Endocrinologist
Fedorov
Elena Anatolyevna
10 years of experience
Endocrinologist
Make an appointment
People diagnosed with diabetes should be aware of hypoglycemic syndrome. This is a condition that occurs when blood sugar levels drop to critically low levels. Hypoglycemia and manifestations of symptoms are variable. The phenomenon can be dangerous to health and life. A drop in sugar (glucose) levels occurs when you skip a meal or after intense physical activity. The deterioration in health occurs suddenly. It is necessary to carefully monitor your condition and know measures to prevent an attack.
All the necessary information about the disease
A person’s condition directly depends on the level of glucose in the blood. If the values drop to 1.9-2.2 mmol/l in women and to 2.5-2.8 mmol/l in men, a hypoglycemic state occurs. In people with diabetes, such jumps in indicators are not uncommon. This poses a particular danger to the brain. He is the most sensitive in this aspect. Glucose levels are regulated in the body by a number of metabolic processes. In a healthy person, hypoglycemia does not occur because the liver contains a sufficient amount of glycogen.
Causes of hypoglycemia
A decrease in blood sugar levels is not a disease, but a condition that occurs due to a number of disorders of carbohydrate metabolism in the body.
Glucose, as a source of energy, determines the functioning of internal organs and the condition of a person as a whole. The brain is especially sensitive to a drop in sugar concentration. It works more intensively than all other organs, consumes an increased amount of “fuel”, is not able to store it and therefore is completely dependent on the continuous supply of glucose through the bloodstream.
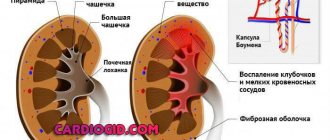
In the body of a healthy person, excess glucose from carbohydrates received from food is stored in the liver in the form of glycogen - a molecule consisting of many interconnected glucose molecules, which, if necessary, is broken down and absorbed into the blood. This ensures the smooth functioning of organs. Thus, any liver pathology can lead to hypoglycemia.
In addition, hormones significantly influence glucose metabolism:
- pancreas: insulin (responsible for the accumulation of glucose in the form of glycogen and reducing its level in the blood) and glucagon (stimulates the breakdown of glycogen, which causes an increase in sugar levels);
- adrenal glands: adrenaline, cortisol, growth hormone (increases sugar);
- thyroid gland: thyroxine and triiodothyronine (increase sugar).
Hypoglycemia is most often observed in diabetes mellitus.
On the one hand, the patient takes glucose-lowering medications. On the other hand, glucose from the liver enters the blood slowly. This leads to the fact that at some point the sugar concentration may drop to critically low values. This condition also occurs as a result of diseases of the gastrointestinal tract with impaired absorption of glucose, renal failure (increased excretion of sugar in the urine), cancer of the pancreas and some congenital pathologies.
Hypoglycemia resulting from disease is called pathological. In contrast, physiological hypoglycemia develops in healthy people during fasting, dehydration, emotional stress or excessive physical activity, taking certain drugs and alcohol.
In women, hypoglycemia is sometimes observed during pregnancy due to the fact that part of the mother's glucose is spent on fetal development. Hypoglycemia in children develops in the first hours or days after birth and can be temporary or permanent. Risk factors include prematurity, maternal diabetes, birth asphyxia, and congenital pancreatic anomalies.
How do symptoms manifest themselves?
Hypoglycemia symptoms begin to appear due to increased activity of the autonomic nervous system. And first of all, a person notices sweating. Further in different combinations there may be:
- nausea and vomiting;
- feeling of hunger;
- headache and weakness;
- drowsiness;
- frequent urination;
- blurred vision;
- lack of coordination;
- fear, panic, hand tremors;
- pallor of the skin.
Are you experiencing symptoms of hypoglycemia?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Symptoms of hypoglycemia
Clinical manifestations of hypoglycemia
consist of a number of symptoms that are combined into the categories of general disorders, autonomic or neurogenic, neurological or neuroglycopenic, metabolic.
General symptoms and neurogenic signs appear when glucose levels drop to 3.3 - 3 mmol/l. Patients, as a rule, complain of increased heart rate, increased nervousness and anxiety, increased sweating, hunger, and a burning sensation in the epigastric region. Upon examination, you can reveal pallor of the skin, trembling of the hands, and impaired sensitivity.
Neuroglycopenic symptoms, indicating an energy deficiency in the brain, are patient complaints of weakness, increased fatigue, decreased concentration, headaches and dizziness. Patients and their immediate environment may also notice disturbances in the organs of vision and speech, changes in behavior, and seizures.
With a sharp decrease in blood glucose levels, a severe complication develops - hypoglycemic coma, characterized by loss of consciousness and lack of sensitivity to various stimuli.
Signs of hypoglycemia
do not always appear gradually. Typically, signs of the initial stage of hypoglycemia are severe hunger, trembling hands, sweating, tachycardia, irritability, feelings of aggression and fear. If these signs are promptly eliminated by eating foods containing easily digestible carbohydrates, the process can be reversed without a trace. However, in case of untimely relief of this condition, it is aggravated by the addition of neurological signs such as double vision, loss of orientation, and hallucinations. The patients' condition is similar to the picture of deep alcoholic intoxication or a hysteroid reaction. In the absence of correction of the hypoglycemic state at this stage, the condition of patients is usually aggravated by increased agitation, the appearance of vomiting, the appearance of clonic and tonic convulsions, clouding and loss of consciousness, followed by the onset of coma.
Patients with a long history of decompensated diabetes mellitus may experience the above-described symptoms of hypoglycemia with a blood glucose level of 5-7 mmol/l. This is the so-called false hypoglycemia. That is why, to confirm the diagnosis, one cannot rely only on clinical signs; laboratory data are needed that can confirm the falsehood or truth of hypoglycemia.
Reasons for the development of hypoglycemic syndrome
For the disease hypoglycemia, the causes lie in skipping meals (with an interval of more than 6 hours). The following items can also cause deterioration in health:
- insufficient amount of carbohydrates in the diet;
- excessive physical activity and stress;
- administration of an increased dose of insulin;
- use of certain types of medications;
- severe emotional stress;
- dehydration of the body.
Prognosis and prevention
Despite the significant number of complications, in most cases hypoglycemia is mild or moderate in severity. In diabetes, it accounts for only 3-4% of the mortality rate. The main cause of death is cardiovascular accidents (heart attack, stroke). To prevent hypoglycemia in diabetes, the patient must strictly adhere to the dosage, technique and frequency of insulin administration, not skip meals, and avoid drinking alcohol.
When carrying out insulin therapy, you need to regularly monitor your blood glucose level with a glucometer, and have quickly digestible carbohydrates with you to independently relieve hypoglycemia. It is also necessary to competently select the dose of glucose-lowering drugs, taking into account the patient’s liver and kidney function and possible drug interactions. For patients with metabolic disorders (glycogenosis, galactosemia), frequent split meals with large amounts of carbohydrates are recommended.
What are the varieties?
It is worth noting that hypoglycemia itself is not a disease in the classical sense. This is a condition that occurs due to certain factors and accompanies different types of diseases. Most often we are talking about diabetes mellitus. In medical practice, there are several stages of this condition:
- easy (a person can help himself independently);
- medium (requires help from other people);
- severe (the most severe stage, when a person falls into a hypoglycemic coma).
Classification
Detection of hypoglycemia in a blood test is not always true. False, or pseudohypoglycemia, can occur with leukocytosis, erythrocytosis. Separately, transient hypoglycemia is distinguished in newborns born to mothers with diabetes. According to the severity, hypoglycemia is divided into mild, moderate, severe, and according to its course - acute, subacute, chronic. According to etiopathogenesis, the following types of hypoglycemia are distinguished:
- Lean (spontaneous)
. Develops with excessive secretion of insulin, insulin-like factor and diseases accompanied by a deficiency of contrainsular hormones. - Reactive (postprandial)
. Occurs 2-4 hours after eating. The cause is the early stage of diabetes, hereditary metabolic disorders, post-resection syndromes, autoimmune insulin syndrome. - Induced
. Develops in diabetes, caused by drinking alcohol and medications.
Possible complications
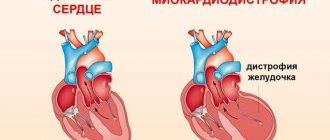
Signs of hypoglycemia should not be ignored. The deterioration of the condition develops quickly. The worst complication is coma, when a person does not receive timely help and the blood sugar level drops below minimum values. Among the complications, it is necessary to highlight the negative impact on small peripheral vessels that are subject to destruction. The legs and eyes are at risk. The legs and eyes are the first to be affected. Over time, blindness and angiopathy (pathology of the retinal vessels of the eye) may develop. If the sugar level drops below 2 mmol/l, the brain is at risk.
Pathogenesis
Glucose is the main energy substrate for the central nervous system. Therefore, the central nervous system is very sensitive to hypoglycemia. First, as a compensatory reaction, counter-insular hormones are released into the blood, including catecholamines (adrenaline, norepinephrine), which cause vegetative symptoms. If glucose continues to be low, neuroglycopenia occurs.
Brain cells (mainly the cerebral cortex, diencephalic structures) begin to experience energy starvation, all metabolic processes, redox reactions, etc. are inhibited in them. Persistent hypoglycemia affects the medulla oblongata and the upper parts of the spinal cord, which leads to suppression of reflexes, convulsive readiness of the brain, impaired consciousness, and coma. Pathomorphological changes include edema, necrosis of certain areas of the brain.
Information about diagnosis and treatment
It is quite simple to notice and determine a change in condition, which is due to characteristic symptoms. For this reason, diagnosis of hypoglycemia is based primarily on an initial analysis of the patient’s condition. After the examination, a number of tests and studies are prescribed to clarify the etiology and diagnosis:
- blood and urine tests;
- study of blood glucose concentration;
- biochemical blood test with determination of albumin and protein;
- urine glucose test;
- insulin level studies;
- assessment of the function of the thyroid gland, pituitary gland and pituitary-adrenal system;
- Ultrasound of the abdominal organs.
Treatment of hypoglycemia
Conservative therapy
To treat mild hypoglycemia, it is enough to take easily digestible carbohydrates - fruit juice, sweet tea, a few pieces of refined sugar. In case of moderate and severe severity, the patient must be hospitalized in the endocrinology department, and in case of depressed consciousness and coma - in the intensive care unit, where the following is carried out:
- Relieving hypoglycemia
. A glucose solution is administered intravenously; if the patient does not regain consciousness, drip administration continues. Intramuscular administration of glucagon is also effective (except for hypoglycemia caused by alcohol and sulfonylurea derivatives). Ascorbic acid is used to improve glucose utilization by neurons. To prevent cerebral edema in severe patients, magnesium sulfate, dexamethasone, and diuretics (mannitol or furosemide) are used. - Treatment of the underlying disease
. If the cause of hypoglycemia is a deficiency of contrainsular hormones, hormone replacement therapy (hydrocortisone, fludrocortisone, L-thyroxine) is performed. For autoimmune insulin syndrome, glucocorticosteroids, immunosuppressants, and plasmapheresis sessions are used. For the treatment of malignant insulinomas, if there are contraindications to surgery, the drug streptozocin is prescribed, which causes the death of beta cells of the pancreas. To improve the motor-evacuation function of the stomach in diabetes, prokinetics (itopride) are used.
Surgery
The most effective treatment for insulin and nesidioblastosis is surgery. In 90% of cases, the operation achieves a complete cure for the disease. The method of choice is tumor enucleation. Sometimes resection of the head, body or tail of the pancreas is performed. As a preoperative preparation, a powerful inhibitor of insulin secretion, diazoxide, is prescribed. Hyperglycemia is possible for 72 hours after surgery. To prevent it, short-acting insulin is administered. After removal of extrapancreatic tumors, glycemic levels return to normal very quickly.
Self-monitoring of general condition
Hypoglycemia is a condition that can be self-controlled when it is mild. Thus, people with type 1 diabetes monitor their blood sugar levels without the help of doctors and make the necessary adjustments. The diet for hypoglycemia consists of consuming foods with a low hypoglycemic index. It is recommended to avoid those foods that can cause a sharp jump in blood glucose levels. This list includes candies, cookies, cakes and other sweets with fast carbohydrates. They can be used in small quantities if the condition worsens.
Classification of hypoglycemia
It is customary to distinguish two forms of hypoglycemia
, differing from each other in the severity of the condition.
1. Mild hypoglycemia
- in this condition, the patient, regardless of the severity of clinical symptoms, can correct the hypoglycemic state independently by ingesting carbohydrate foods.
2. Severe hypoglycemia
accompanied by disturbances of consciousness, including its loss. In this case, the patient needs outside help.
Symptoms of hypoglycemia
Hypoglycemia may be characterized by the following symptoms:
- Weakness and fatigue;
- Anxiety;
- Nausea;
- Sweating;
- Trembling in the limbs;
- Rapid heartbeat;
- Paresthesia (the so-called numbness of the limbs, tingling, “goosebumps”);
- Visual disturbances (for example, the patient may have double vision);
- Decreased ability to concentrate, drowsiness;
- Headache;
- Impaired consciousness (the patient may even fall into a coma)
- In some cases, convulsions.
Possible complications of hypoglycemia
If, in the presence of the symptoms of hypoglycemia described above, the necessary assistance is not provided, the second stage of hypoglycemia develops. It is characterized by the appearance of auditory, olfactory and visual hallucinations, paresthesia - false sensations (crawling on the skin, phantom pain, etc.).
Then the patient loses vision, develops convulsions, loses consciousness and falls into a coma.
You can distinguish hypoglycemic coma from others by the following signs:
- drop in blood pressure, weak pulse;
- shallow breathing;
- skin pale, cold, moist and clammy;
- the tone of the eyeballs is reduced;
- the person does not smell of acetone (as in ketoacidotic coma in diabetics).
How to treat hypoglycemia
It is logical that if the sugar level is below normal, then you need to raise it. How to do it right? When stopping hypo, it is important to act QUICKLY and ACCURATELY. For adults, it is recommended to use the so-called “rule 15”
:
- for hypoglycemia, take 15 grams of fast carbohydrates
- wait 15 minutes and take a blood sugar test
- if glucose levels are still low, take another 15 grams of fast carbohydrates
- blood sugar measurement after 15 minutes
- repeat until sugar returns to normal
This rule is not suitable for small children and people with high sensitivity to carbohydrates. For such people, 5-10 grams of carbohydrates are enough to successfully stop hypoglycemia.