Home » Articles » Lactostasis: what to do if your breasts are inflamed
Young mothers often face problems. Most often they are related to their health. Even the natural process of breastfeeding can bring problems, one of them is lactostasis. The doctor makes this diagnosis to every third woman who chooses natural feeding. Let's figure out how to cope with this disease.
What is lactostasis
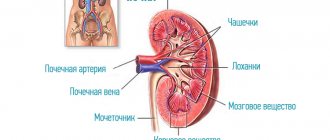
Lactostasis is a blockage of the milk ducts, which first causes heaviness in the breasts, and then severe pain and other symptoms. Anatomically, this process looks like this:
- The mammary gland consists of lobules;
- ducts pass between them - through them milk flows to the nipple;
- if the duct is blocked, the milk does not come out of the lobule and accumulates there;
- symptoms arise, becoming brighter as the lobule fills.
Causes of blocked ducts:
- Choosing a single feeding position. In this case, the baby does not empty all the lobules, but a plug forms in others.
- Choosing a single sleeping position. If a woman sleeps only on her side, then milk will accumulate in the lobes located under the arms.
- Insufficient fluid intake. If a woman is in a stuffy room or walking along the street in the heat, she needs to increase the volume of consumption of clean water, juices and compotes. Otherwise, the viscosity of the milk will increase, and it will be difficult for the baby to empty the lobes.
- Reduced activity on the part of the child during feeding due to the use of pacifiers and nipples.
- Incorrectly selected underwear. Young mothers often do not purchase new underwear for nursing and the postpartum period, but use bras with underwires or the wrong size. Breasts change after childbirth, so you need the right underwear that will not put pressure on the mammary gland. It should not have hard bones or hard cups.
- Disruption of the ducts as a result of edema due to injury to the mammary gland.
- Regular pumping after feeding. Because of this procedure, the milk increases and the baby cannot empty the breast completely. Remaining milk will cause blockage.
Decaying lactostasis
24/7 help and advice
The doctor will come to you within an hour after the call
Some pediatricians are of the opinion that feeding should be interval. In this case, the baby is put to the breast every 3 hours, and each of the breasts is emptied only once every 6 hours. If you follow the on-demand feeding method, the risk of lactostasis will be less. In this case, it may occur in the first weeks after birth, and then lactation improves and blockages do not occur.
If milk stagnation does occur, what should you do at home? Step-by-step instruction
Step 1.
First of all, don't panic. Stress reactions and tension impair milk flow. You need to relax as much as possible to stimulate the oxytocin reflex. Therefore, walking with a baby and a stroller is bad for you now, but bed rest is good.
Drinking a warm drink immediately before feeding or pumping is very helpful for relaxation. You can also apply a heating pad to the collar area.
Step 2.
The most effective measure is to put the baby to the sore breast more often. Often points 1+2 are enough to solve the problem, but if that doesn’t help, read on:
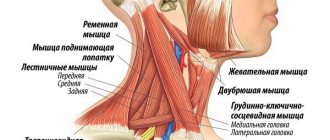
Massage during stagnation of milk should be done according to the movement of lymph: from the areola to the armpits and collarbones.
Step 3.
Perhaps in your situation you need to improve your application as much as possible, contact a consultant to correct it. If there is no possibility of an in-person consultation, find someone who can advise you using photos and videos. If it is impossible to get such help quickly, at least feed in different positions. For lactostasis and mastitis, it sometimes helps to turn the baby with his chin towards the seal. I also recommend reading my article “Proper breastfeeding” (link at the end of the text).
Step 4.
Apply cold to the sore area after feeding. For example, a towel soaked in ice water. You can throw ice in a deep bowl and cool the compress as it warms up from the skin. Cold should be applied regularly after each feeding from the sore breast for 7-15 minutes. It helps eliminate swelling in the breast tissue. Swelling often additionally blocks stagnant milk.
Step 5.
Breast massage during milk stagnation is also a very good decongestant measure! It should be done from the areola to the nearest large lymph nodes: the armpits and collarbones. Using light circular or stroking movements, and without pressing on the mammary gland with great force!
Step 6.
Stimulating the movement of lymph helps to effectively eliminate milk stagnation or quickly remove residual symptoms. For example, elements of lymphatic drainage massage: kneading the collar area and shoulders, warming rubbing under the collarbones and in the armpit.
During the consultation, I also give so-called “lymphatic exercises.” This set of exercises was started by Anna Osipyan, one of the first consultants with the international IBCLC certificate in Russia:
1. Hands folded at the chest in a “praying” or “namaste” position - a greeting from yoga. The palms press hard on each other so that tension is felt in the armpits. 2. Hands in a “lock” behind your back. Rock the “lock” up and down. 3. Using the thumb and index finger of either hand, we feel the pits between the ribs, where they are attached to the sternum. We massage the pits in a circular motion, moving down from the upper ribs to the lower ones. Then repeat with the other hand. 4. Clench your hands into fists and rub the ribs at the sternum up and down with your middle phalanges.
- The hands are folded at the chest in a “praying” position or “namaste” - a greeting from yoga. The palms press hard on each other so that tension is felt in the armpits.
- Rotate your shoulders.
- We stretch the lateral surfaces of the body: we stretch our right hand up, above our heads, and to the left, in turn, so that we feel the muscles stretching on the right side of the thigh. The same with the left hand.
- We place the ribs of the palms under the lower ribs and rub them.
- We place our palms under the lower ribs and, with an exhalation, lightly plunge them into the stomach. With each exhalation, we move deeper as far as possible, tilting the body forward.
- Throw your hand behind your head and pat your armpit.
- We place the ribs of the palms under the lower ribs and rub them.
- Throw your hand behind your head and pat your armpit.
5. Rotate your shoulders.
6. Stretch the lateral surfaces of the body: we stretch our right hand upward, above our head and to the left, in turn, so that we feel the muscles stretching on the right side of the thigh. The same with the left hand. 7. Place the ribs of the palms under the lower ribs and rub them. 8. Put your hand behind your head and pat your armpit. 9. This exercise should be done while sitting (on a chair or cross-legged on the floor). Place your palm under the ribs, with the back side facing the body. Fingers point vertically upward. We inhale, and as we exhale, we gently lower ourselves, plunging our fingertips under our ribs. New breath - we stop. New exhalation - down again.You can go lower and lower until you feel the first pain. When they occur, make a slight rocking vibration with your fingers. The main thing is not to overdo it and work in your comfort zone. You can avoid pain completely.
Having done the exercise closer to the center, we move our fingers further away from each other. We move them to the sides as many times as necessary to work the entire hypochondrium area.
9. We place our fingers under the lower ribs and, with an exhalation, lightly plunge them into the stomach.
With each exhalation we move deeper, tilting the body forward. It is better to do gymnastics while standing. At high temperatures it is better to refrain. Contraindicated for cancer!
Step 7
Practice shows that Traumeel-s ointment can help, especially in cases where redness and fever appear. However, there are no studies confirming the effectiveness of this drug. On the first day, it is enough to apply the ointment to the sore area 4 times, and then 2 times a day.
Symptoms of the disease
Signs of lactostasis can be divided into two groups: at an early stage and after inflammation has begun (in advanced form). Immediately after the blockage of the duct appears, the woman feels:
- chest pain;
- compaction in the area of one or more lobes;
- slight tissue swelling.
Departure is paid separately - from 550 rubles
Request a call
Call:
+7 (499) 455-08-05
Sometimes it happens like this: there is pain and swelling of the tissue, but there is no compaction. This happens with a slight lactostasis, which went away on its own. For example, milk stagnation occurred at night, and in the morning you fed the baby, and it resolved.
How to understand that inflammation has begun
More advanced lactostasis, which can only be treated with the help of a specialist, is often accompanied by a pronounced inflammatory process. Its symptoms:
- skin redness;
- increased body temperature;
- severe pain;
- bad feeling;
- heaviness in the chest;
- feeling of fullness of the gland.
If you have lactostasis, then the temperature will remain at 37-37.5 degrees. If it becomes higher, then this is a sign of the development of infectious mastitis. After the lobes and ducts are emptied, the temperature will drop within a few hours.
Preventive actions
Prevention of lactostasis involves the nursing mother following several recommendations. The baby should be fed regularly (but no more than once every two hours), and any remaining milk should be carefully expressed using a manual or automatic breast pump.
You should avoid wearing tight underwear. Limiting physical activity and stress during lactation significantly reduces the likelihood of lactostasis. An important role is played by the diet - it must include fresh vegetables and fruits.
If symptoms of lactostasis appear, you should not stop feeding your baby. If there is a prolonged delay in milk flow, you should consult a doctor. Self-administration of any medications is not recommended. It should be borne in mind that the affected mammary gland after recovery may produce less milk. Over time, secretory function will be restored in full.
Treatment options
There are several methods for treating lactostasis. It is best to use only those recommended by doctors or invite a specialist to your home to help you and establish breastfeeding. Most young mothers take the wrong actions during lactostasis, aggravating their condition.
Massage
One of the main methods that can influence lactostasis is massage. It is worth kneading the mammary gland or performing lymphatic drainage. In the latter case, you should entrust the actions to a doctor, since you will not achieve a positive effect on your own. Correctly influencing the breasts should be done according to the following rules:
- knead from the outer area to the nipple;
- make only smooth and careful movements;
- stroke and rub your breasts.
If you have pain in the chest, you need to massage it very carefully. Some women do it in the shower while expressing milk. If you choose this option, you must not overdo it - pumping should be done until relief, and not until the breast is completely emptied.
Departure is paid separately - from 550 rubles
Request a call
Call:
+7 (499) 455-08-05
To reduce tissue swelling, it is necessary to apply a cool compress to the chest after manipulation. Some people choose cabbage leaves or a wet towel for it. Thanks to this, the mother’s condition can be slightly alleviated, and the milk will flow easily during feeding.
Hot shower
Another way to get rid of swelling, congestion and pain is to treat it with a shower. The water should be lukewarm and under no circumstances hot, since the mammary glands cannot be overheated. An increase in temperature will only worsen the woman’s condition, as the milk will become more viscous and the swelling will intensify.
A warm shower along with massage movements with a washcloth or hands can cope with slight lactostasis. If the problem is serious, it is necessary to express the excess milk. You can do this right under the shower - the streams of water relax the ducts and gently massage the breasts.
Professional help
The best solution for young mothers is to call a professional at home. You should contact him at the first symptoms, then you will quickly get rid of stagnation and prevent the development of mastitis. You can’t do without the help of a specialist when:
- prolonged stagnation, with symptoms persisting for 48 hours or more;
- an increase in body temperature above 37.7 degrees;
- severe pain;
- intense redness of the skin in the area of congestion.
All these signs may indicate that a woman has developed mastitis. It will not be possible to cope with it using folk and improvised means.
A doctor who deals with lactation problems is able to choose the right method to eliminate stagnation. He can offer:
- medicinal method of treatment;
- teach how to express milk correctly;
- perform a massage correctly;
- choose a suitable compress.
He will also give the young mother a lecture on proper breastfeeding and suggest the appropriate position and regimen. Most breastfeeding doctors are good psychologists. They will calm the woman down and help her achieve a state of psychological comfort. It is worth remembering that stress leads to spasm of the ducts, which causes disruptions in lactation.
How to express milk during stagnation?
If, despite all the steps taken, the baby still cannot cope with the resorption of stagnation, you need to try to express the milk yourself. In rare cases, even a breast pump may work.
But it’s more effective with your hands. However, there is no need to press with all your might on the stagnation. This is very painful and traumatizes the breast tissue. The World Health Organization does not recommend using this method in its materials!
The technique of pressing your fingers on the areola works great. It's called the Marmet pumping technique:
Place your fingertips on the border of the areola and white skin, in line with the nipple. For example, first from above and below the nipple. We press towards the ribs, and then begin to move our fingers towards each other and a little forward. Fingers should not slip on the skin! They should stand in one area and move with the breast tissue. There is also no need to pull the nipple forward. (See video at the end of the article). To enhance the effect with less pressure on the areola, you need to rest the base of the hand on the chest, and not keep your hand suspended.
To make pumping more effective, you should think about relaxing and drink a cup of warm drink first, or get under a warming shower - it is better to direct it not on the chest, but on the neck and back. You can also steam your feet.
What not to do with lactostasis
Many mothers are interested in whether it is possible to feed a child with stagnant milk. The answer to this question is yes. He needs to be fed on demand, trying to choose different positions. It is recommended to place the child so that his chin faces the area of congestion.
But there are a number of actions that will lead to a worsening of your condition:
- the use of ointments belonging to the group of non-steroidal anti-inflammatory drugs;
- treating the skin with alcohol or camphor;
- taking painkillers;
- intensive gland massage;
- breast tightening bandages;
- use of local warming preparations;
- refusal of breastfeeding.
It is strictly forbidden to go to baths and saunas while breastfeeding. A stuffy room negatively affects the quality of milk, and with lactostasis, overheating can lead to the development of mastitis. The inflammatory process will develop quickly due to an increase in the thickness of the milk and heating of the tissues.
If milk stagnation occurs, you should not:
- You can’t stop feeding your baby (if you’re pumping, you can’t stop pumping). Milk must continue to be removed, otherwise the problem will be aggravated by inflammation or congestion in the adjacent lobes.
- You can't limit your drinking. A lack of fluid in the body makes it difficult for milk to flow out.
- You can't warm your chest. Heat helps pathological flora multiply. This can lead to mastitis more quickly.
- Do not apply alcohol compresses. Alcohol blocks oxytocin receptors and suppresses milk production. It can be very disruptive if you want to continue breastfeeding. In addition, the alcohol compress will warm the sore area.
- Do not put too much pressure on the milk lobes. As I wrote above, this injures the breast tissue and aggravates the swelling.
- You cannot ask your husband or other relatives to “dissolve” the stagnation. This often leads to even greater swelling and trauma to the areola, as well as mastitis. An adult will not be able to suck and move his tongue like a child, but he will be able to leave behind pathogenic flora!
Prevention
Any disease is easier to prevent than to treat. There are several ways to help reduce the risk of developing lactostasis to 5%.
- Prevent cracked nipples. To do this, you need to properly attach the baby and prepare the nipples for feeding. Cracks appear in almost all women who put children to their breasts for the first time. If you could not avoid them, then you need to start treatment in a timely manner.
- Wear comfortable underwear. Give preference to soft bras that do not compress your breasts. Be sure to choose them according to your parameters - models that are too spacious or narrow can injure the gland.
- Feed your baby on demand. Don't try to create a clear schedule, trust nature.
- Eat right and remember to drink enough fluids. This will help improve lactation and strengthen the body of a nursing mother.
- Try to avoid stress and rest more often. After giving birth, you need to restore your strength, try not to argue with your household and not panic over trifles.
It is important to establish proper lactation so that enough milk is produced so that the baby has enough of it, and there is no excess left in the breast. This is a very delicate process with which professionals will help you. Due to the heavy workload of maternity hospitals, young mothers are practically not taught how to breastfeed their children. This leads to the fact that they apply it incorrectly and make many other mistakes, leading to stagnation of milk and infectious mastitis.
Causes of pathology
The development of lactostasis occurs against the background of decreased patency of the excretory duct of the mammary gland due to excess milk production. The milky passages are subject to spasms, which cause their obstruction. The anatomical features of the structure of the mammary glands of patients have a significant impact on the likelihood of developing lactostasis:
- flat nipple;
- sagging breasts;
- narrowed milk ducts.
Often the pathology develops due to a sudden cessation of lactation or difficulty feeding. Cracks may form on the nipples. Similarly, the likelihood of developing lactostasis in a nursing girl is influenced by:
- improper attachment of the baby to the breast;
- insufficient sucking activity of the child;
- tight underwear;
- falling asleep on the stomach;
- hypothermia of the chest;
- stressful situations.
Some women experience blockage of the milk ducts due to excessive physical activity after the birth of a child.
Is there enough breast milk for adequate feeding? How to increase milk production?
Expectant mothers worry about whether they will have milk and whether there will be enough to feed the baby as many times as he asks.
In principle, it should not happen that milk does not appear at all - nature will not allow this. There may be little milk or it may disappear due to illness or nervousness, which is why peace of mind and the absence of stress are so important for a nursing woman.
There are several ways to increase lactation (breast milk production).
- Eating walnuts in small quantities, of course, causes milk to appear.
- Tea with milk, green tea and any liquid in general should be consumed by a nursing mother in larger volumes than before childbirth. Modern industry, using scientific developments and folk recipes, produces special teas to increase lactation. In about 30 minutes. Before feeding, you should drink a mug of such hot tea, since it is the hot liquid that will cause the flow of milk.
- Before feeding, you can take a shower: warm water on your breasts will promote milk flow.
- To increase lactation, it is useful to carry out night feedings.