Causes of the syndrome
The disease develops due to a disruption in the normal functioning of the q11-13 region of the 15th pair of chromosomes. PWS can occur due to damage to only the paternal chromosome.
The reasons for the development of the disease include:
- Loss of section q11-13 of the father's gamete. Occurs in approximately 70% of people.
- Absence of a copy of the 15th chromosome of the father and disomy of the mother's chromosomes. Observed in 20% of cases.
- In 5% of patients, deactivation occurs in the fetus due to methylation of the paternal chromosome at the q11-13 site.
It is generally accepted that PWS is isolated and sporadic. But some scientists still classify the dangerous syndrome as an autosomal dominant disorder.
Due to the fact that in Prader-Willi syndrome the paternal chromosome is damaged and all its work is disrupted, increased deposition in the subcutaneous fat is observed. The exchange of sex hormones also becomes difficult, which means that the healthy functioning of the genital organs becomes impossible, and various anomalies appear in the structure of the organs of the reproductive system.
People with PWS are predisposed to the formation of malignant tumors due to genetically inherent weak DNA protection.
Aniridia
With aniridia, the normal structure of the eye is disrupted: the organ of vision lacks the iris. In addition, concomitant pathological changes often develop, such as macular hypoplasia and optic nerve hypoplasia, corneal changes, and cataracts. Visual acuity noticeably drops, attempts at correction do not bring significant results. Photophobia and horizontal nystagmus develop. In some cases, congenital glaucoma appears.
The cause of the disease is a dysfunction of the PAX6 gene from the short arm of chromosome 11. The protein it encodes leads to the launch of a number of processes that control the process of proper formation of the visual organs and a number of other structures. It is noteworthy that the gene is very conservative: the difference between the forms of PAX6 in humans and zebrafish is less than 5%, despite the divergence of evolutionary lines approximately 400 million years ago.
The disease belongs to the group of autosomal dominant pathologies. In the case of homozygosity for a mutant copy of the PAX6 gene, the negative effect on the body increases, which causes multiple disturbances in the functioning of the visual organs. In addition, the central nervous system is affected, which leads to death.
Treatment is aimed at relieving symptoms. To visually imitate the pupil, it is recommended to use specially colored lenses. It is possible to restore the pupil through reconstructive plastic surgery.
Symptoms of Prader-Willi syndrome
The presence of a disorder can be detected already in the early stages of pregnancy. The fetus is not only inactive, but also incorrectly positioned, and asphyxia or malnutrition is possible. Polyhydramnios sometimes occurs. Also, a pregnant woman's gonadotropin levels change. Babies are often born premature and tend to be breech. Based on these indicators, specialists must conduct additional diagnostics.
In infancy, with Prader-Willi syndrome, the child has weakened muscle tone, impaired coordination of movements, and hip dislocation is common. Sometimes the baby does not have a sucking and swallowing reflex, so feeding is only possible through a tube. In rare cases, breathing becomes impaired and artificial ventilation becomes necessary.
Children with the syndrome regularly experience drowsiness, apathy, and fatigue. They are often stubborn, hostile and aggressive.
Already in infancy, dysmorphia of the skull and acromicria of the arms and legs become noticeable, which manifests itself:
- Strabismus;
- Almond-shaped eyes;
- Large bridge of nose;
- Elongated skull shape;
- Small mouth or narrow upper lip;
- Violation of pigmentation of the iris of the eyes, skin and hair;
- Low-set ears.
As the disease progresses, a person experiences:
- Spinal diseases: scoliosis and osteochondrosis;
- Increased appetite, and, consequently, excess weight;
- Oral diseases: caries, gingivitis;
- Mental retardation;
- Ataxia;
- Muscle spasms;
- Late reproductive maturation.
changes in the limbs in PWS
Already in adolescence, children with Prader-Willi symptom are not similar to their peers. Patients are characterized by:
- Short stature and excess weight;
- Speech development delay;
- Excessive flexibility;
- Learning disability.
In children with PWS, the development coefficient does not exceed 80 units, while the norm is 85-115 units. However, they have a very developed imagination, the guys can write and read, but due to the small set of words they speak, their speech abilities still lag behind the norm. Mathematics and calligraphy are difficult.
The mental state of patients is usually unstable. Regular outbursts of aggression, anger and hysteria are replaced by friendliness. Such children are characterized by obsessive-compulsive neurosis, hallucinations, depression, and sometimes dermatillomania – tearing off the skin on the body.
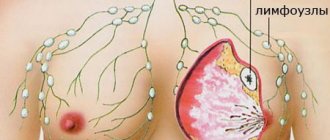
Patients suffer due to dysfunction of the hypothalamus. As a result, underdevelopment of the ovaries and testicles appears, and, consequently, the production of hormones is disrupted. It also leads to lack of pigmentation in the skin, eyes and hair. The child develops an endless feeling of hunger and becomes obese. Fat deposition usually occurs in the thighs and abdomen.
Endocrine disorders
There are several factors that support the concept of growth deficiency in individuals susceptible to the syndrome.
- Affected individuals are short and overly obese, meaning they have low free fat mass, low bone density, and low energy use.
- This disease is characterized by disturbances in the genitourinary system. In males, problems arise with undescended testicles (over time, the testicles may drop to normal levels), and in females, problems arise with the appearance of adrenarche. In both cases, it is possible to solve the problem surgically.
Diagnosis of PWS
Diagnosis of the disease in its initial stages allows you to prevent the development of some of its symptoms:
- Therapy started at an early stage develops correct eating behavior in the child;
- If specialists begin to adjust the ratio of growth hormones before the 18th month of life, the baby’s physique will develop correctly, just like a healthy person.
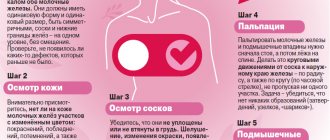
Typically, the diagnosis is made based on external and internal symptoms. In infants, the disease is suspected with a score of 5 on a special scale, in children over 3 years old - with 8 (4 of them should be major signs).
Large signs equal to one point:
- Periodic difficulties with feeding the newborn;
- Delay in cognitive development up to 5-6 years;
- Special facial features: almond-shaped eyes, small mouth, narrow upper lip;
- Muscle hypotonia detected at the age of 1 to 3 years;
- Changes in the structure of the organs of the reproductive system;
- Development of obesity.
Minor signs (0.5 points):
- Insufficient fetal activity;
- Refractive errors;
- Damage to the skin;
- Reduced pigmentation of the iris, hair and skin;
- Thick saliva;
- Short stature;
- Disproportional limbs;
- Sleep problems;
- Mental abnormalities in behavior;
- Articulation impairment.
In addition to the above criteria, to accurately determine the diagnosis, karyotyping should be performed and the presence of various modifications at the level of chromosome 15 should be determined. DNA markers and the prometaphase analysis method are also used.
Often the pathology becomes noticeable already during an ultrasound examination of pregnancy. The specialist notices an increase in amniotic fluid, fetal hypoxia or its non-standard location. At the slightest suspicion of a disorder, the expectant mother will have to undergo perinatal diagnostics, including genetic testing and a blood test for gonadotropin levels. Also, to determine the syndrome, it is necessary to use special molecular genetic markers.
Children with PWS move little, often steal food, hide food, and, even despite a recent snack, are constantly hungry. In this case, there is a threat of apnea - stopping breathing during sleep, which is dangerous and possibly fatal.
How is Robert and Christina’s relationship with your other children?
Marina A.: The eldest son, Leon, was waiting for his brother. Kissed my belly when I was pregnant. He has treated him with such tenderness since birth. During feedings, when I poured milk into Robert through the tube, Leon sat next to him and held his brother’s hand, and approached this process very responsibly. But their age difference is less than two years. And now he is so happy about his brother’s success. For example, when Rob is trying to stand, Leon comes running and tells me: “Can you imagine, Robert was standing! I counted to three, and he stood there!” I am very glad that Robert has an older brother, he is a huge support for everyone.
Leon with his younger brother Robert
Marina V.: Christina is my fifth child, and other children see that she is different and ask questions. I believe that the main thing in relationships with children is honesty, so I explain everything to them. They help me look after her, play with her, and do educational exercises together. They worry about her when she needs injections. We call them power shots. The whole family is involved.
Treatment of PWS
Unfortunately, even in the 21st century the disease cannot be treated. Specialists can only make the disease easier for the patient. For example, if a baby has breathing problems, doctors put him on artificial ventilation. In case of swallowing impairment, the patient is prescribed enteral nutrition through a special tube. With reduced muscle tone, therapeutic massage or physiotherapy is necessary.
In rare cases, patients need a psychiatrist. Psychological assistance is especially needed for children with delayed psycho-emotional development and speech.
Human chorionic gonadotropin should also be replaced regularly. To stimulate timely sexual development, you need to take hormonal medications, and for boys you also need to have your testicles lowered.
Children with this syndrome need to be regularly administered somatotropin. It will relieve a person from the constant feeling of hunger, which means it will prevent obesity and help increase muscle gain. But in any case, parents, and sometimes a nutritionist, must monitor the child’s appetite.
Adults around the baby need to understand that his health directly depends on nutrition. And if even in preschool age you can practically not limit the child’s diet, then already in primary school it is necessary to provide a low-fat diet, the calorie content of which should not exceed daily expenses. During the period of active treatment for detected obesity - up to 1000 kcal.
It is advisable to hide all products from the child, or lock the refrigerator. Children with Prader-Willi syndrome should exercise a lot, play a variety of sports, and go for evening walks as often as possible. They need to be registered with a neurologist and endocrinologist.
Retinoblastoma
Retinoblastoma is a malignant tumor of the retina. The development process usually begins in childhood, and the starting material is tissue of embryonic origin. The peak phase occurs at two years of age.
Almost all known cases are detected during the first 5 years of life.
The cause of the disease in most cases is a mutation in the genetic material. In this case, it is necessary to have a genetic condition due to the presence of a mutant version of the Rb gene, obtained by inheritance. The second tumor-causing mutation occurs in the retinoblast.
There is a small chance that parents who have had retinoblastoma may have children with no pathological changes.
There are unilateral and bilateral cases of retinoblastoma. According to statistics, for the bilateral form the probability of hereditary origin is noticeably higher.
Symptoms of the disease include eye pain, glowing pupils, and loss of vision. It is very, very difficult to identify them in a small child.
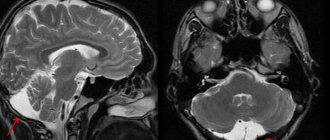
Diagnosis usually takes the form of an examination under anesthesia using ultrasound, CT and MRI. A fairly common procedure is a red bone marrow biopsy and spinal puncture. There are 5 groups based on the severity of symptoms.
There are two effective treatment methods. With cryotherapy and photocoagulation, it remains possible to preserve both vision and the eye itself. Complications with their use rarely occur. However, if a relapse occurs, the treatment will need to be repeated in the same form. Typically cryotherapy is used in cases where the anterior retina is damaged. For the posterior region, photocoagulation appears to be the preferred option.
Needs of people with PWS
Any person sooner or later needs medical care, treatment of various diseases and strengthening his immunity and health in general. Patients with Prader-Willi syndrome are no exception. But patients often encounter the following barriers to health:
- Difficulties in communicating and understanding with others;
- Insufficient mobility due to obesity;
- Mental disorders;
- Little knowledge of society about the disease;
- Lack of special schools for children with PWS.
Diagnostic measures
Early diagnosis of Prader-Willi syndrome and subsequent treatment can improve the prognosis of the disease. The diagnosis is made, as a rule, on the basis of the clinical manifestations of the disease, but today genetic testing is often used, which experts recommend primarily for newborns. This is due to the fact that in children the presence of the syndrome is much more difficult to determine, since it is impossible to test their ability to diagnose Prader-Willi syndrome based on clinical manifestations. Genetic testing is carried out using the DNA methylation method to determine whether abnormalities are present on chromosome 15 that lead to the onset of the disease. This method of diagnosing Prader-Willi syndrome helps to identify 97% of cases of the disease. It is also worth noting that the disease is often misdiagnosed, since it is often confused with Down syndrome, which is much more common. In addition, such a characteristic sign of Prader-Willi syndrome as obesity may also be present in Down syndrome. For this reason, a huge number of cases of the disease remain undetected.
Complications
Prader-Willi syndrome itself is usually not life-threatening. Timely therapy helps people live to at least 60 years of age. But if treatment is absent or prescribed incorrectly, the following complications may occur:
- Heart failure;
- Diabetes;
- Spinal diseases;
- Malignant tumors, incl. leukemia;
- Diseases of the respiratory system and nervous system (breathing apnea during sleep is especially dangerous);
- Destruction of cartilage due to excess weight.
Pathogenesis
The pathogenesis of the disease remains poorly understood to date.
There are suggestions that obesity accompanying Prader-Willi syndrome is caused by very low processes of fat breakdown (lipolysis) and increased synthesis of fat from acetate by more than 10 times.
Hypogonadism, developing according to the hypogonadotropic type, is associated with dysfunction of the hypothalamus (presumably, the pathology affects the areas of the ventromedial and ventrolateral nuclei). This theory is confirmed by the effectiveness of treating patients with clomiphene, which promotes the secretion of gonadotropins.
The hypopigmentation of the skin, hair and iris characteristic of patients is explained by a decrease in the activity of tyrosinase, an enzyme containing copper and catalyzing the oxidation of phenols, in the hair follicles and in the cells that produce melanin.
The 2nd phase of the disease is characterized by a deficiency of growth hormone (GH) caused by dysfunction of the hypothalamus.
Prader–Willi syndrome occurs due to imprinting. The determination of the expression of alleles that occurs due to this process is associated with their origin (either the father's gene or the mother's gene is always expressed). As a result of the lack of expression of the alternative form of the gene (paternal), the pathogenic mutant allele of the mother is expressed in the child’s phenotype.
The beginning of the imprinting process is associated with the process of gamete formation. In the potentially inactive allele of the embryo genome, cytosine methylation occurs and CpG islands are formed in the DNA, which consist of guanine (G) and methylated cytosine (C) pairs. Due to methylation in the promoter region of the repressed gene, abortive (short, resulting from premature cessation of synthesis) RNA is formed, which is necessary for gene suppression. Thus, through methylation, the gene is marked for imprinting.
The occurrence of uniparental disomy is influenced by the age of the mother (it affects conceptions with trisomy or monosomy of chromosome 15). Such cases are explained by maternal nondisjunction, in which the homologous chromosomes of a pair do not separate, but are directed to one pole of the cell. After fertilization of such a gamete, a zygote is formed containing an odd number of chromosomes.
In many cases, the extra chromosome is removed before the embryo begins to develop. Since the mechanism for removing an extra chromosome does not take into account its origin, only in 66% of cases the cell gets rid of one of the maternal chromosomes, and in the rest the only paternal chromosome is removed.
Prader-Willi syndrome in 10% of cases occurs as a result of chromosomal rearrangement (translocation) in the region critical for the syndrome. Observations of families of patients with similar translocations showed a high risk of relapse (about 50%) and the dependence of the phenotype on the sex of the parent transmitting the chromosome.
The Prader–Willi syndrome phenotype occurs in 2–5% of cases due to imprinting defects. Defects that include division into two parts of the imprinting center within the 15th chromosome (region q11-q13) lead to a change in the epigenotype of the chromosome of one of the parents. These defects are often associated with deletion (loss) of the imprinting center, and in some cases with an epigenetic mutation that does not cause a change in the DNA nucleotide sequence.
In all cases, the identified defects lead to changes in DNA methylation, disturbances in chromatin structure and the content of transcripts of a given gene in various cells.
Deletions in the imprinting center are associated with a 50% risk of relapse (the risk depends on the sex of the parent who transmitted the anomaly), and in the absence of a deletion the risk of relapse is low.
Currently, genes that are affected by genomic imprinting on chromosome 15 (region q11-q13) have been identified only for Angelman syndrome. According to scientists, Prader–Willi syndrome is associated with genes in the cluster of non-coding small nucleolar RNAs (snoRNAs) or with protein-coding genes SNURF – SNRPN (located in the area of the imprinting center) and Necdin.
Prevention
It is impossible to prevent a congenital disease; the main thing in this case is to prevent complications from occurring. Treatment of the syndrome should begin as early as possible, then it will be easier for the child to adapt to school and life in society.
Prevention of the disease includes medical and genetic consultations for families who have a predisposition to the occurrence of the syndrome. Expectant parents need to conduct a prenatal genetic study, which will help determine the structural features of the fetal chromosomes.
To improve the life of a child with PWS, constant cooperation between medical specialists, parents and the child himself should be ensured.
How do your husbands support you?
Marina A.: I couldn’t have done it without my husband and his support. When I found out about the diagnosis, I called him and cried, and he said: “I don’t understand why you react this way, nothing bad happened, we’ll handle everything.” At that moment he gave me incredible strength. My husband is my biggest support. And we have a very large and loving family, it gives an unshakable feeling of care and protection, endless love and tenderness. Robert definitely feels this.
Marina V.: My husband helps me both psychologically and physically. Always ready to pick up. He is very active with children, and they are not afraid of anything in this life. He does not treat Christina like some unhealthy child - he plays, tickles, and throws her in the same way. But we understand that there are families who do not have this, and men leave. We want to show positive experience that you can still live like this.
Forecast
Most often, the prognosis is directly determined by the presence of diseases of the heart, respiratory system, kidneys and the state of the endocrine system. According to established statistics, the life expectancy of people with Prader-Willi syndrome who received insufficiently active treatment is about 30 years. But there are also many cases where people lived 50-60 years. The main thing is to register with a doctor, follow his instructions, and regularly undergo all the necessary tests.
Positive effects of some deletions on viability
Small deletion changes can have a significant impact on the survival of the organism. For example, the loss of the gene encoding the CCR5-δ32 protein causes immunity to the human immunodeficiency virus. Scientists suggest that this mutation first appeared about 2.5 thousand years ago and over time spread across Europe.
The current distribution is uneven. According to statistics, about 10% of residents of European countries are resistant to HIV. However, in the Scandinavian countries this figure reaches 14-15 percent. Russians and Finns demonstrate a 16 percent level of resistance. For Sardinia, however, the frequency is a modest 4 percent.
A number of scientists have hypothesized that such a spread is determined by the bubonic plague epidemics that took place in the medieval period. It is likely that a mutation in the gene causes increased resistance to this disease. Therefore, in the countries where the Black Death took place, more people with this genotype survived.
References
- ^ a b
"Prader-Labhardt-Willi syndrome".
Whonamedit?
. Archived from the original on August 21, 2021. Retrieved August 20, 2016. - Cortes M., F.; Allende R, MA; Barrios R, A; Curotto L, B; Santa Maria V, L; Barraza O, X; Troncoso A, L; Mellado S, C; Pardo, V., R. (January 2005). "[Clinical, genetic and molecular features in 45 patients with Prader-Willi syndrome]". Revista Médica de Chile
.
133
(1):33–41. Doi:10.4067/s0034-98872005000100005. PMID 15768148. - ^ a b c d f g g h i j k l m p o
“Prader-Willi syndrome”.
A Home Guide to Genetics
. June 2014. Archived from the original August 27, 2021. Retrieved August 19, 2021. - ^ a b c
"Is there a cure for Prader-Willi syndrome (PWS)?".
NICHD
. January 14, 2014. Archived from the original August 27, 2021. Retrieved August 20, 2021. - Teitelbaum, Jonathan E. (2007). On the page: Pediatrics
. Lippincott Williams and Wilkins. item 330. ISBN 9780781770453. - ^ a b c d f g d
"What are the treatments for Prader-Willi syndrome (PWS)?".
NICHD
. January 14, 2014. Archived from the original August 10, 2021. Retrieved August 20, 2021. - ^ a b
"How many people have/are at risk of Prader-Willi syndrome (PWS)?".
NICHD
. January 14, 2014. Archived from the original August 27, 2021. Retrieved August 20, 2021. - "Prader-Willi Syndrome (PWS): Other Frequently Asked Questions." NICHD. January 14, 2014. Archived from the original July 27, 2021. Retrieved August 19, 2021.
- "Angelman Syndrome". Genetic Home Guide
. May 2015. Archived from the original August 27, 2021. Retrieved August 20, 2021. - Mia, Mary Mohan (2016). Classical and molecular genetics
. American academic press. p. 195. ISBN 978-1-63181-776-2. Archived from the original dated September 11, 2017. - Jorde, Lynn B.; Carey, John S.; Bamshad, Michael J. (2015). Medical genetics
(5th ed.). Elsevier Health Sciences. paragraph 120. ISBN 978-0-323-18837-1. - "Mayo Clinic Diseases and Conditions." Prader-Willi syndrome, symptoms and causes
. Retrieved February 6, 2021. - ^ a b c d e
Cassidy, Suzanne B. Driscoll, Daniel J (September 10, 2008).
"Prader-Willi syndrome." European Journal of Human Genetics
.
17
(1): 3–13. doi:10.1038/ejhg.2008.165. PMC 2985966. PMID 18781185. - ^ a b
Curfs LM, Fryns JP (1992).
"Prader-Willi syndrome: a review with special attention to the cognitive and behavioral profile." Birth defects Orig.
Artic. Ser .
28
(1):99–104. PMID 1340242. - ^ a b c
Cassidy S.B.
(1997). "Prader-Willi syndrome." Journal of Medical Genetics
.
34
(11): 917–23. Doi:10.1136/jmg.34.11.917. PMC 1051120. PMID 9391886. - ^ a b c d
Udvin O. (November 1998). "Prader-Willi syndrome: psychological and behavioral characteristics." Contact family. Archived from the original on July 16, 2011. - Holm, W. A., Cassidy, S. B., Butler, M. G., Hanchett, J. M., Greenswag, L. R., Whitman, B. B., Greenberg, F. (1993). "Prader-Willi syndrome: consensus diagnostic criteria". Pediatrics
.
91
(2):398–402. PMC 6714046. PMID 8424017. - Whittington, J., Holland, A., Webb, T., Butler, J., Clark, D., Boer, H. (February 2004). "Cognitive ability and genotype in a population-based sample of people with Prader-Willi syndrome." J Intellect Disabil Res
.
48
(Pt 2): 172–87. Doi:10.1111/j.1365-2788.2004.00556.x. PMID 14723659. - Bur, H; Holland, A; Whittington, J; Butler, J; Webb, T; Clark, D. (January 12, 2002). "Psychotic illness in individuals with Prader Willi syndrome due to maternal uniparental disomy of chromosome 15." Lancet
.
359
(9301):135–6. Doi:10.1016/S0140-6736(02)07340-3. PMID 11809260. S2CID 21083489. - ^ a b c
"What are the treatments for Prader-Willi syndrome (PWS)?". Archived from the original July 6, 2021. Retrieved June 16, 2021. - ^ a b c
Nordqvist, Christian (15 March 2010).
“What is Prader-Willi syndrome? What causes Prader-Willi syndrome? Medical news today
. MediLexicon International. Archived from the original January 16, 2013. Retrieved December 4, 2012. - Cummings DE, Clement K, Purnell JQ, Vaisse C, Foster KE, Frayo RS, Schwartz MW, Basdevant A, Weigle DS (July 2002). "Elevated plasma ghrelin levels in Prader-Willi syndrome." Nature Medicine
.
8
(7): 643–4. doi:10.1038/nm0702-643. PMID 12091883. S2CID 5253679. - Clark DJ, Boer H, Webb T (1995). "General and behavioral aspects of PWS: a review." Mental Health Research
.
8
(195): 38–49. - Cassidy S. B., Devi A., Mukaida S. (1994). "Aging in PWS: 232 patients over 30 years of age." Proc.
Greenwood Genetics Center .
13
: 102–3. - Hered RW, Rogers S, Zang YF, Biglan AW (1988). "Ophthalmological features of Prader-Willi syndrome." J Pediatrician ophthalmol strabismus
.
25
(3): 145–50. PMID 3397859. - Buting, K; Saito, S; Gross, S; Dittrich, B; Schwartz, S; Nicholls, R.D.; Horsthemke, B. (April 1995). "Inherited microdeletions in Angelman and Prader-Willi syndromes identify an imprinting center on human chromosome 15." Nature Genetics
.
9
(4): 395–400. Doi:10.1038/ng0495-395. PMID 7795645. S2CID 7184110. - "Major breakthrough in understanding Prader-Willi syndrome, a parental imprinting disorder." medicalxpress.com. Archived from the original April 28, 2015. Retrieved June 18, 2015.
- Online Mendelian Inheritance in Man (OMIM): Prader-Willi Syndrome; PWS - 17627
- de los Santos T, Schweizer J, Rees CA, Francke U (November 2000). "A small evolutionarily conserved RNA resembling small nucleolar C/D box RNA is transcribed from PWCR1, a novel imprinted gene in the Prader-Willi deletion region that is highly expressed in the brain." American Journal of Human Genetics
.
67
(5):1067–82. Doi:10.1086/303106. PMC 1288549. PMID 11007541. - Cavaillé J, Buiting K, Kiefmann M, Lalande M, Brannan CI, Horsthemke B, Bachellerie JP, Brosius J, Hüttenhofer A (December 2000). "Identification of brain-specific and imprinted small nucleolar RNA genes exhibiting unusual genomic organization." Proc.
Natl. Academician Sci. UNITED STATES OF AMERICA .
97
(26):14311–6. Bibcode:2000PNAS ... 9714311C. doi:10.1073/pnas.250426397. PMC 18915. PMID 11106375. - "Prader-Willi Syndrome - MeSH - NCBI." National Center for Biotechnology Information. US National Library of Medicine, n.d. Online. November 1, 2021. "Prader-Willi Syndrome - MeSH - NCBI." Archived from the original November 3, 2021. Retrieved November 1, 2016.>.
- Cassidy, S. B.; Dykens, E (2000). "Prader-Willi and Angelman syndromes: nursing imprinted disorders." Am J Med Genet
.
97
(2): 136–146. Doi:10.1002/1096-8628(200022)97:2 3.0.co; 2-v. PMID 11180221. - Runte, M., Varon, R., Horn, D., Horsthemke, B., Buyting, K. (2005). "Exclusion of the HBII-52 C/D box snoRNA gene cluster from a major role in Prader-Willi syndrome." Hum Genet
.
116
(3):228–30. Doi:10.1007/s00439-004-1219-2. PMID 15565282. S2CID 23190709. - Scriabin B.V., Gubar L.V., Seeger B., Pfeiffer J., Handel S., Robek T., Karpova E., Rozhdestvensky T.S., Brosius J. (2007). "Deletion of the MBII-85 snRNA gene cluster in mice results in postnatal growth retardation." PLOS Genet
.
3
(12):e235. doi:10.1371/journal.pgen.0030235. PMC 2323313. PMID 18166085. - Sahu T, del Gaudio D, Herman Jr, Shinawi M, Peters SU, Person RE, Garnica A, Chung SW, Bode AL. (2008). "Prader-Willi phenotype caused by paternal deficiency for the small HBII-85 C/D box nucleolar RNA cluster." Nat Genet
.
40
(6): 719–21. doi:10.1038/ng.158. PMC 2705197. PMID 18500341. - Ding, F., Li, H. H., Zhang, S., Solomon, N. M., Kamper, S. A., Cohen, P., Frank, W. (March 2008). "Deletion of SnoRNA Snord116 (Pwcr1/MBII-85) causes growth deficiency and hyperphagia in mice." PLOS ONE
.
3
(3):e1709. Bibcode:2008PLoSO...3.1709D. Doi:10.1371/journal.pone.0001709. PMC 2248623. PMID 18320030. - Ding F, Prints Y, Dhar MS, Johnson DK, Garnacho-Montero C, Nicholls RD, Francke U (2005). "Lack of Pwcr1/MBII-85 snRNA is critical for neonatal lethality in Prader-Willi syndrome mouse models." Mamm genome
.
16
(6): 424–31. Doi:10.1007/s00335-005-2460-2. PMID 16075369. S2CID 12256515. - de Smith AJ, Purmann C, Walters RG, Ellis RJ, Holder SE, Van Haelst MM, Brady AF, Fairbrother UL, Dattani M, Keogh JM, Henning E, Yeo GS, O'Rahilly S, Froguel P, Farooqi IS, Blakemore AI (June 2009). “Deletion of the HBII-85 class of small nuclear RNAs (snRNAs) is associated with hyperphagia, obesity, and hypogonadism.” Hm.
Mol. Genet .
18
(17): 3257–65. Doi:10.1093/hmg/ddp263. PMC 2722987. PMID 19498035. - ^ a b
Killeen, Anthony A. (2004).
"Genetic Inheritance". Principles of Molecular Pathology
. Humana Press. paragraph 41. ISBN 978-1-58829-085-4. Archived from the original dated June 29, 2014. - Davies, P. S., Evans, S., Broomhead, S., Clough, N., Day, J. M., Laidlaw, A., Barnes, N. D. (May 1998). "Effects of growth hormone on height, weight, and body composition in Prader-Willi syndrome." Arch.
Dis. Child .
78
(5): 474–6. Doi:10.1136/adc.78.5.474. PMC 1717576. PMID 9659098. - Carrell A.L., Myers S.E., Whitman B.A., Allen D.B. (April 2002). "Benefits of Long-Term GH Therapy in Prader-Willi Syndrome: A 4-Year Study." J. Clin.
Endocrinol. Metab .
87
(4):1581–5. doi:10.1210/jc.87.4.1581. PMID 11932286. - Höybye C, Hilding A, Jacobsson H, Thorén M (May 2003). "High hormone treatment improves body composition in adults with Prader-Willi syndrome." Clin.
Endocrinol .
58
(5): 653–61. Doi:10.1046/j.1365-2265.2003.01769.x. PMID 12699450. S2CID 6941937. - Scheimann, AO; Butler, M. G.; Gurash, L; Cuffari, C; Klish, Z (January 2008). "A critical analysis of bariatric procedures for Prader-Willi syndrome." Journal of Pediatric Gastroenterology and Nutrition
.
46
(1):80–3. Doi:10.1097/01.mpg.0000304458.30294.31. PMC 6815229. PMID 18162838. - Tweed, Catherine (September 2009). "Shawn Cooper Fights Prader Willi Syndrome." AOL Health. Archived from the original on September 9, 2009. Retrieved September 9, 2009.
- Mary Jones. “Case Study: Cataplexy and SOREMP without Excessive Daytime Sleepiness in Prader-Willi Syndrome. Is this the onset of narcolepsy in a five year old? European Society of Sleep Technologists. Archived from the original April 13, 2009. Retrieved April 6, 2009.
- "Dog eat dog." Csifiles.com. Archived from the original June 4, 2009. Retrieved June 12, 2009.
- “I can’t stop eating.” Channel4.com. 2006. Archived from the original July 25, 2009. Retrieved June 12, 2009.
- "Extreme Makeover: Articles for Home Edition on AOL TV." Aoltv.com. Archived from the original on September 23, 2015. Retrieved June 18, 2015.
- [1] Archived July 14, 2014 Wayback Machine