Signs of a depressive phase
Bipolar disorder begins in most patients without noticeable bright manifestations.
In a typical case of MDP, there are subtle fluctuations in the background mood with cycles of several days or weeks. Researchers of the problem emphasize that the unfavorable course of bipolar disorder is the onset of the disorder from the first depressive episode. During the depressive phase, 89% of suicides or suicide attempts occur. Depression occurs when high productivity of mental processes is abruptly replaced by its decline. Specific manifestations of the phase:
- severely depressed mood;
- slowing down the thought process;
- slower speech motor activity;
- decreased or complete absence of appetite, perverted taste sensitivity;
- weight loss;
- prostration;
- in women - problems with menstruation;
- mothers have problems with maternal instinct;
- lack of sexual desires;
- melancholy, which is felt physically as heaviness in the chest area;
- attacks of tachycardia, constipation, mydriasis (dilated pupils of the eyes);
- self-flagellation, guilt;
- increased anxiety;
- cognitive impairment.
Depression sometimes takes on an endogenous form - due to the biological nature of the disorder, not only mental, but also somatic and endocrine disorders occur.
Sometimes an “atypical” course of depression develops—increased appetite, hypersomnia. There is also a hypochondriacal type of disorder - in this case, obsessive hypochondriacal beliefs with an affective overtone are noted. With the delusional type of progression, “Cotard's syndrome” is present - in addition to anxiety, delusional beliefs of a fantastic nature are observed. With agitation depression there is noticeable nervous overexcitation. With the asthenic variant, the patient experiences a loss of the ability to feel anything.
Patients experience unmotivated sadness and a feeling of hopelessness especially acutely - from several hours to several days without the ability to be distracted by anything else. The person withdraws into himself and stops contacting family members and friends. Interest in those activities and things that previously had interests is completely lost. Low ability to learn new things. Appetite may be uncontrollable or absent.
Fatigue and lack of energy are felt around the clock. Sleep is interrupted, and episodes of awakening occur frequently, especially in the early morning. After sleep, a person does not feel rested. Memory problems arise and concentration is poor. Thoughts about suicide appear - a person experiences a clear conviction that life has no meaning and will never bring pleasure. With parasuicidal behavior, a syndrome of “tunnel thinking” is observed.
The depressive phase is very dangerous due to the high level of suicidal tendencies, parasuicides, and auto-aggressive acts. It is recommended to hospitalize the person for subsequent treatment in a hospital setting. 24-hour monitoring of the patient’s condition and indicators is important.
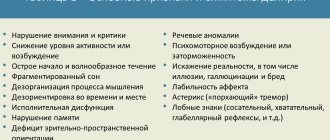
Clinical picture of bipolar disorder
The symptoms of bipolar disorder are determined by the manifestations of the main phases - mania (hypomania), depression. The number of episodes is unpredictable, as is their severity. The duration of an exacerbation can range from several days to 1-2 years. Intermissions (“bright” interval with the absence of symptoms) with controlled treatment persist for 3-10 years or more.
Symptoms and signs of the manic phase
Manic syndrome varies in severity, from hypomania to severe psychotic disorders. The classical phase should include a triad of such signs: ideational-mental and motor arousal, elevated mood (hyperthymia). A “full” episode occurs in 5 stages, accompanied by a worsening of symptoms followed by calm.
Hypomania is the mildest degree, not accompanied by delusional-hallucinatory phenomena. The patient is unusually cheerful, active, and energetic. Increased social activity, hypersexuality, and shortened sleep duration are possible. People take extravagant actions, spend money thoughtlessly or, on the contrary, become aggressive. Thinking is accelerated, speech is confused, and attention is easily distracted.
Approximately 86% of patients with bipolar disorder experienced a severe manic phase. Delusional ideas of grandeur, hallucinations, and an influx of thoughts (mentism) cause social maladjustment. Mood changes should be clear, observed for at least 4-7 days (depending on the phase criteria according to ICD-10).
Symptoms and signs of the depressive phase
Depressive episodes usually last at least three times longer than manic episodes. The classic syndrome includes the following symptoms that should be observed for at least 2 weeks:
- Symptoms are worse in the morning.
- Decreased/absent habitual responses to events or activities that would normally resonate within the person.
- Interests are reduced. The patient ceases to enjoy individually pleasant phenomena, things, food.
- Appetite, body weight, and libido decrease.
- Psychomotor retardation confirmed by others.
- Fast fatiguability.
- Lack of self-confidence, decreased self-esteem.
- Slowing of mental activity, ineffective work capacity.
- Unreasonable feelings of guilt, self-judgment, thoughts of death, or suicidal behavior.
- Insomnia or drowsiness.
Mixed episodes consist of symptoms from both phases and can appear at any stage of the disease. Rapid cyclicity (10-15% of patients) is indicated by the development of at least 4 cases of exacerbation per year, accompanied by intermissions.
Patients usually remain in the depression phase most of their lives. Thus, patients with type G BD are on average 32% of the time in a state of depression and 9% in a state of mania/hypomania. Patients with type BD GG spend 50% of their time in the depression phase and only 1% in a state of hypomania. Depression is usually the first symptom of BD, especially in women. The risk of suicide during this phase is greatest.
Sturov N.V., Romanova O.L. Bipolar disorders: clinical picture and principles of therapy // Difficult Patient. 2008. No. 4.
Diagnostics
Diagnosis is carried out by psychiatrists. This is an important step before treating the disorder, since the symptoms of many mental disorders are similar to each other. To exclude or confirm organic lesions, MRI of the head, radiography, and electroencephalography are prescribed. The diagnosis is made according to the criteria of the ICD disorder according to the categorical division of symptoms.
An episode of a mood disorder is considered to be a condition in which the mood disorder is expressed to a certain degree and for a certain time: depression - 2 weeks; mania – 1 week. According to researchers FK Goodwin, KR Jamison (in 1990), 65-70% of initially established psychiatric diagnoses are erroneous - other diseases are easily confused with bipolar disorder. The consequence is the prescription of incorrect drug treatment, aggravation of the course of MDP.
The diagnosis of manic stage is established if the person being examined has at least three of the following symptoms:
- delusions of grandeur;
- excessively low need for sleep;
- previously unusual incoherence of speech;
- uncontrolled flow of ideas;
- previously unusual distractibility;
- psychomotor stimulation;
- interest in activities with increased risk to life or health;
- problems in labor, educational, social functioning of the individual.
The psychiatrist determines the severity of the disorder: mild, moderate or severe with psychotic symptoms. According to research by authors RM Hirschfield et al., (2003), G. Perugi (2010), affective disorder is more often confused with depression (60%), anxiety disorder (26%), schizophrenia (18%), personality disorders (17%) , addiction to psychoactive substances (14%).
To establish the correct diagnosis, pay attention to the following points:
- with bipolar disorder, there is an unstable mental response to treatment with antidepressant drugs;
- in case of bipolar disorder, depression and anxiety are initially not combined with the use of psychoactive substances;
- psychotic symptoms develop at a previously normal level of social adaptation;
- family history is likely to include mood disorders or other mental pathologies.
The complexity of diagnosis is based on the fact that the symptom complex of bipolar disorder in its depressive phase is in many ways similar to clinical depression. Differences between bipolar depression and its other types: appetite disorder of the hyperphagia type, the presence of hypersomnia, mild psychotic manifestations. Bipolar disorder is also differentiated from classical depression by the fact that manifestations are noticeable in childhood and develop faster.
Treatment
Treatment for manic-depressive psychosis is gradual. First, the current exacerbation is stopped, normalizing the psychophysical state of the person. Next, maintenance and anti-relapse treatment regimens are individually prescribed.
A suicidal condition is an indication for emergency hospitalization. In some cases, electroconvulsive therapy (ECT) is justified to overcome drug resistance. ECT is relatively safe, as it is performed under anesthesia with the use of muscle relaxants, but there are a number of contraindications.
Medication
The choice of pharmaceuticals depends not only on the severity of symptoms. Relief from an acute condition is possible with the help of rationally prescribed drugs in adequate dosage. Often during treatment it is necessary to change medications, taking into account individual tolerance.
The following groups of pharmaceutical drugs can be used in the treatment of bipolar disorders:
- mood stabilizers - eliminate psychomotor agitation, normalize mood - Valproate, lithium preparations, benzodiazepines;
- neuroleptics - auxiliary drugs in the presence of severe psychotic symptoms, eliminate delusions and hallucinations;
- antidepressants from the group of selective serotonin reuptake inhibitors;
- combinations of psychotropic drugs in individually tolerable doses;
- symptomatic treatment of concomitant disorders.
Quickly bringing aggression and psychomotor agitation under control prevents the exacerbation episode from prolonging. The preventive effect of the drugs develops gradually, so maintenance therapy is prescribed for a long period. Timely relief of depression is necessary to prevent suicidal behavior.
Psychotherapy and rehabilitation
Pharmacotherapy is carried out against the background of psychosocial support. Rehabilitation measures significantly help in managing people with a depressive phase, reducing the frequency of relapse. Particular attention is paid to the following areas:
- increasing awareness of the patient and his caregivers about the nature of the disease, features of the course, methods of therapy and prognosis;
- formation of motivation to improve the quality of life;
- explaining the need to comply with the prescribed regimen;
- training to recognize early signs of developing relapse;
- methods of dealing with stress, exacerbation triggers, risk factors;
- psychotherapy – individual (cognitive-behavioral, rational), family, group (interpersonal).
A scheduled consultation with your doctor is a key point in treatment, so you need to openly discuss all issues with a specialist. The psychiatrist must regularly monitor not only the effectiveness of the measures taken, but also monitor changes in the person’s status. If necessary, the therapeutic course is modified.
Causes of the disease
Accurate scientific data on the causes of TIR have not yet been established. But there are confirmed factors that increase the risk of developing the disease:
- genetic predisposition;
- autointoxication with psychoactive substances;
- disturbed endocrine water balance, water-electrolyte metabolism;
- organic disorders.
The following hormones are involved in the development of pathology: norepinephrine, serotonin, dopamine, acetylcholine, GABA. With bipolar disorder, there is an increased tone of the sympathetic nervous system, hyperfunction of the thyroid gland and pituitary gland.
At risk are persons with the following characteristics:
- melancholic temperament;
- excessive conscientiousness;
- traits of a psychasthenic personality type;
- increased anxiety and suspiciousness;
- instability of the emotional sphere.
The disorder occurs either for no apparent reason or after provoking factors (stress, past infections, psychological trauma, against the background of other mental pathologies).
The main role among the reasons is given to the genetic factor. It has been established that if a close relative has mental pathologies, the risk of developing bipolar disorder is 14-15%. M.R. Post and SR Weiss in 1989 described the causes of bipolar disorder, which were hidden in the effects of various stimulants and surfactants.
Psychotherapy for manic-depressive psychosis
Treatment of a patient with this type of disorder is best carried out with the participation of several specialists at once - a psychologist, a psychotherapist with the constant participation of a psychiatrist. Therefore, to get a good result and achieve sustainable remission, you should contact a medical institution with a full team of doctors.
An important component of the complex treatment of manic-depressive psychosis is psychotherapy. She helps:
- learn to manage symptoms of affective attacks;
- improve socialization;
- optimize professional functioning;
- independently cope with stressful situations;
- improve intrafamily relationships.
Experienced specialists at our clinic approach the choice of the method of providing assistance individually. Each patient has his own treatment regimen.
To choose a treatment method, many factors are taken into account: age, severity of the condition, personality characteristics of the patient. Cognitive-behavioral, interpersonal, family therapy, and social support help well with this disorder. For many patients, social rhythm therapy becomes a salvation.
The cognitive-behavioral method helps a person cope with the manifestations of the disease and avoid factors that can provoke another exacerbation. At the same time, the patient learns to solve his problems. This practice makes it possible to identify hypomania and depression at an early stage, normalize the patient’s sleep and activity level. Thanks to the work of a specialist, a person’s vulnerability to external influences becomes less, which reduces the likelihood of relapse.
Family therapy for manic-depressive psychosis shows high effectiveness. An experienced psychotherapist helps not only the patient, but also his loved ones:
- it is easier to experience affective episodes;
- accept the inevitability of severe mood swings in the future;
- understand the need to use mood stabilizers to prevent another attack and relieve its manifestations;
- separate the personality traits of the patient and the symptoms characteristic of the disorder;
- detect and cope with psycho-emotional life situations that can cause aggravation;
- restore functional relationships after the relief of an affective episode.
Properly selected psychotherapeutic treatment allows a person to successfully neutralize the effects of stress factors, which most often are a trigger for the development of one of the phases of the disease.
A patient diagnosed with manic-depressive psychosis exhibits high sensitivity to even minimal changes in the alternation of sleep and wakefulness. Often they develop another episode due to a disruption in their routine, for example, due to jet lag. Therefore, psychotherapists pay great attention to teaching patients to regulate rhythms, especially before life events that can greatly disrupt them. This skill allows you to optimize the prognosis for this disease and reduce the number of exacerbations.
As practice shows, overcoming an illness largely depends on the willingness of the person and those around him to discuss the problem out loud. A comparative description of one’s condition and the characteristics of the manifestation of manic-depressive psychosis in other people has a positive effect on the patient’s health. Therefore, when he is ill, it is useful for him to attend group classes, where he can share his experiences, listen to people with similar complaints, and receive support. Such meetings represent a minimized model of society and help the patient to successfully adapt to ordinary life in the future.
Differences between males and females
If you believe the statistics, men get sick less often than women. Ratio: 3:2. The female part of the patients is characterized by a rapidly cyclical nature of the disorder. Women have low sensitivity to therapeutic methods. They have a higher risk of suicidal behavior and a higher rate of hospitalization. The symptoms of bipolar disorder in men are practically no different from the manifestations of the disorder in women.
Minor differences - in the male part of the patients the phases of mania and hypomania predominate, and in the female part - depressive states. Symptoms of depression in women are much more pronounced.
How is bipolar disorder treated?
Treatment for each patient is selected individually, depending on the characteristics of his personality, the course of the disease and the condition of the body. The most common methods:
- medications (antidepressants, mood stabilizers, antipsychotics, neurometabolic drugs);
- physiotherapy (electro-sleep, TCM, electroanalgesia);
- Biofeedback therapy (biofeedback);
- psychotherapy;
- massage and exercise therapy;
- diet therapy.
TIR in children
Bipolar affective disorder is most often diagnosed in people between 15 and 55 years of age. Symptoms are most pronounced at the age of 16-20 years.
Very rarely, bipolar disorder is observed in childhood. The difficulty of diagnosis at this age stage is that symptoms of a mood disorder are often confused with ADHD. Treatment for ADHD involves taking stimulants. And if the child really has bipolar disorder, then stimulants increase symptoms in the manic phase.
The course of the disease in children differs from the pathology of adults. Children during manic periods show more irritability than adult patients. The symptoms of mania are usually more severe, and hallucinations are sometimes present.
Childhood patients, experiencing a depressive phase, suffer from physical symptoms and pain. A noticeable difference in children's bipolar disorder is hidden in the frequency of alternating cycles. A child’s cycles change very quickly, sometimes even within a day.
Diagnosis is also difficult for adolescent children. The reason is that the symptoms are difficult to differentiate from depression or mood swings that are natural for this age. In case of childhood mental disorders, in addition to the classical treatment regimen, it is important to consult with parents to increase pedagogical awareness.
Types and classification of manic-depressive psychosis
Modern clinical classification divides manic-depressive psychosis into two large types, according to the predominance of one of the phases. The first option is a unipolar option, when only periodic mania or periodic depression is observed, the second is bipolar, with an alternation of high or low mood, with a predominance of one of the phases or a clear change in them. Bipolar disorder is divided into types:
- correctly intermittent, when mania successively replaces depression and there is a light interval between episodes;
- irregularly alternating, the phases alternate chaotically, with no definite order, there are time intervals between them without a change in mood;
- double, in which two opposite phases are observed in a row, and then interphase occurs;
- circular (continuum), this type is the most severe, with it there is a constant change of affective manifestations without gaps between them.
To accurately determine the type of disease, consultation with an experienced specialist is required. In our clinic you can make an appointment with him by phone, or call a doctor at home.
The most common type of psychosis or periodic depression occurs. In the international classification, it is classified as recurrent depression, although some experts disagree with this. The number of phases during a person’s life varies. Some have only one episode, while others have more than a dozen. The duration of the acute affective state can be observed from one week to two years, with depression usually lasting somewhat longer than mania. The light period lasts from three to seven years. Cases are described in a number of patients of mixed episodes, when there is a simultaneous manifestation of both phases, or they quickly replace each other during the day.
Questions and answers
When is hospitalization required for a manic patient?
In case of severe mania, hospitalization will allow the patient to avoid actions aimed at himself and others. It will also help to identify the minimum maintenance doses of drugs to prevent another exacerbation. If a person, after stopping the attack, continues to follow the recommendations for taking medications, then the likelihood of developing the next phase will be minimal.
What is the best thing to do if a relative develops a manic stage and refuses treatment?
There are several options. One of them is calling a doctor at home and following his recommendations. The second is forced hospitalization if a person poses a threat to himself and others. Usually, after the symptoms subside, most patients agree to go to the doctor on their own, as their condition worsens, they feel weak and empty.