficiency (LALD)
ICD-10 code for this disease: E75.5 Other lipid storage disorders
. DLCL is a rare inherited lysosomal storage disease that can affect people of all ages (first clinical manifestations have been reported from birth to 68 years of age) and has a highly variable clinical presentation. The disease is inherited according to an autosomal recessive mode of inheritance, its prevalence is 1:40,000–1:300,000, according to world data [3], while the expected incidence in the Russian Federation is 1:100,000 [4].
The disease is based on impaired activity of lysosomal acid lipase (LAL), caused by mutations in the lipase A gene ( LIPA
). LCL is the only known enzyme active at acidic pH in the lysosome, under the action of which cholesterol esters (CS) and triglycerides undergo hydrolysis to form free fatty acids and free cholesterol in the cell. The essential role of LCL in lipid metabolism has been confirmed in mice and humans with LCL. Recent studies have revealed the regulatory role of lipolytic products of lysosomal lipid hydrolysis in catabolic, anabolic and signaling pathways [5].
DLCL is characterized by minimal residual LCL activity in children and adults, resulting in a severely impaired ability to hydrolyze cholesterol esters and triglycerides, and a complete absence of LCL activity in infants, causing a more rapidly progressive and fatal course of the disease at a very early age. The intracellular accumulation of lipids throughout the body causes numerous and extremely varied clinical manifestations [6], which depend on the form of DLCL and are similar to the clinical picture of many other diseases, both rare and frequently encountered in clinical practice.
Introduction
The problem of early diagnosis and the possibility of pathogenetic treatment of rare (orphan) diseases throughout the world, including our country, is extremely relevant.
To date, about 6-7 thousand rare diseases have been discovered, and new ones are regularly described in the medical literature [1]. Most are inherited and caused by changes or defects in genes (mutations), while others can be acquired as a result of environmental exposures and toxic conditions. Despite the different clinical picture of orphan diseases, patients are united by a common problem: due to a number of obstacles, diagnosing the disease, and therefore the possibility of starting pathogenetic treatment, is extremely difficult. For example, for one third of people with rare diseases, obtaining an accurate diagnosis can take anywhere from 1 to 14 years [2]. Patients often have to go a long way to finally find a doctor who knows about their disease and can provide qualified care, and the costs associated with this search can be colossal. The task of timely diagnosis and treatment of rare diseases is especially relevant for pediatrics, in particular for medical specialists providing medical care to the child population, due to the fact that more than 50% of orphan diseases manifest themselves in childhood [1]. However, there are often cases when the disease progresses almost asymptomatically until adulthood and manifests itself as irreversible damage to organs and systems.
The availability of modern and highly sensitive methods for diagnosing many rare hereditary diseases (molecular genetic studies, enzyme diagnostics, etc.) allows practitioners to shorten the diagnostic path of a “rare” patient and make a diagnosis faster, which, of course, affects the effectiveness of treatment, since the disease does not have time to progress to irreversible conditions.
In the Russian Federation, diseases that have a prevalence of no more than 10 cases per 100,000 population are considered rare (orphan). For the first time at the state level, the concept of rare (orphan) diseases was introduced by Federal Law dated November 21, 2011 No. 323-FZ “On the fundamentals of protecting the health of citizens in the Russian Federation.”
Diagnosis and treatment
Without the doctor's vigilance and awareness of the disease, it can be difficult to suspect DLCL due to the similarity of the clinical picture with non-alcoholic fatty liver disease (NAFLD) and many other diseases of the liver and cardiovascular system. The main diagnostic method is enzymatic diagnostics - determining the activity of the LAL enzyme in dried blood spots. The combination of the clinical picture and sharply reduced activity of the acid lipase enzyme makes it possible to establish the diagnosis of DLCL. In this case, it is possible to conduct additional molecular genetic research and search for mutations in the LIPA
by sequencing [4].
Diet modifications, lipid-lowering medications, and liver transplantation have not been shown to be effective in treating or preventing the progression of DLCL because none of the above addresses the underlying cause of the disease. Hematopoietic stem cell transplantation in patients with DLCL has been poorly studied and is known to be associated with numerous complications [6, 8, 9]. Currently, pathogenetic treatment has been developed - lifelong enzyme replacement therapy with the drug sebelipase alfa, a recombinant human LCL that improves lipid metabolism in patients of all ages [11–13].
Interpretation of results
Self-diagnosis using laboratory tests is impossible; the clinical picture, circumstances of the disease and previous events are always taken into account. Only a doctor can make the correct conclusion by analyzing a wealth of knowledge and a specific situation. A doctor of any specialty can prescribe a test.
Reasons for the increase:
- pancreatitis (within 3 to 7 days from the onset the concentration reaches maximum values);
- gland tumors – both benign and malignant;
- chronic cholecystitis and other chronic diseases of the bile-forming and biliary system, including cholestasis;
- breakthrough or perforation of any organ located in the abdominal cavity;
- constriction (strangulation) of an intestinal loop, causing tissue necrosis;
- peritonitis;
- severe ischemia (oxygen starvation) or infarction of a section of the intestine;
- cyst or other cavity formation of the pancreas;
- endocrine and other diseases in which lipid metabolism is disrupted - diabetes, gout, obesity;
- long-term use of medications and narcotic drugs, resulting in spasm of the sphincter of Oddi - analgesics, barbiturates, heparin, indomethacin;
- “mumps” (mumps) with damage to the pancreas.
Reasons for the decline:
- cancer of any organ except the pancreas;
- hyperlipidemia, which is hereditary;
- cystic fibrosis, in which the gland undergoes cystic fibrosis;
- food with excess fat.
All laboratory services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Lipase: effect on the body
Enlarge image
When fats (animal or vegetable origin) enter the mouth of an adult with food, they do not undergo changes. And they come out of the stomach in almost the same form. Although the gastric juice contains lipase , its concentration is quite low. And the pH for enzyme activation is far from normal (5.5 - 7.5). It does not break down fats in the stomach, but greatly simplifies their further digestion in the intestines.
It's a different matter for infants. In response to sucking and swallowing movements, lipase , which helps quickly deal with the lipids contained in milk.
When chyme (semi-digested food) enters the small intestine, gastric acid is neutralized, after which the final fractionation of fat begins.
Some vegetables and fruits contain lipase . These foods are easier to digest and even help get rid of “bad fat” in the body. These include:
- avocado (avocado oil and fresh fruits);
- flax seeds;
- pumpkin seeds;
- nuts.
All these foods should be consumed raw.
Low lipase
In turn, low levels of lipase in the blood are a symptom of such ailments as:
- diabetes ,
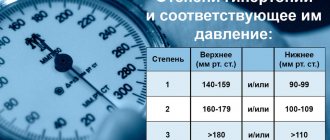
- hypertension,
- high cholesterol,
- Genetic hyperlipidemia (this is a very rare disease in which unhealthy high levels of body fat are determined entirely genetically and are not the result of poor diet and low physical activity, as is usually the case).
Vorobyova Marina
Neurologist of the highest qualification category (work experience 14 years), doctor of neurofunctional diagnostics (work experience 12 years); author of scientific publications on vertebroneurology; participant of scientific conferences on neurology and functional diagnostics of all-Russian and international significance.