The powerful lymph nodes located around the pharynx cannot cope with the attack of the pathogen, so the body begins to produce antibodies that can find pathogenic bacteria, paralyzing their activity.
As a result, streptococci are defeated, but the child’s body produces so many antibodies that, in addition to foreign cells, the body’s own tissues, primarily the heart and joints, begin to suffer. Therefore, it is always better to entrust the treatment of sore throat in a child to a qualified doctor.
In 10% of cases, sore throat in children can be caused by Staphylococcus aureus, rarely pneumococcus, Haemophilus influenzae, chlamydia and fungal flora. Viral pathogens (adenoviruses, herpes virus) more often attack the body of children under 3 years of age.
How and why does infection occur?
Infection occurs by airborne droplets, from a sick person, by using shared utensils and eating contaminated food, as well as by a number of other factors:
- weakened immunity;
- hypothermia or consumption of cold foods and drinks;
- mouth breathing (for chronic adenoiditis, deviated nasal septum);
- irritation of the nasopharyngeal mucosa with a runny nose;
- recent viral diseases;
- inflammatory diseases of the ENT organs (sinusitis, sinusitis, otitis);
- caries and other oral infections.
Secondary tonsillitis in children can occur against the background of scarlet fever, diphtheria, mononucleosis, as well as blood diseases.
In any case, a sore throat develops rapidly, in a matter of hours, and is especially acute in children, accompanied by the main symptoms—a sore throat when swallowing and an increase in body temperature.
What symptoms indicate a child has a sore throat?
To assume that a child has a dangerous form of streptococcal tonsillitis, one or more of the following symptoms must be present:
- Temperature ≥ 38.3°C
- Season: late autumn, winter or early spring.
- The child does not have a cough
- The child's age is from 5 to 15 years.
- Recent exposure to someone with a sore throat
- Difficulty breathing or swallowing
- The child's voice sounds muffled
- Stiffness in the neck or difficulty opening the mouth
Sore throat in children: forms and clinical manifestations
Depending on the nature of the change and the degree of damage to the tonsils, several forms of angina are distinguished.
Catarrhal sore throat
A mild form, characterized by enlargement and redness of the tonsils, as well as the absence of purulent lesions. The child feels dry mouth, a whitish coating appears on the tongue, and the cervical lymph nodes are slightly enlarged. In addition to a sore throat that gets worse when swallowing, the child feels a sore and burning sensation. The temperature rises to 38 degrees, children complain of weakness and headache.
Follicular tonsillitis
A serious disease in which the tonsils become covered with purulent pinpoint follicles. On days 2-3, the ulcers open, leaving wounds that heal quickly. There is severe pain in the throat, radiating to the ear, making it difficult to swallow, children refuse to eat and drink. The lymph nodes are enlarged and painful when pressed lightly. Fever and chills are accompanied by a temperature of up to 40 degrees, vomiting, convulsions and fainting are possible.
Lacunar tonsillitis
In the lacunae, between the lobes of the tonsils, islands of yellow purulent plaque appear, which tend to unite into wide purulent foci. The symptoms are similar to those of purulent follicular tonsillitis, but are more pronounced and are accompanied by severe intoxication of the body. It hurts the child to turn his head, his mouth opens with difficulty, which makes speech slurred.
Viral (herpetic) sore throat
Most often, the development of the disease is facilitated by vitamin deficiency and weakened immunity. The tonsils become covered with red blisters, which burst, leaving small ulcers in their place. In addition to a sore throat, symptoms are acute respiratory in nature: cough, runny nose, abdominal pain, indigestion, as well as stomatitis and conjunctivitis. Lack of timely treatment of herpetic sore throat in children can lead to serous meningitis.
Fungal tonsillitis
A relatively mild form of sore throat that occurs in children under 3 years of age. It is distinguished by a coating of white, curdled flakes on the tonsils and, with proper treatment, goes away within a week.
Antibiotics in the arsenal of a local pediatrician for the treatment of respiratory diseases
Although the diagnosis and treatment of respiratory pathology in children occupy a leading place in the work of a pediatrician, antibacterial therapy is required in almost only 6–8% of patients in this category - mainly with otitis, sinusitis, streptococcal sore throat, lymphadenitis, pneumonia, as well as bronchitis caused only by mycoplasma and chlamydia. Unfortunately, both here and abroad, the excessive use of these drugs has not been eliminated - they are sometimes used in 30–80% of children with acute respiratory viral infections (ARVI). Without bringing any benefit, this practice increases the risk of developing flora resistance and side effects, and also disorients the doctor: having not received the effect of an antibiotic for a viral infection, the doctor switches to reserve drugs, which also do not have an effect. Therefore, the main question is: are antibiotics indicated for this patient? — a positive decision should only be made for a proven (or probable severe) bacterial infection. And although it is rarely possible to prove the bacterial nature of acute respiratory diseases (ARI), the accumulated data allows the doctor with a high probability not only to identify such children, but also to outline the range of probable pathogens and their sensitivity to antibiotics. IN
forms of respiratory pathology are presented for which the prescription of an antibiotic is and is not indicated, as well as a symptom complex that allows one to suspect pneumonia in the absence of clear physical data, and the values of inflammatory markers for which the administration of an antibiotic is justified.
IN
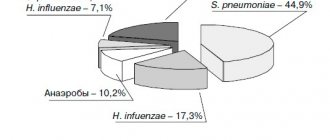
the main pathogens of bacterial acute respiratory infections are presented; It is obvious that the range of pathogens of acute respiratory infections in children is small, which facilitates the choice of a drug that acts on the probable causative agents of a particular disease. These data for antibiotics that should be used in outpatient settings are given in
.
Fortunately, penicillin resistance of pneumococci circulating among the Russian population (less than 10% of strains) is many times lower than, for example, in the countries of South-West Europe (40–50%). But it should be taken into account that among children in preschool institutions (preschool institutions) and especially in boarding schools, 50–60% of isolated pneumococcal strains are resistant to penicillin. Pneumococci remain 100% sensitive to amoxicillin (as well as ceftriaxone), but are resistant to co-trimoxazole, tetracycline, gentamicin and other aminoglycosides. Resistance of pneumococci to penicillins is not associated with the production of lactamase (it is caused by the loss of penicillin-binding proteins), therefore the use of inhibitor-protected penicillins does not increase the effectiveness of treatment. Resistance of pneumococci to macrolides is growing faster (up to 15–20% of strains in some regions); to a lesser extent, it is growing to 16-membered macrolides: josamycin, midecamycin, spiramycin.
Haemophilus influenzae (both non-capsular and type b) in Russia are sensitive to amoxicillin, doxycycline, 2nd and 3rd generation cephalosporins, and all aminoglycosides. But these pathogens are not sensitive to penicillin, cephalexin, cefazolin, and most macrolides - except for azithromycin (its use for otitis and sinusitis is limited by its low concentration in the corresponding cavities).
Under the influence of treatment, H. influenzae produces lactamases that inactivate lactam drugs (including penicillin and amoxicillin), therefore, in previously treated children (as well as in children from preschool education), amoxicillin/clavulanate or cefuroxime axetil are used from the beginning of treatment.
Group A beta-hemolytic streptococcus (GABHS) is sensitive to all antibiotics except aminoglycosides, but in some regions the frequency of macrolide-resistant strains can reach 15%. Moraxella catarrhalis, capable of producing lactamase, usually isolated from previously treated children, is sensitive to macrolides, cephalosporins, aminoglycosides, but resistant to amoxicillin.
Staphylococcus aureus rarely causes “outpatient” forms of respiratory tract damage (purulent sinusitis, cervical lymphadenitis); it is generally not sensitive to penicillins, there are strains resistant to cephalexin and amoxicillin/clavulanate, and its sensitivity to macrolides decreases rapidly if treatment lasts more than 5–7 days. The drugs of choice are cephalexin orally, and for more severe forms - oxacillin (parenteral), and in case of resistance to it - vancomycin.
In outpatient practice, drugs of first choice are prescribed if there is no reason to suspect the presence of drug resistance (
). For the vast majority of forms, oral forms of penicillins, cephalosporins of the first and second generations and macrolides are effective; they are most reliably administered in a pediatric dosage form - granules, Solutab dispersible tablets or syrup, which allows precise dosing.
The most used drug of first choice is amoxicillin (Flemoxin Solutab, etc.), it accounts (by weight) for 1/3 of all antibiotics produced in the world. Its bioavailability is higher than that of oral ampicillin, which has displaced the latter from the pediatrician’s arsenal. Other first-choice drugs: phenoxymethylpenicillin (Ospen syrup) and cephalexin are used only for the treatment of streptococcal tonsillitis, and macrolides are used for “atypical” infections (mycoplasmosis and chlamydia), as well as for the treatment of coccal infections in patients with allergies to penicillins.
second-choice drugs is started only in the case of previous (within the last 2–3 months) antibiotic therapy, as well as in case of nosocomial infection (in a child who became ill 1–3 days after discharge from the hospital). The most used drug is amoxicillin/clavulanate (Amoxiclav, Augmentin, Flemoklav Solutab), effective against both pneumo- and streptococci, as well as Haemophilus influenzae and Moraxella. Second-generation cephalosporins (cefuroxime axetil - Zinnat, which is much more active than cefaclor against pneumo- and streptococci) are also effective as second-choice drugs. Age-specific dosages are used, however, for amoxicillin/clavulanate and Zinnat, a number of instructions indicate underestimated (20–30 mg/kg/day) doses, which may be insufficient (see observation) - they should not be lower than 45–50 mg/kg/ days
Third-choice drugs (reserve, usually parenteral) are used only in cases of multidrug resistance, usually in a hospital setting.
are not used for respiratory pathology due to the increasing resistance of pneumotropic flora to them, as well as third-generation oral cephalosporins - ceftibuten (Cedex) and cefixime (Suprax), which may not be sufficiently active against coccal flora, in particular pneumococci.
Oral antibiotics are not used for severe acute processes. These include purulent sinusitis (occurs with swelling of the cheek or periocular tissue), it often requires surgical intervention, lymphadenitis with signs of purulent inflammation (adhesion to hyperemic skin, fluctuation). In children with croup, it is important to exclude epiglottitis - a bacterial inflammation of the epiglottis, which also causes inspiratory stridor as in viral croup, but with febrile temperature, intoxication, pain when swallowing in the absence of a barking cough, and dysphonia. Epiglottitis is characterized by increased dyspnea in the supine position, neutrophilic leukocytosis, and requires early intubation to prevent asphyxia. These diseases, as well as pneumonia complicated by pleurisy and destruction, require hospitalization, before which a broad-spectrum drug, ceftriaxone (80 mg/kg), should be administered parenterally, which should be in the emergency department and every local doctor.
In other cases, oral medications are used (). acute otitis media is suspected (or diagnosed by otoscopy), it is adequate to prescribe amoxicillin at a dose of 50 mg/kg/day, or amoxicillin/clavulanate at the same dose (overcoming the resistance of non-capsular hemophilus and moraxella), or, in a recently treated child, in a dose of 80–100 mg/kg/day of amoxicillin to overcome the possible reduced sensitivity of pneumococci in the middle ear cavity. In the latter case, it is advisable to use Augmentin or Flemoklav Solutab with a 7:1 ratio of amoxicillin and clavulanic acid. The duration of treatment is 10 days for children under two years of age and 7 days for older ones.
The same treatment tactics are effective for non-purulent bacterial sinusitis , which is diagnosed in the second or third week of acute respiratory infections while nasal congestion persists, often also fever, and pain in the projections of the sinuses.
Great difficulties arise in the treatment of acute tonsillitis , which in only 30% of cases is caused by GABHS, and in the rest by adenovirus or Epstein-Barr virus (infectious mononucleosis). They are equally characterized by an acute onset, fever with or without chills, sore throat when swallowing, hyperemia, swelling of the tonsils, often also of the uvula and soft palate, purulent detritus in the lacunae, plaque, enlarged lymph nodes (without suppuration). Streptococcal tonsillitis differs from viral tonsillitis in the absence of cough and catarrh, conjunctivitis, soreness of the lymph nodes and a drop in temperature 24–48 hours after the prescription of the antibiotic. Adenoviral tonsillitis is distinguished by conjunctivitis and nasopharyngitis, mononucleosis - nasopharyngitis, enlargement of the liver and spleen, and the appearance of wide-plasma lymphocytes in the blood. A positive culture makes the diagnosis of GABHS infection indisputable, as does an increase in antistreptolysin-O (ASL-O), therefore, such studies are indicated in all cases of acute tonsillitis.
In case of proven streptococcal tonsillitis, as well as in cases where the etiological diagnosis is unclear (especially in children over 6 years of age and in spring), one of the penicillins, cephalexin or macrolide is prescribed, which leads to a drop in temperature after 14–36 hours, confirming the diagnosis of streptococcal tonsillitis; in these cases, treatment should be continued for up to 10 days (for azithromycin - at a dose of 12 mg/kg/day - 5 days). If there is no effect, the antibiotic can be discontinued, leaving only symptomatic treatment.
If the lower respiratory tract is affected (its signs are tachypnea or dyspnea, the presence of wheezing, shortening of the percussion sound), it is important to differentiate viral bronchitis from pneumonia, in the vast majority of cases - bacterial.
Viral bronchitis, the most common form of damage to the lower respiratory tract (75–300 per 1000 children), is important to differentiate from bacterial pneumonia, the frequency of which is significantly lower (4–15 per 1000 children). This is all the more important because the complication of viral bronchitis, including bronchiolitis in infants, with bacterial pneumonia is extremely rare. A low-grade fever speaks against pneumonia (with the exception of chlamydial forms in the first months of life, in which the leading symptom is tachypnea) or if the initially febrile temperature drops to low-grade within 1-3 days. The abundance of wheezing typical for bronchitis or signs of obstruction are observed only with “atypical” mycoplasma pneumonia - they are asymmetrical and are often accompanied by a shortening of the percussion sound. Asymmetry of wheezing is also observed in bronchitis caused by mycoplasma, which is an indication for radiography. For typical (pneumococcal, hemophilus) pneumonia, if there is wheezing, it is local, often against the background of hard or weakened breathing over the lung area, often with shortening of the percussion sound (observation). Unfortunately, these local signs are not detected in all patients with pneumonia.
Thus, based on physical data, it is usually not difficult to exclude typical pneumonia and prescribe symptomatic therapy for viral bronchitis. If pneumonia is suspected (in the absence of threatening symptoms), the starting drug is amoxicillin 50 mg/kg/day, and in recently treated children amoxicillin/clavulanate 50 mg/kg/day or cefuroxime axetil - 40–60 mg/kg/day, which, As a rule, they give a quick effect. Lack of effect usually indicates an “atypical” etiology of pneumonia and requires changing the drug to a macrolide.
Infection with mycoplasma, which causes about half of all pneumonia in children over 5 years of age (it is difficult to draw a line between pneumonia and bronchitis with a loose pulmonary infiltrate), should be suspected in case of persistent (5–10 days) high temperature, usually with mild toxicosis (not causing severe anxiety for parents ), with mild catarrhal symptoms and conjunctivitis, with profuse, fine-bubble (as in infants with bronchiolitis) wheezing, but heard asymmetrically. A characteristic symptom is the lack of effect from the administration of amoxicillin and other lactam drugs; The administration of any macrolide in an age-related dose leads to apyrexia and a decrease in the symptoms of bronchitis within 1–3 days.
Local pediatricians often misinterpret the symptoms of these two types of pneumonia, prescribing “stronger” cephalosporins, which do not produce an effect, for more “noisy” (accompanied by an abundance of wheezing) atypical pneumonia, and “weaker” macrolides for typical pneumonia with a minimum of wheezing. In some cases of typical pneumonia, macrolides provide a quick effect, but due to the increasing resistance of pneumococcus, they may not have an effect. Therefore, one should strive to make starting appointments according to the more likely form of pneumonia. Relying on the detection, for example, of antibodies to mycoplasma is not reliable, since in the first week there may not yet be IgM antibodies, and PCR can detect the antigen in carriers.
To confirm or exclude a bacterial infection, so-called markers of bacterial inflammation are usually used - levels of leukocytosis, C-reactive protein, and, more recently, also procalcitonin. It is not uncommon to see a child with ARVI without visible bacterial foci, who receives antibiotics only because he has a leukocytosis of the order of 10–15 × 109/L. In most of these patients, ARVI progresses smoothly without the use of antibiotics. It has been proven that only leukocytosis > 15×109/l, absolute neutrophil count > 10×109/l and/or band > 1.5×109/l (as well as C-reactive protein (CRP) > 30 mg/l and procalcitonin > 2 ng/ml) more or less reliably indicate the possibility of a bacterial infection, while lower numbers are quite common in viral infections. Thus, in children with ARVI, bronchitis, croup, leukocytosis 10–15×109/l occurs in 1/3, CRP 15–30 mg/l – in 1/4 of patients. With tonsillitis caused by adenoviruses and the Epstein–Barr virus, in 1/3 of children, leukocytosis is in the range of 10–15 × 109/l, and 1/3 is above 15 × 109/l; CRP levels of 30–60 mg/l are detected in 1/4 of children, and in 1/3 - above 60 mg/l.
It should also be taken into account that with bacterial infections leukocytosis is not always observed: for example, with purulent otitis and typical pneumonia in 40% of patients, leukocytosis does not exceed 15´109/l, and with catarrhal otitis and atypical pneumonia - in 90%.
Literature
- Baranov A. A. (chief editor). Clinical recommendations. Pediatrics. Edition 2. M.: Geotar-Media. 2009.
- Baranov A. A. (ed.). Guide to outpatient clinical pediatrics. M.: Geotar-Media. 2006.
- Baranov A. A. Russian national pediatric formulary. M.: Geotar-Media. 2009.
- Union of Pediatricians of Russia. Scientific and practical program “Acute respiratory diseases in children. Treatment and prevention." M., 2002.
- Tatochenko V.K. Pneumococcal infection is an underestimated threat // Children's infections. 2008, no. 2.
- Tatochenko V.K. Antibiotic and chemotherapy of infections in children. M. IPK-Continent Press, 2008.
V. K. Tatochenko, Doctor of Medical Sciences, Professor
SCCD RAMS , Moscow
Table 1.
Table 2.
Table 3.
Table 4.
Observation
Nastya K., 4.5 years old, was admitted on the 4th day of illness, accompanied by a temperature of 39 °C and cough. Two doses of Flemoklav Solutab 15 mg/kg did not produce any effect.
On admission: obsessive cough, redness of the right cheek, shortening of the right lung above, no wheezing. Blood: L - 31.6 ´ 109/l, p/i - 29%, p/i 57%, ESR 36 mm/hour, CRP 60 mg/l, PCT 10 ng/ml.
A dose of Flemoklav Solutab 45 mg/kg led to a drop in T° by the end of the day, a rapid improvement in the condition and normalization of the picture in the lungs after 2 weeks. The course of treatment is 5 days.
Diagnosis: lobar pneumonia
Why is a sore throat dangerous?
As practice shows, only in half of the cases are enlarged tonsils and sore throat caused by purulent sore throat. Many diseases, such as diphtheria or Epstein-Barr virus, have symptoms similar to sore throat. Therefore, only a qualified doctor with modern diagnostic equipment and a well-equipped laboratory can accurately determine the disease and prescribe the necessary treatment.
Each causative agent of sore throat is sensitive to a certain type of antibiotics prescribed by a doctor depending on the diagnosis.
Remember!
Incorrect or untimely treatment of sore throat in children, as well as relying on folk remedies for “red throat” can lead to serious complications and irreversible consequences.
Delay in diagnosis and prolonged treatment provoke the development of rheumatoid arthritis, vascular diseases, heart diseases (including rheumatic endocarditis), renal failure and many chronic diseases leading to disability.
Complications of sore throat
The reason for the development of complications is often a late start of treatment, incorrect selection of antibiotics and a sharp weakening of the immune system2.
- Streptococcus has an allergenic effect on the body3, creates the preconditions for the development of nephritis (inflammation of the kidneys), myocarditis (inflammation of the heart muscle), rheumatism, manifested by the development of heart defects and inflammation of the joints, systemic connective tissue diseases, such as systemic lupus erythematosus, Sjogren's syndrome, systemic vasculitis , scleroderma.
- Aggressive streptococcus can penetrate from the tonsils into the surrounding tissues, causing the formation of paratonsillar and retropharyngeal abscesses, periadenitis (inflammation of the lymph nodes), phlegmon - diffuse purulent inflammation of the tissues.
- The list of complications of tonsillitis includes otitis (inflammation of the middle ear), sinusitis (damage to the paranasal sinuses).
- The infection can enter the blood, spread throughout the body and cause the formation of purulent foci in other organs (septicopyemia).
Sore throat and acute tonsillitis in children should be taken seriously.
Consultation with a pediatrician and ENT doctor is necessary in any case, even if at first glance the patient’s condition does not cause much concern!
Self-medication is fraught with the development of complications - all parents should understand this.
Up to contents
The information in this article is for reference only and does not replace professional advice from a doctor. To make a diagnosis and prescribe treatment, consult a qualified specialist.