- home
- general surgery
- Adrenal tumor
- Pheochromocytoma - hormonally active adrenal tumor
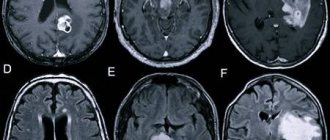
Pheochromocytoma accounts for about 5-7% of adrenal tumors. At the present stage of development of diagnostic methods, at least 50% of pheochromocytomas are initially detected as incidentalomas (accidentally detected), and only about half of these observations are accompanied by arterial hypertension. Despite certain advances in the interpretation of the radiological semiotics of pheochromocytoma, laboratory tests are fundamental in confirming the diagnosis.
Malignant pheochromocytomas (pheochromoblastomas) are often found. This group of pheochromocytomas also includes catecholamine-producing tumors with distant metastases. They are usually fused with surrounding organs. The tumor on the section is variegated due to the alternation of dark red areas and grayish fields of necrosis; the capsule is sharply worn out in places or even absent.
1.General information
In order not to overload the text with complex terminology from the very beginning, let’s try to figure it out in order. The title ends in "-oma", so it's definitely about a tumor.
Chromaffin cells (literally “related to chromium”) are a type of endocrine cells. Consequently, they are capable and obligated to produce hormones at the command of the nervous system, i.e. biochemical regulators of physiological and mental processes in the body.
The synonymous names for these cells are pheochromocytes; from here the “origin” of the tumor to which this article is devoted becomes clear. By the way, the prefix “feo-” indicates a dark color. Dissected chromocytes are stained with chromic acid salts and are visualized under a microscope as yellow-brown.
These cells produce catecholamines (“fear and battle hormones”), i.e. adrenaline, norepinephrine and dopamine. The history of scientific research into tumors developing from such tissue dates back to the 80s of the nineteenth century. Today, medicine knows a lot about pheochromocytoma, but not everything: a number of key points need further study.
It is known, in particular, that pheochromocytes are found in a variety of structures and systems of the body, but their greatest concentration is in the adrenal medulla.
Accordingly, pheochromocytoma in the vast majority of cases (approx. 90%) is found there. It is also known that this tumor is quite rare: statistical estimates vary slightly around the frequency of 1:200,000 (it should be noted that some sources consider this estimate to be underestimated), and the frequency of new confirmed cases of the disease is approximately 1 case per one and a half to two million people in the world. year. It has finally been established that pheochromocytoma is a classic hormone-producing tumor, i.e. its growth and activity cause increased levels of associated hormones.
Considering which hormones are secreted in chromaffin cells, it is not difficult to understand the patterns of the clinical picture of the disease.
A must read! Help with treatment and hospitalization!
Classification
The formation of the adrenal glands is distinguished, i.e. pheochromocytoma itself. In addition to the adrenal glands, a small number of chromaffin cells in the form of small clusters can be found in the heart, head, neck, bladder, and along the spine. Tumors in these cells are called paragangliomas. They have a similar effect on the body as pheochromocytomas, as the same hormones are released.
Classification of pheochromocytoma according to ICD-10
The disease is placed in section D35.0 - “Benign neoplasm of other and unspecified endocrine glands.”
2. Reasons
The etiopathogenetic mechanism of the triggering and development of pheochromocytoma is one of those moments that modern science cannot yet explain reliably and unambiguously. Diseases of this kind are usually called sporadic: in their rare occurrences, it is impossible to trace any logic and system, a statistically stable and repeated influence of any factors. Attempts to prove the hereditary nature have not yet been crowned with convincing success, although it has long been known that pheochromocytoma is one of a number of purely genetic syndromes (Sipple, Hippel-Lindau, etc.) - but precisely as one of many manifestations of a more general anomaly, and not as an axial, syndrome-forming one phenomenon. In general, one or another connection with heredity is found in no more than every tenth case.
Visit our Oncology page
Surgery for pheochromocytoma - possible options
Currently, surgeons use three options for operations for pheochromocytoma. Treatment of patients can be carried out through the open route, laparoscopic access (with the introduction of instruments through the abdominal cavity and manipulation under the control of a video camera) and retroperitoneoscopic (lumbar) access, in which instruments and an endoscope with a video camera are inserted into the retroperitoneal tissue surrounding the kidney and adrenal gland.
Traditional (“open”) surgery to remove pheochromocytoma
used by the vast majority of surgeons. During this operation, surgical actions are performed through a skin incision up to 20-30 cm long, with the intersection of the muscles of the anterior abdominal wall, chest and the diaphragm separating them. Only the separation of tissues on the way of the surgeon to the adrenal gland with this type of operation can take 30-40 minutes! The removal of the adrenal gland itself can take place quite quickly - in 5-10 minutes, after which the surgeon “starts the return journey”, suturing the cut muscles and tissues. This takes at least another half hour. As a result, the operation turns out to be long (about 2-2.5 hours), traumatic, forming a long postoperative suture on the skin and leading to persistent and prolonged pain, a difficult recovery process that requires a long stay of the patient in the hospital. Of course, large adrenal tumors that grow into neighboring organs even today sometimes require open surgery, but the progressive development of surgical technology has long led to the emergence of much less traumatic methods for removing pheochromocytoma - such as the laparoscopic method.
|
|
During laparoscopic surgery to remove pheochromocytoma
the patient is positioned on the operating table on his side, a high cushion is placed under the lower back, which, as it were, “breaks” the patient in the lumbar spine. In this position, the most convenient location of the internal organs is achieved for removing pheochromocytoma, and the intestinal loops are shifted down the abdominal cavity and do not interfere with the surgical process. Through small (about 1 cm) incisions in the skin of the anterior abdominal wall, instruments and an endoscope with a video camera are inserted into the abdominal cavity. After dissecting the peritoneum of the posterior surface of the abdominal cavity, the surgeon penetrates with instruments into the retroperitoneal space, where he finds the kidney and adrenal gland, after which he isolates the adrenal gland with pheochromocytoma and removes it. Pheochromocytoma is usually clearly visible, which makes the surgeon's job easier. After complete isolation of the tumor and clipping of its vessels, the pheochromocytoma is removed along with the adrenal gland. The peritoneum is sutured, then the instruments are removed from the abdominal cavity and postoperative wounds on the anterior abdominal wall are sutured. Compared to traditional open surgery, laparoscopic removal of pheochromocytoma is significantly less traumatic, has a shorter duration and is accompanied by the formation of smaller sutures. However, this operation also has disadvantages - it is difficult to perform for patients who have already had operations on the abdominal organs in the past, leading to the development of adhesions. Inserting instruments into the abdominal cavity during adhesions is dangerous due to the possibility of damage to large vessels or intestinal loops. It is also significantly complicated to perform laparoscopic surgery on the adrenal gland in obese patients who have a significant thickness of fatty tissue on the anterior surface of the abdominal cavity and large “reserves” of fat inside the abdominal cavity in the greater omentum. In obese patients, the length of laparoscopic instruments is sometimes simply not enough to “reach” the tumor. An important disadvantage of laparoscopic surgery is the need to introduce carbon dioxide into the abdominal cavity in order to create a working space for the movement of instruments and viewing of internal organs. The introduction of carbon dioxide into the abdominal cavity increases the pressure in it, as a result of which the diaphragm is pushed upward and compresses the lungs located above it, reducing their vital capacity. Impaired ventilation in elderly patients with severe concomitant diseases can lead to serious complications both during surgery and in the postoperative period. That is why the laparoscopic method of treatment, although it is certainly progressive, cannot be considered an ideal method for treating pheochromocytoma.
|
|
In 1994, in Essen (Germany), Professor Martin Waltz developed a technique for retroperitoneoscopic surgery on the adrenal gland
using a lumbar approach.
During this operation, the patient is positioned on the operating table on his stomach. Three incisions are made on the back, each about 1-1.5 cm long (with the traditional technique, otherwise called CORA
, from conventional retroperitoneoscopic adrenalectomy) or one incision 2.5-3 cm long (when removing pheochromocytoma with one access, the so-called
SARA
– single accessretroperitoneoscopicadrenalectomy). With the lumbar approach, the surgeon inserts instruments into the retroperitoneal lumbar fat, which contains the kidney and adrenal gland with pheochromocytoma. Unlike the laparoscopic approach, in which the surgeon needs to go a long way with instruments in order to get to the pheochromocytoma, with the lumbar approach the surgeon immediately “gets” to the tumor. Typically, tumor vessels are intersected using the Ligasure automatic electrocoagulator, which allows not only to reliably seal the internal lumen of the vessels, but also to dissect them after coagulation. The tumor is placed in a durable plastic container, in which it is crushed and brought out through the same incisions into which the instruments were inserted. After surgery on the lower back, the patient is left with three small stitches that are barely noticeable to the naked eye.
|
|
|
The lumbar approach to the adrenal gland has several important advantages that make it currently considered the best available approach to the adrenal gland for the removal of pheochromocytoma
.
Firstly, it provides faster and significantly less traumatic tumor removal
– in some cases, an experienced surgeon is able to perform an operation to remove pheochromocytoma in 30-40 minutes.
The speed of the operation in this case is very important - with a quick and accurate operation, much less manipulation is performed on the tumor, the surgeon presses less on its tissue with instruments, which leads to a decrease in the amount of adrenaline and norepinephrine entering the blood from the tumor. Rapid surgery using the lumbar approach is rarely accompanied by a dangerous increase in blood pressure levels, requiring emergency measures. It is important to consider that during lumbar surgery, the surgeon inserts instruments into the area where the adrenal vein is located, through which catecholamines enter the blood from pheochromocytoma. One of the first stages of the operation when using the lumbar approach is the intersection of the adrenal vein using the Ligasure device, after which nothing else enters the blood from the adrenal gland. Rapid division of the adrenal vein can dramatically reduce the level of complications during surgery
.
Secondly, the adrenal gland is located quite close to the surface of the skin, so the surgeon’s path to the adrenal gland is quite short. During the lumbar approach, the surgeon performs all manipulations not in the abdominal cavity, where the intestines and the peritoneum, which is easily traumatized and reacts very violently to touch, are located, but in the retroperitoneal space, where there is nothing except the kidney and adrenal gland. Therefore, the morbidity of the lumbar approach is very low
.
Thirdly, performing surgery outside the abdominal cavity makes it possible to remove pheochromocytoma using a lumbar approach even in patients who have previously undergone abdominal surgery, in obese patients, and in patients with severe spinal deformity
. This significantly expands the capabilities of surgeons.
Fourthly, surgery through the lumbar approach leads to the formation of barely noticeable sutures
small in size on the lower back, where they do not attract the attention of surrounding people.
The cosmetic result of such an operation is significantly superior to the result of open and laparoscopic surgery to remove the adrenal gland. If the lumbar operation was performed through one access (using SARA technology), then the cosmetic result of the operation is simply amazing
.
Fifthly, the low trauma and speed of surgery using the lumbar approach allows patients to recover quickly
after removal of pheochromocytoma. In the evening, patients can eat and drink and move around the ward. Discharge is made in 2-3 days.
Unfortunately, the mastery of lumbar access to the adrenal gland by surgeons is very slow. This approach requires the surgeon to have significant experience in operations to remove pheochromocytoma, so it is used only in specialized endocrine surgery centers.
3. Symptoms and diagnosis
Pheochromocytoma can be either malignant (in which case it is called pheochromoblastoma) or benign. Malignant ones are several times less common (and, as a rule, are localized outside the adrenal glands), but there is also no consensus in this regard. The fact is that pheochromocytoma more often meets some criteria for malignancy, but almost never meets others. Thus, more than 60% of such tumors grow due to atypical cells and become overgrown with their own vascular network of blood supply, but no more than 5% of pheochromocytomas metastasize and grow into adjacent structures.
Returning to the main clinical picture, it should be noted that most often the hormonal activity of pheochromocytoma manifests itself in crisis attacks: very high blood pressure (up to 300 mm Hg or more) is accompanied by a feeling of fear, tachycardia, pallor, nausea and/or vomiting, frequent and profuse urination, increased body temperature, increased heart rate, hyperhidrosis (forced sweating) and severe headache. The combination of the last three symptoms forms the so-called. Carney's triad and is observed in almost all patients with crisis-type pheochromocytoma. With a smoother type of course, blood pressure is increased almost constantly; with mixed forms, persistent hypertension alternates with even more dangerous crises; the most aggressive form of pheochromocytoma symptoms can result in life-threatening catecholamine shock.
Equally serious are other possible complications associated with hypersecretion of catecholamines and severe persistent arterial hypertension: various types of heart failure, stroke (acute cerebrovascular accidents, strokes), pathology of the gastrointestinal tract, kidneys, blood vessels, etc. The most dramatic outcome is sudden death from vascular collapse; This was precisely the first described clinical case associated with a bilateral adrenal tumor.
Diagnosis is extremely difficult, firstly, by the rarity of the pathology (in a doctor’s practice, pheochromocytoma may occur only once in a lifetime or not at all), and secondly, by the absence of pathognomonic or at least highly specific symptoms. Often, identifying the true cause of hypertension takes a lot of time and requires consistent exclusion of a number of symptomatically similar diseases. It is not for nothing that this tumor is called the “great imitator” - from one to two thirds of correct diagnoses are postmortem.
Adequate intravital diagnosis is based on anamnestic and clinical data, monitoring of blood pressure dynamics, laboratory tests of hormone levels in the blood, as well as imaging methods (ultrasound and tomography), which make it possible to clarify the size and localization of pheochromocytoma.
About our clinic Chistye Prudy metro station Medintercom page!
Diagnosis of pheochromocytoma.
Fractionated determination of metanephrines (that is, separate determination of metanephrine and normetanephrine, if indicated - methoxytyramine) in urine or plasma has the greatest diagnostic sensitivity in relation to the initial (i.e., truly tumor) amount of catecholamines. This test is recommended as a first-line diagnostic test. The sensitivity of the method for determining methylated catecholamine derivatives in urine is 99%, the specificity is 91. Plasma methylated catecholamines have a sensitivity of almost 99%, and a specificity of 85% - 89%.
Reference values for plasma and urinary fractionated metanephrines should primarily ensure optimal diagnostic sensitivity. The specificity of this test is assessed secondarily. This is due to the potential consequences of a missed diagnosis.
A decrease in specificity significantly increases the number of false-positive results; therefore, serious treatment decisions should be based on the degree to which the upper limit of reference values is exceeded. A slight excess of the upper limit of both plasma and urinary fractionated metanephrines is associated with a slight likelihood of pheochromocytoma, while a fourfold excess is associated with an almost 100% likelihood of this type of tumor.
If the results of hormonal studies are questionable, scintigraphy with MIBG-I123, determination of chromogranin A and/or a test with clonidine are used to increase the specificity of the test and verify the diagnosis of pheochromocytoma. With adrenal tumors with low native density of the tissue component (less than 10 H units), the likelihood of pheochromocytoma is extremely low, which can be used as a differential method in the “gray” zone of the level of fractionated metanephrines.
It should be noted that the study of fractionated metanephrines for the diagnosis of pheochromocytoma is a primary task that precedes the assessment of the malignant potential of the tumor.
4.Treatment
The method of choice is adrenalectomy - unilateral or total surgical removal of the adrenal glands (in the latter case, lifelong hormone replacement therapy will be required). Organ-preserving intervention is also practiced, but the risk of relapse is unreasonably high. Minimally invasive (endoscopic, without open cavity intervention) removal methods require further technical development. If there are contraindications, radiation therapy may be prescribed.
Conservative treatment, the essence of which is to inhibit the secretion of catecholamines by the tumor, is much less effective.
The prognosis depends on a number of clinical, morphological and individual factors. Thus, with timely surgical intervention for benign pheochromocytoma, the five-year survival rate (the main indicator for oncology) approaches 100% with a low percentage of relapses, but with a malignant course it does not reach even half (the remaining cases of pheochromoblastoma are characterized by sluggish progression and approximately 20-year survival).
Pheochromocytoma - treatment and preparation for it
The main treatment for pheochromocytoma is surgery. Removal of the tumor can significantly improve blood pressure in the vast majority of patients and reduce the likelihood of developing severe complications (stroke, myocardial infarction, myocardial hypertrophy). At the same time, performing surgery on an unprepared patient with high blood pressure (constantly high blood pressure or the presence of hypertensive crises) can lead to the development of severe and life-threatening complications during the operation: uncontrolled hemodynamic syndrome, cardiac arrhythmias, intraoperative vascular accidents (stroke). That is why special attention is currently paid to preparing patients for surgery for pheochromocytoma.
The objectives of preoperative preparation of patients with pheochromocytoma are to normalize blood pressure levels, eliminate dangerous fluctuations during the day, and reduce heart rate to 60 beats per minute.
The main drug used to prepare for surgery for pheochromocytoma is doxazosin (Cardura). The drug is prescribed at least 2 weeks before the planned operation. It is advisable to do the first prescription of the drug in a hospital or under the close supervision of a doctor, since very often the start of doxazosin is accompanied by a decrease in blood pressure, which frightens the patient (the so-called “first dose syndrome”). However, subsequent use of the drug is no longer accompanied by such unpleasant symptoms. Doxazosin causes blockade of alpha-adrenergic receptors and ensures their insensitivity to catecholamines released by the tumor. In some cases, beta-blockers (bisoprolol) are added to the preoperative preparation, which provide an additional decrease in heart rate. As additional preparations, antiplatelet agents (aspirin) are used to reduce the risk of thrombosis during surgery to remove pheochromocytoma.
With proper preparation, the operation usually takes place without any serious circulatory disorders. However, even in trained patients, a sharp increase in blood pressure can sometimes occur during manipulations on the tumor (moving it, isolating tumor vessels, pressing on the tumor). To eliminate dangerous surges in blood pressure in the operating room, fast and short-acting drugs (for example, sodium nitroprusside) are used, which allow you to quickly respond to increased pressure.
Registration for surgery to remove pheochromocytoma
To schedule an operation for pheochromocytoma, the patient must consult a specialist at the Northwestern Endocrinology Center. The center's endocrinologist surgeon will examine the available medical documentation and, if necessary, prescribe and evaluate the results of additional studies. If the diagnosis is confirmed and there are indications for surgery, hospitalization is carried out at the center for removal of pheochromocytoma using the most modern technologies.
Patients with pheochromocytoma are consulted:
| Sleptsov Ilya Valerievich, Endocrinologist surgeon, Doctor of Medical Sciences, Professor of the Department of Surgery with a course in surgical endocrinology, member of the European Association of Endocrine Surgeons | |
| Rebrova Dina Vladimirovna, Endocrinologist, Candidate of Medical Sciences. Assistant at the Department of Endocrinology named after Academician V.G. Baranov, North-Western State Medical University named after I.I. Mechnikov. Member of the European Society of Endocrinologists, International Endocrinological Society, St. Petersburg Association of Endocrinologists. | |
| Fedorov Elisey Alexandrovich, Surgeon-endocrinologist of the highest qualification category, Candidate of Medical Sciences, specialist at the North-West Center for Endocrinology. One of the most experienced surgeons in Russia performing operations on the adrenal glands. The operations are performed using a minimally traumatic retroperitoneoscopic approach through lumbar punctures, without incisions. | |
| Chinchuk Igor Konstantinovich , Endocrinologist surgeon, oncologist, candidate of medical sciences, member of the European Thyroid Association (ETA). Performs endoscopic operations on the adrenal glands. Retroperitoneoscopic approach. More than 350 surgical interventions per year, half of which are endoscopic. |
Consultations are carried out in outpatient branches of the center:
- Petrograd branch
(St. Petersburg, Kronverksky pr., 31, 200 meters from the Gorkovskaya metro station, telephone for appointment, from 7.30 to 20.00, daily);
— Primorsky branch
(St. Petersburg, Savushkina st., 124, building 1, 250 meters to the right from the Begovaya metro station, telephone for appointments from 7.00 to 21.00 on weekdays and from 7.00 to 19.00 on weekends).
For consultation, please bring all available examination results.
Operations at the Northwestern Endocrinology Center
The North-Western Endocrinology Center is the largest endocrine surgery clinic in Russia and Eastern Europe. The Endocrinology Center annually performs more than 2,100 operations on the thyroid gland, parathyroid glands, and adrenal glands. The absolute majority of operations on the adrenal gland are performed using a low-traumatic endoscopic lumbar approach. The center’s surgeons have significant experience in performing operations on the adrenal glands, and the center’s anesthesiologists and endocrinologists have extensive experience in preparing patients for surgery and subsequent management of patients after surgery to remove the adrenal gland.
To date, endocrinologist surgeons at the Northwestern Endocrinology Center have the greatest experience in performing operations on the adrenal glands using CORA and SARA technologies. Among the staff of the center are professors, doctors and candidates of medical sciences, doctors of the highest qualification category.
Currently, for residents of the Russian Federation, most operations on the adrenal glands at the North-Western Endocrinology Center are performed free of charge for patients
, within the framework of the federal quota system.
In the absence of quotas, patients can be hospitalized free of charge under the compulsory health insurance policy (CHI). Similar treatment is carried out for residents of any region of Russia
. For foreign citizens, as well as patients who, for one reason or another, are unable to be treated at the expense of the federal budget, surgery on the adrenal gland can be performed for a fee (the cost of a typical case with a 4-day hospitalization ranges from 70 to 80 thousand rubles).