Causes of cardiosclerosis
1. Functional disorders:
- Damage to the heart muscle as a result of inflammatory diseases.
- Hypoxia due to insufficient blood supply to the heart muscles due to narrowing of large cardiac vessels.
- Stretching of the walls of the heart, which leads to an increase in its volume.
2. Lifestyle and bad habits of the patient:
- Alcohol abuse and smoking.
- No, minimal or excessive physical activity.
- Repetitive stress.
- The habit of overeating and, accordingly, excess body weight.
Hereditary factors play an important role in the occurrence of the disease.
Classification of cardiosclerosis
According to the morphological principle, focal (most often occurs as a complication after myocardial infarction and myocarditis) and diffuse cardiosclerosis, in which the connective tissue spreads to the entire myocardium, are distinguished.
For etiological reasons, the following types are distinguished:
- Post-infarction. As a result of myocardial infarction, scars form at the site of necrotic damage, which reduces the contractility of the heart muscle. The more cases of myocardial infarction a patient has suffered, the more scar tissue is formed. The threat of chronic aneurysm increases due to protrusion of the walls of the heart muscle, which is stretched and weakened by connective tissue. Aneurysm rupture is associated with high mortality.
- Myocardial. Myocardial inflammation develops mainly in young patients with chronic allergic and infectious diseases. With this form, the right ventricle of the heart increases in volume and is insufficiently supplied with blood.
- Atherosclerotic. As a rule, it is the result of atherosclerosis of the coronary vessels and coronary heart disease. This form of the disease develops over a long period of time, because due to damage to blood vessels, heart cells do not receive enough oxygen, hypoxia develops, the course of coronary heart disease is complicated, and cholesterol levels increase. This leads to diffuse cardiosclerosis, which is accompanied by arrhythmia.
Treatment
Conservative treatment of atherosclerotic cardiosclerosis is aimed at eliminating the symptoms of ischemia, correcting blood composition, improving blood circulation, increasing the density and elasticity of arterial vessels.
In advanced stages of the disease, drug therapy is inappropriate. To restore hemodynamics, the patient undergoes surgery to correct the arteries. Regardless of the chosen treatment tactics, the medical diet “Table No. 10” is prescribed, intended to eliminate hypercholesterolemia.
Groups of medications
Prescribed drugs are divided into several pharmacological groups:
How to lower blood cholesterol levels?
- Statins. Slow down the production of endogenous cholesterol. As a result, the level of LDL decreases and the content of HDL in the blood compensatory increases.
- Fibrates (fibric acid derivatives). Normalize lipid metabolism and the balance of lipoproteins of different densities.
- Calcium channel blockers and angioprotectors. They tone the walls of the arteries, strengthen the endothelium, and enhance the contractility of blood vessels.
- Anticoagulants and antiplatelet agents. Reduce high blood clotting rates characteristic of coronary artery disease and its manifestations.
- Bile acid sequitrants. Stimulate hepatocytes to use excess low-density lipoproteins for bile synthesis.
- Cardiac glycosides are plant stabilizers of rhythmic myocardial contractions.
- Vitamin PP (nicotinic acid) is an active participant in lipid metabolism.
- Nitroglycerin preparations for the relief of angina attacks.
At the same time, hypertension, metabolic disorders and other chronic diseases are treated.
Diet therapy
Diagnosed atherosclerosis, as a trigger for cardiovascular pathologies, is poor eating behavior, nicotine addiction, and addiction to alcoholic beverages. First of all, cardiologist patients are advised to review their diet, quit smoking, and give up alcohol.
The diet for atherosclerotic cardiosclerosis excludes the consumption of foods rich in animal fats, baked goods, smoked products, sausages, fast food, and pickles. It is prohibited to eat foods prepared by frying (including over charcoal).
Dietary nutrition is organized on the basis of slow carbohydrates (dishes from legumes, grains and cereals), fiber and vitamins (vegetables, herbs, berries, fruits), foods rich in Omega acids (linseed oil, fish, seafood, nuts). The rules of the diet indicate adherence to the eating regimen (every 3-4 hours in small portions).
A short list of products for atherosclerotic disease
Beverage classification
| Refuse | Introduce into your diet on a regular basis |
| coffee | freshly squeezed fruit and vegetable juices |
| alcohol (any strength) | berry compotes and jelly |
| energy | decoctions of rosehip, linden |
| sweet cocktails and juices |
When compiling a daily menu, special attention should be paid to compliance with the daily calorie intake and the ratio of nutrients.
Surgical intervention
With intense negative dynamics of the disease, surgical methods are used in treatment. Depending on the progressive changes, one of the following types of surgery may be prescribed:
- coronary bypass surgery - creation of an artificial channel for blood flow bypassing the atherosclerotic section of the coronary artery;
- aneurysm resection – excision of the damaged area of the aorta of the heart followed by prosthetics;
- RFA (radiofrequency ablation) – endoscopic cauterization of a section of the myocardium that blocks cardiac impulses;
- angioplasty of coronary vessels with stenting - dilation of arteries by installing a wall.
In difficult cases, an electrical pacemaker (ECS) is implanted.
Symptoms of cardiosclerosis
Very often the initial stages of the disease are asymptomatic. In the clinic of the onset of sclerosis, the first symptom may be arrhythmia. Typical manifestations of the diffuse form should be considered heart failure and disturbances in the rhythm of the heartbeat.
Symptoms regardless of the form (post-infarction or atherosclerotic):
- heart rhythm disturbances;
- dyspnea;
- the appearance of fluid in the abdominal and pleural cavities;
- pain in the heart area;
- increased heart rate;
- pulmonary edema;
- increase in liver size.
As the area of affected heart tissue increases, the severity of symptoms increases.
Very often the course of cardiosclerosis is accompanied by arterial hypertension. In this case, high blood pressure alternates with long periods of normal blood pressure.
Expert advice
I always tell patients about the high risk of recurrence of a vascular accident in order to create motivation for lifestyle correction. An important criterion is to bring the body mass index and abdominal circumference to standard values - 18.5-24.9 kg/m2 and 80 cm, respectively. Taking care of your health is a guarantee of a long and happy life!
Drug therapy
Treatment of post-infarction cardiosclerosis in the presence or progression of signs of myocardial ischemia involves the administration of nitrates. Their use is justified both on an ongoing basis and during attacks. Long-acting nitro drugs (“Nitrolong”, “Isosorbide dinitrate”) and symptomatic ones (for chest pain) are recommended. To stop a seizure, Nitrospray and regular Nitroglycerin are indicated.
The presence of arterial hypertension is an indication for antihypertensive therapy, which includes at least 2 groups of drugs from the main ones:
- ACE inhibitors and AARs (“Enalapril”, “Valsartan”, “Captopril”). They act at the level of the renin-angiotensin-aldosterone system, quickly and lastingly reduce blood pressure, and prevent myocardial remodeling.
- Diuretics - reduce blood pressure by removing fluid from the body, indicated for edema. Thiazide (“Indapamide”) and loop (“Furosemide”, “Torasemide”) are usually used.
- Beta blockers (Bisoprolol, Atenolol, Metoprolol, Nebivalol, Carvedilol) - reduce the total peripheral resistance of the vascular bed, reduce heart rate and weaken the strength of contractions of the heart muscle, promoting relaxation and rest of the myocardium. They are a means of preventing tachyarrhythmias.
- Calcium antagonists - relax the muscular wall of the arteries and have a mild diuretic effect. More often, drugs of the dihydroperidine series are prescribed (Nifedepine, Corinfar, Lacidipine).
To reduce the severity of oxygen starvation and increase the functionality of organs, antihypoxants are used. The only remedy with a proven effect is Preductal. My patients already notice an improvement in mental and associative processes, memory activation, and improved mood within 3-5 days. Mexidol has proven itself to be excellent in neurology.
Atherosclerosis occurring in the post-infarction period should be the reason for prescribing statins (Rosuvastatin). Fibrates and blockers of cholesterol absorption in the intestine (Ezetrol) are used less frequently.
For severe heart failure, glycosides are used. Medicines of this pharmacological group increase the activity of myocytes and slightly reduce the frequency of contractions.
Glycosides cause the heart to work to the detriment of its own condition. For some time, heart failure stabilizes, and then the myocardium is completely depleted, circulatory disorders increase and death from cardiogenic shock may occur. Consequently, such medications are used in exceptional cases, or in extremely small doses.
All patients undergo prophylaxis of thromboembolic complications. Anticoagulants are used (Heparin, Xarelto).
Surgical correction
In case of severe rhythm disturbances, when the hollow muscular organ is not able to cope with the load on its own, an electrical pacemaker or cardioverter is installed. They are activated during extrasystole, cardiac arrest, tachyarrhythmias and quickly normalize myocardial function.
The formation of an aneurysm is an indication for resection of the thinned area. The operation requires wide access and lengthy manipulations. Usually not performed in older people.
At-risk groups
The risk of cardiosclerosis is highest in patients with pathologies in the development of the heart and cardiovascular diseases, as well as in people with various types of allergies.
Pregnant women can be identified as a separate group. Pregnancy causes hormonal, autonomic, metabolic and hemodynamic changes in the body of women and can act as a proarrhythmogenic factor. Complex heart rhythm disturbances are diagnosed both in pregnant women with cardiovascular pathology and in patients without changes in metabolism and the condition of internal organs.
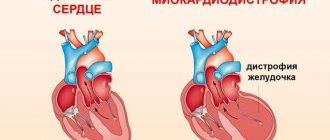
Cardiosclerosis in children is possible against the background of myocardial pathologies, for example, inflammatory and dystrophic processes, in particular diseases of the heart muscle caused by metabolic disorders in heart cells. These biochemical disorders significantly weaken the contractile, conductive, excitatory and automatic functions of the myocardium.
Diagnostics
The diagnosis of “atherosclerotic cardiosclerosis” is based on the results of laboratory and instrumental studies. The patient receives an appointment for tests and diagnostic procedures upon presentation of symptomatic complaints. Characteristic changes in the biochemical blood test indicate myocardial damage.
An increase in enzyme concentration is determined:
- aspartate aminotransferase (ALT);
- creatine phosphokinase (CPK);
- lactate dehydrogenase (LLH).
The lipidogram (the patient's lipid profile, which determines the quality of fat metabolism) shows a significant excess of the norm for total cholesterol, triglycerides, low and very low density lipoproteins. A general clinical blood test determines the hanging platelet count, the discrepancy between thrombocrit and platelet indices from normal values.
A number of pathological changes are recorded during a coagulogram (blood clotting test). Primary examination of the heart - ECG (electrocardiogram) reveals areas of the myocardium that have lost the ability to conduct impulses.
Depending on the nature and intensity of the violations, the following may be prescribed:
- transthoracic or transesophageal echocardiography - ultrasound of the heart with an external probe or a tubular probe through the esophagus;
- echocardiography with Doppler – examination of the aorta and coronary arteries;
- stress echocardiography – ultrasound of the heart in a calm state and after a dynamic load (physical exercise or administration of medications);
- coronography - x-ray of the coronary arteries of the heart with the introduction of a radiopaque substance.
If possible, magnetic resonance imaging or computed tomography of the cardiovascular system is performed.
Cardiosclerosis medications
The European Society of Cardiology recommends the following medications for the treatment of cardiosclerosis, eliminating the symptoms of the disease, as well as its root cause:
- Antihypertensive drugs. To maintain vascular tone and normalize blood pressure, ACE inhibitors (Captopril, Enalapril, Ramipril) are prescribed; calcium antagonists (Amlodipine, Semlopin, Phenigidine), beta blockers (Atenolol, Bisoprolol, Metoprolol), antiplatelet drugs (Aspirin), lipid-lowering drugs (Simvastatin, Atorvastatin, Allesta).
- Cardioprotectors (antianginal agents). Their task is to maintain the functional activity of the heart and counteract the influence of negative exo- and endogenous factors on it. These include organic nitrates (Nitroglycerin, Isosorbide Mono- and Dinitrate); sydnonimines (Mosikor, Sidocard); metabolic agents (Trimetazidine).
- To normalize heart rate and conduction: amiodarone (Amiodarone), dronedarone (Multak).
- To normalize metabolic processes - potassium and magnesium preparations: Panangin, Asparkam, Magnerot.
- Antibiotics and corticosteroids: for myocarditis and other inflammatory processes.
List of used literature
- Stryuk R.I., Shoikiemova D.U., Borisov I.V.; State Budgetary Educational Institution of Higher Professional Education "Moscow State Medical and Dental University named after. A.I. Evdokimov" Ministry of Health of the Russian Federation, Moscow, Russia / Pregnancy as a risk factor for heart rhythm disturbances
- POKROVSKAYA E.M., 2, Ph.D., N.A. VOLOV 2, Ph.D., I.S. VASILYEVA 2, GORDEEV I.G. 1, Doctor of Medical Sciences, Professor, PAVLIKOVA E.P., 2, Doctor of Medical Sciences, Professor 1 State Budgetary Educational Institution of Higher Professional Education “Russian National Research Medical University named after. N.I. Pirogov" of the Ministry of Health of Russia, Department of Hospital Therapy No. 1, Faculty of Medicine 2, State Budgetary Institution "City Clinical Hospital No. 15 named after. O.M. Filatova "DZ Moscow / NEW OPPORTUNITIES FOR TREATING PATIENTS WITH HEART FAILURE DUE TO POST-INFARCTION CARDIOSCLEROSIS
- Berezin A. E., Doctor of Medical Sciences, Professor of the Department of Internal Medicine No. 2 of the 1st Medical Faculty of Zaporozhye State Medical University / Combined potassium and magnesium preparations in the treatment of patients with high cardiovascular risk.
Frequently asked questions about cardiosclerosis
Which doctor treats cardiosclerosis?
If you suspect cardiosclerosis, you should contact a cardiologist.
What signs should you see a doctor for?
High blood pressure; arrhythmia; increased fatigue and swelling of the limbs.
Can cardiosclerosis develop in children?
Cardiosclerosis in children can develop against the background of inflammatory and dystrophic processes in the myocardium - in particular, diseases of the heart muscle caused by metabolic disorders in heart cells.
Complications
Atherosclerotic cardiosclerosis leads to disruption of the rhythm of heart contractions. Due to the fact that the conducted impulse “stumbles” over a healed area of the myocardium, the heart rate is lost. Types of failures:
- bradycardia – slowing of the rhythm. HR (heart rate) less than 60 beats/min.;
- tachycardia – heart rate more than 140 beats/min. without physical activity;
- extrasystole - uneven contraction of the heart (the most characteristic pathology for cardiosclerosis);
- atrial fibrillation is a chaotic contraction (in the atria the rhythm slows down, while the ventricles contract up to 140-150 times/min.).
Reference! The normal heart rate at rest for an adult ranges from 60 to 90 beats/min.
Unstable myocardial function leads to the development of:
- CHF (chronic heart failure);
- acute necrosis of a portion of the myocardium (infarction);
- congestion in the lungs and pulmonary edema;
- cardiomyopathy;
- sudden cardiac arrest (coronary death).
The main clinical syndrome of pathological changes in cardiosclerosis is angina pectoris (an imbalance in the myocardial oxygen demand and the supply of blood to the heart muscle).