Classification
Neutrophil leukocytes themselves come in two main types: segmented (mature) and band (young). Band neutrophils normally make up from 1 to 5% of the total number of leukocytes, segmented neutrophils - from 35 to 65%. Based on the ratio of young and mature cells, neutrophilia are distinguished with and without nuclear shift. A nuclear shift to the left implies an increase in the number of young forms of neutrophils and is divided into the following types:
- Hyporegenerative
. A slight increase in band neutrophil leukocytes. The cause is infectious, inflammatory diseases with a mild course. - Regenerative
. It is characterized by the appearance of metamyelocytes in the blood (intermediate forms between myeloblastic cells and granulocytes). Occurs during infections with moderate severity (typhoid fever, pneumonia). - Hyperregenerative
. Severe hyperactivation of the bone marrow granulocyte lineage with impaired granulocyte maturation. In the blood, the number of band neutrophils, metamyelocytes, promyelocytes is sharply increased, and myeloblasts are sometimes present. Possible aneosinophilia (complete absence of eosinophils). This form of neutrophilia is observed at the very beginning of purulent-inflammatory processes (sepsis, abscesses, phlegmon). - Degenerative
. Along with the increased number of band leukocytes, a large number of destructively altered segmented neutrophils (toxic granularity, pyknosis of nuclei) appear in the blood. Indicates inhibition of the functional activity of the bone marrow. Characteristic of the height of severe infections.
With neutrophilia, which has a nuclear shift to the right, the hemogram shows the absence of young forms of granulocytes and the appearance of hypersegmented (containing more than 5 segments) neutrophils. Neutrophilia without nuclear shift is accompanied by an increase in only segmented neutrophils. In relation to other types of leukocytes, the following are distinguished:
- Relative neutrophilia
. An increase in the percentage of neutrophils (in adults more than 75%, in children under 5 years of age - more than 55%) in the leukocyte formula, the total number of leukocytes is normal. - Absolute neutrophilia
. An increase in the number of neutrophils while simultaneously increasing the level of leukocytes.
Causes of neutrophilia
Physiological reasons
There is a so-called physiological neutrophilia, or pseudoneutrophilosis. Its occurrence is not associated with increased neutrophil production, but with their redistribution, i.e. a change in the ratio of the parietal and circulating pools of neutrophils towards the latter. Pseudoneutrophilia is observed under stress, intense physical activity, exposure to heat or cold, and after eating. Also, neutrophils are often increased during pregnancy and in a newborn child.
Infections in children
Due to a physiological decrease in the level of neutrophils due to leukocyte crossover, a child of preschool age (up to 5-6 years) has an increased susceptibility to bacterial infections. In children, neutrophils increase mainly with scarlet fever and streptococcal sore throat. A dangerous infection such as diphtheria is quite common in the pediatric population. Parasitic infestations (ascariasis, enterobiasis, toxocariasis) are also common among preschoolers. In these diseases, in addition to neutrophilia, high eosinophilia is observed in the blood.
Infections in adults
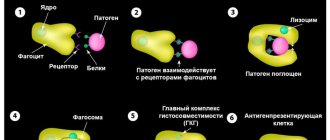
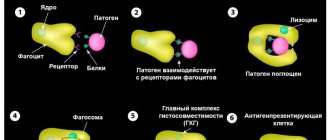
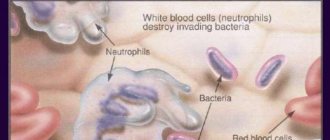
Most often, neutrophils are increased during bacterial infections. The main function of neutrophils is anti-infective protection of the macroorganism, namely, the destruction of bacteria. They also take part in the fight against viruses and parasites. Migrating through the vascular wall, neutrophils are directed to the site of localization of the pathogenic microorganism. By releasing cytokines and inflammatory mediators, neutrophils activate other components of the immune system (complement, T-B lymphocytes).
Neutrophil leukocytes first phagocytize (absorb) the infectious agent, then secrete degradation enzymes (lysozyme, lactoferrin, phosphatases) and reactive oxygen species (superoxide anion, hydroxyl radical, hydrogen peroxide), which contributes to the death of microorganisms. Neutrophilia increases rapidly, reaches a maximum parallel to the height of the disease, and gradually decreases after antibacterial therapy.
The most common cause of neutrophilia in adults is acute localized bacterial (pneumonia, sinusitis, pyelonephritis) or specific infections (typhoid fever). Moderate neutrophilia is typical for them. Less commonly, the cause is severe generalized infections (bacterial endocarditis, sepsis, meningococcal meningitis), characterized by high neutrophilia with a hyperregenerative or degenerative shift.
Acute surgical pathologies
Quite often, neutrophils are increased in acute abdominal pathology (cholecystitis, pancreatitis, perforation of a stomach or duodenal ulcer), purulent processes (phlegmon, abscess). Neurophilia in a child often occurs with appendicitis. An increase in the number of neutrophil leukocytes in these diseases acts as a reaction to the inflammatory process. A correlating relationship between the severity of inflammation and the degree of increase in neutrophils has been precisely established. Usually there is high neutrophilia with a degenerative shift of the leukocyte formula to the left, which quickly regresses after emergency surgery. However, neutrophils may remain within normal limits.
Tissue damage or breakdown
Such conditions include infarctions of various organs (myocardium, lungs, intestines), abdominal operations, gangrene, pancreatic necrosis. The cause of neutrophilia is stimulation by decay products of granulocytopoiesis in the bone marrow. An additional role is played by reactive neutrophilia, which occurs due to the release of large amounts of stress hormones (catecholamines, glucocorticosteroids) into the blood.
Also, the occurrence of neutrophilia in these conditions is facilitated by the addition of a secondary infection (for example, pneumonia due to pulmonary infarction). The degree of neutrophilia correlates with the volume of damaged, necrotic tissue, often reaches very high values (especially in a child), can persist for a long time, and decreases with recovery.
Rheumatological diseases
Neutrophilia can be observed in some chronic inflammatory pathologies of a rheumatic nature. There is an assumption that mediators, cytokines, and autoantibodies that are formed during rheumatic inflammation stimulate the bone marrow production of neutrophilic granulocytes. Typically, the appearance of neutrophilia along with other laboratory markers, such as an increased erythrocyte sedimentation rate and C-reactive protein, indicates an exacerbation of the disease.
After anti-inflammatory treatment, the concentration of neutrophils gradually returns to normal. In adults, especially high neutrophilia is characteristic of acute gouty attack, necrotizing vasculitis (polyarteritis nodosa, granulomatosis with polyangiitis). In a child, neutrophils are enlarged most often due to dermatomyositis.
- Joint diseases
: rheumatoid arthritis, ankylosing spondylitis (ankylosing spondylitis). - Diffuse connective tissue diseases (collagenoses)
: systemic lupus erythematosus, systemic scleroderma, Sjogren's disease. - Inflammatory bowel diseases
: Crohn's disease, ulcerative colitis. - Systemic vasculitis:
Takayasu's nonspecific aortoarteritis, Horton's giant cell arteritis.
Oncological diseases
Neutrophilia can sometimes indicate a malignant tumor. Its occurrence is promoted by two mechanisms - the breakdown of tumor tissue and the ability of some tumor cells to secrete granulocyte colony-stimulating growth factors (paraneoplastic syndrome). Neutrophilia most often occurs in patients with breast, lung, colon, and ovarian cancer. Neutrophilia increases slowly as the tumor grows, reaches moderate numbers, gradually regresses after chemotherapy, or quickly returns to normal after surgical removal of the neoplasia.
Hematological diseases
High neutrophilia is observed in oncohematological diseases. It can reach very high numbers (up to 100 thousand) in myeloproliferative diseases (acute, chronic myeloid leukemia). In lymphoproliferative pathologies (non-Hodgkin's lymphomas, lymphosarcoma), neutrophilia is slightly less pronounced and is almost always accompanied by absolute lymphocytosis. In a child, the most common cause is lymphogranulomatosis (Hodgkin's lymphoma).
In addition to neutrophilia itself, in patients with acute leukemia, a basophilic-eosinophilic association, a large number of blast cells and the absence of intermediate forms (leukemic failure) are found in the blood. The mechanism of neutrophilic leukocytosis lies in the malignant transformation of a hematopoietic stem cell. Granulocyte counts return to normal only after several courses of chemotherapy or bone marrow transplant.
Rare causes
- Endocrine disorders
: Cushing's disease or syndrome, thyrotoxic crisis. - Blood diseases
: hemolytic anemia, polycythemia vera, Addison-Birmer pernicious anemia. - Endogenous intoxication
: chronic renal failure, liver failure, diabetic ketoacidosis. - The phenomenon of bone marrow hyperactivation
: after agranulocytosis, treatment of megaloblastic anemia. - Use of medications
: adrenaline, cardiac glycosides, glucocorticosteroids, lithium. - Intoxication with mercury, lead
. - Exposure to ionizing radiation
.
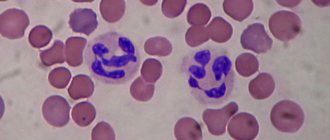
What are neutrophils
Blood Basics neutrophils are one of the types of leukocytes, white blood cells, thanks to which the body fights all kinds of infections. Moreover, this type of blood cells is the most numerous.
Up to 70% of the Blood Basics of all leukocytes in the human body are neutrophils.
Doctors call them immediate response cells. Having discovered a virus or bacteria, neutrophils rush to attack with lightning speed. Even if it means leaving the bloodstream and going into the tissues of the body.
The more clearly the immune system perceives a threat, the more neutrophils are produced in the bone marrow and the higher their level in the blood.
Diagnostics
Detection of neutrophilia requires differential diagnosis. To do this, you need to consult a general practitioner. In order to obtain primary information, anamnesis is collected - how long ago the symptoms appeared, whether there was recent contact with infectious patients, whether there was an increase in body temperature, pain, skin rashes.
If there is a suspicion of acute surgical abdominal pathology, the abdomen must be palpated for tension in the muscles of the anterior abdominal wall and the presence of a positive Shchetkin-Blumberg sign. However, it must be taken into account that these signs are difficult to identify in a child under 9 years of age. To confirm the diagnosis, additional examination is prescribed, including:
- Blood tests
. The total number and percentage of all types of leukocytes are calculated. The concentration of red blood cells, platelets, and inflammatory markers (ESR, CRP) is measured. The morphology of granulocytes (toxic granularity, karyopyknosis) is studied. In a septic condition, the level of presepsin and procalcitonin is determined. The presence of autoantibodies (anti-DNA, topoisomerase, antineutrophil antibodies) is checked. - Identification of the pathogen
. To identify the pathogenic microorganism, bacteriological culture, microscopy of sputum, urine, smear from the throat and tonsils are performed. To diagnose helminthiases, a stool test is performed for worm eggs, a blood test for specific immunoglobulins, and a scraping is taken from the child’s perianal folds. - Ultrasound
. A sign of pyelonephritis on an ultrasound of the abdominal cavity is expansion, thickening of the renal collecting system, pancreatitis - enlargement, diffuse changes in the pancreatic parenchyma, cholecystitis - thickening of the walls of the gallbladder, often the presence of stones. - X-ray
. On chest x-rays with pneumonia, foci of infiltration and darkening are visible. When the ulcer is perforated, the images reveal the presence of free gas in the abdominal cavity (“sickle symptom”). In case of inflammatory diseases of the joints, x-rays show a narrowing of the joint space and marginal osteoporosis. - ECG.
Electrocardiography during myocardial infarction reveals ST segment elevation, left bundle branch block, ventricular tachycardia, and other heart rhythm disturbances. With pulmonary embolism leading to pulmonary infarction, signs of overload of the right parts of the heart are detected - a deep Q wave in III, an S wave in lead I, a high pointed P wave (P-pulmonale) in leads II, III, aVF. - Histological studies
. A definitive diagnosis of cancer can only be made on the basis of a biopsy. The main feature of solid tumors is a large number of atypical cells. In case of leukemia, in the bone marrow biopsy, hyperplasia of the granulocytic lineage and the predominance of blast cells are noted; in the tissues of the lymph node in case of lymphomas, diffuse proliferation of cells with blast morphology is noted.
Secondary neutropenia
Secondary neutropenia most often develops due to:
- Taking certain medications (antibiotics, antihistamines, antipyretics, barbiturates, analgesics);
- Development of infections;
- Immune reactions;
- Bone marrow infiltration.
Secondary neutropenia provokes pathologies:
- Liver, spleen, kidneys;
- Pancreas, thyroid gland;
- Aplastic anemia;
- Megaloblastic anemia;
- Myelodysplastic disorders;
- Myelofibrosis, leukemia;
- Sepsis, HIV, Felty's syndrome;
- Rh-conflicting neutropenia;
- Lymphoproliferative diseases, etc.
In the case of secondary neutropenia, it is not the blood “test” that needs to be treated, but the patient with specific symptomatic manifestations.
Primary and secondary neutropenia should be distinguished, since in the first case, a decrease in the level of neutrophils is the only manifestation, while secondary ones develop on the basis of infections, systemic autoimmune pathologies and onco-neoplasia.
Correction
Conservative therapy
There are no direct ways to normalize the number of neutrophil granulocytes. To combat neutrophilia, it is necessary to treat the underlying disease against which it developed. Short-term neutrophilia after eating, stress or physical work does not require any intervention, as it is not a sign of disease or pathological condition. Neutrophilia resulting from surgery also does not need to be treated. In the case of persistent neutrophilia, you should consult a doctor to find out the cause and prescribe differentiated treatment:
- Antimicrobial (antiparasitic) therapy
. For bacterial infections, antibiotics (amoxicillin, cefixime) are used. For generalized infections (sepsis, bacterial endocarditis), it is necessary to use a combination of 2 antibacterial drugs. In case of helminthic infestation in a child, anthelmintic drugs (mebendazole) are prescribed. - Hemorheological therapy
. For heart attacks of any location caused by thrombosis or thromboembolism, antiplatelet drugs (acetylsalicylic acid), anticoagulant drugs (low molecular weight, unfractionated heparin), and sometimes thrombolytic drugs (alteplase) are used. - Antisecretory and antienzyme therapy
. In order to reduce the secretion of hydrochloric acid in peptic ulcers, proton pump inhibitors (omeprazole, pantoprazole), H2-blockers (famotidine, ranitidine) are used. To suppress the destructive action of proteolytic enzymes of the pancreas in acute pancreatitis and pancreatic necrosis, enzyme inhibitors (aprotinin) are effective. - Anti-inflammatory treatment
. To achieve remission of rheumatological diseases, medications are prescribed that stop the inflammatory process. These include glucocorticosteroids (prednisolone), 5-aminosalicylic acid derivatives (sulfasalazine), immunosuppressants (cyclophosphamide, methotrexate). - Chemotherapy.
For the treatment of malignant tumors, chemotherapeutic drugs (cytostatics, antimetabolites, hormone antagonists) are used in combination with radiotherapy. For oncohematological diseases, a combination of several antitumor agents is necessary.
Surgery
Many diseases accompanied by neutrophilia (mainly acute abdominal pathologies) require emergency surgical intervention - laparoscopic appendectomy, laparotomy and suturing of the ulcerative defect, cholecystectomy, opening and drainage of the abscess, etc. For myeloproliferative pathologies, in case of ineffectiveness of conservative therapy, they resort to stem cell transplantation cells.
Treatment
Intermittent neutropenia usually occurs without symptoms or severe infectious complications, and therefore does not require therapeutic treatment. Especially if the patient carefully observes the rules of personal hygiene, eats foods that have been heat-treated (raw fish dishes, meat with blood are not allowed in case of neutropenia), uses gloves when cleaning, and protects the skin from prolonged exposure to the sun.
With secondary neutropenia, treatment is aimed primarily at eliminating the underlying disease, which led to a pathological decrease in granulocytes.
At the Spizhenko Clinic, treatment of neutropenia is carried out taking into account the cause and clinical symptoms and may include:
- Antibacterial therapy.
- Antifungal therapy.
- Immunotherapy.
- Use of glucocorticoids.
Including treatment of associated conditions (ulcers, stomatitis, gingivitis) by rinsing the mouth with saline solution, using antiseptics (chlorhexidine), nystatin, clotrimazole, fluconazole (for candidiasis).
In case of acute lesions of the mucous membranes, an additional diet (with a predominance of liquid food in the diet) and local anesthesia are prescribed. If the decrease in neutrophils occurred as a result of taking medications, the way out of the situation is to stop using them and switch to alternative treatment.
Medicines
that lead to neutropenia:
- Anticonvulsants (Diazepam, Phenytoin, Sodium Valproate).
- Antidepressants (Clozapine, Haloperidol).
- Antibiotics (Doxycycline, Lincomycin, Cephalosporin, Penicillin, Vancomycin).
- Antiviral (Acyclovir, Zidovudine).
- Anthelmintics (Levomizole, Mebenzadol).
- Antituberculosis (Streptomycin, Rifampicin, Isoniazid, Ethambutol).
- Antifungals (Griseofulvin, Mycozolon, Amorolfine).
Including analgesics (Ibuprofen, Indomethacin, Amidopyrine, Acetylsalicylic acid, Phenylbutazone).
Treatment of febrile neutropenia
Febrile neutropenia requires immediate medical intervention (within 1 hour!).
For neutropenic fever the following is prescribed:
- Antimicrobial therapy;
- Emergency diagnostics (culture of blood, urine, secretions from the mouth, catheterization sites, vagina/urethra, ultrasound of internal organs, radiography).
The basis of modern antibacterial treatment for FN (febrile neutropenia) is beta-lactam antibiotics.
At the Spizhenko Clinic you can undergo a comprehensive study of neutropenia, determine the exact cause and receive the most correct treatment (if necessary).
Neutropenia is not a “sentence”, but also not a reason to leave this situation without competent medical attention.
Forecast
It is impossible to predict prognosis based on neutrophilia alone. It all depends on the disease that served as the background for the occurrence of neutrophilia. For example, a transient increase in the number of neutrophils after stress, food intake, or in a child on the first day of life is absolutely benign and transient. Conversely, severe purulent-septic pathologies and oncological diseases have a fairly high incidence of deaths. Therefore, any excess of the reference values of neutrophils (especially high and persistent ones) requires contacting a doctor.
For what reasons do neutrophils decrease?
Most often, neutrophils decrease due to the occurrence of an inflammatory disease, viral infection and radiation exposure. Quite often the following factors provoke the appearance of neutropenia:
- poor environmental conditions;
- use of certain medications (“Sulfanilamide”, “Analgin” and “Levomycetin”);
- inflammatory process in the body.
A reduced percentage of neutrophils is not an independent disease. This is only the result of the development of another disease, which can be identified after a thorough medical examination. If laboratory test results are unsatisfactory, you should visit a hematologist. After a thorough examination, the specialist prescribes complex therapy.