This site was made by experts: toxicologists, narcologists, hepatologists. Strictly scientific. Tested experimentally.
Author of this article, expert: Gastroenterologist-hepatologist Ekaterina Kashukh
In short: Untreated hepatitis, cirrhosis and other liver diseases lead to severe damage to the organ and nervous system. Hepatic encephalopathy will develop, which ends in hepatic coma. The later the patient went to the doctor, the less likely he was to be saved.
- Causes of hepatic coma development
- Symptoms of disease development
- How a patient is treated
- Prognosis for hepatic coma
Hepatic coma represents the final stage in the progression of liver failure. This condition can occur during the progression of acute and chronic liver diseases. This is usually a manifestation of severe liver cirrhosis. As a result of the development of a coma, symptoms of damage to the central nervous system appear.
What is hepatic coma
Hepatic coma is a serious condition of the body that developed as a result of acute inflammatory processes and chronic liver diseases. Despite the fact that many are immediately placed under emergency hospitalization, the survival prognosis for such a diagnosis is disappointing.
The disease is accompanied by loss of consciousness, lack of natural reflexes, and circulatory disorders. Hepatic coma does not occur as a separate disease; it is a complication of long-term disturbances in the functionality of the organ. It is often preceded by chronic failure, in which there was no appropriate treatment and health maintenance.
A serious condition develops when metabolic products (phenols, ammonia, etc.) accumulate in the body, which must be eliminated naturally. Due to their accumulation, a toxic effect occurs that affects the brain. That is why hepatic coma affects the functioning of the central nervous system, namely, the inhibition of its functions.
Hepatic coma (acute liver dystrophy)
Hepatic coma is a neurophysiological syndrome that is the final stage of liver failure. The disease is accompanied by a severe disorder of the central nervous system: impaired consciousness, pathology of reflexes, and respiratory paralysis.
Hepatic coma is characterized by high mortality even with intensive care. Severe brain dysfunction is reported in approximately 30% of patients with liver failure. Cerebral edema is the main cause of death in 82% of patients.
CAUSES OF HEPATIC COMA
Most often, the cause of hepatic coma is a dysfunction of the liver due to a chronic disease (cirrhosis, hepatitis, cancer, etc.). The work of an organ can also be undermined by:
- gastrointestinal bleeding;
- long-term alcohol abuse;
- sepsis;
- diffuse peritonitis;
- taking certain medications (anti-inflammatory, anti-tuberculosis, etc.);
- long-term surgery.
When exposed to poisons (poisoning with mushrooms, alcohol, industrial poisons), viral hepatitis, severe infectious diseases, surgical shock, fulminant liver failure can develop, which in a short time leads to hepatic coma.
PATHOGENESIS OF HEPATIC COMA
Hepatic coma is characterized by:
- accumulation of cerebrotoxic substances in the blood: ammonia, phenols, short chain acids (fatty), mercaptan;
- decreased sugar levels (hypoglycemia), which leads to energy deficiency in the brain;
- a change in acid-base balance, which clears the way for ammonia to penetrate into cells;
A patient with hepatic coma has impaired consciousness - hypoxemia (low levels of oxygen in the blood);
- kidney dysfunction leading to metabolic encephalopathy (complete disruption of brain functionality).
SYMPTOMS AND STAGES OF HEPATIC COMA
Hepatic coma goes through three stages, which are preceded by severe headache, inability to eat due to loss of taste, and burning of the skin.
- Precoma is an initial condition characterized by sleep disturbances, causeless euphoria or sadness, and inhibited thinking. Physiological symptoms include sweating, cold hands, liver odor, fever, sometimes jaundice, pain in the epigastric region (stomach). Dialogue with the patient is still possible;
- A threatening condition for the patient . Loss of consciousness and orientation in space, memory lapses, slowdown of speech processes, delirium. Depression, severe agitation, hallucinations. Reflexes are impaired: this manifests itself in muscle twitching, numbness, and convulsions.
- To whom. The person loses consciousness, has no reflexes, and the muscles are rigid (resist any movement). Breathing is hyperventilation, pupillary response is absent, convulsions. The sphincters are paralyzed. Without medical care, respiratory paralysis occurs.
There is no clear answer as to how long this or that stage lasts. The duration depends on the individual endurance of the body and the adequacy of treatment of the concomitant disease.
In addition to neuropsychiatric symptoms, hepatic coma is accompanied by signs of hepatocellular failure. Characterized by yellowness of the skin, a typical liver odor, tachycardia, hyperthermia, hemorrhagic syndrome.
DIAGNOSIS OF HEPATIC COMA
It is better to diagnose hepatic coma in the presence of relatives, who can tell the doctor about the time of the first symptoms and the rate of their progression. Upon examination, the doctor discovers yellowness of the skin and a liver odor from the mouth.
To correct oxygen deprivation of the brain, a patient in a hepatic coma is given intravenous glucose.
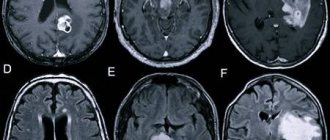
To identify signs of hepatocellular failure, laboratory tests (biochemical, clinical blood tests) are needed. An electroencephalogram allows you to assess the functional activity of the brain. Additionally, computed tomography, MRI of the brain, and magnetic resonance spectroscopy may be prescribed.
TREATMENT FOR HEPATIC COMA
A patient in a state of hepatic coma should be urgently hospitalized in the intensive care unit. Speed of action is extremely important, as this condition threatens human life. Doctors need to quickly establish the cause of the coma and eliminate the etiological factor.
First steps for hepatic coma:
- heart rate and ECG monitoring;
- control of intracranial pressure;
- artificial ventilation;
- deep sedation with fentanyl and propofol;
Timely visit to the doctor and treatment will help to avoid the serious consequences of gastrointestinal diseases - intravenous administration of glucose solution to correct oxygen starvation of the brain;
- with a strong decrease in hemoglobin levels, blood transfusion is indicated.
To treat intracranial hypertension and cerebral edema, which are observed in 85% of patients, mechanical ventilation, sedation and restoration of electrolyte and blood gas composition are used. Antibiotics are used to prevent infection.
In a state of hepatic coma, a person experiences stress damage to the mucous membrane of the digestive tract. To prevent gastrointestinal bleeding, the patient is prescribed gastroenteroprotectors based on rebamipide (Rebagit) and proton pump inhibitors (PPIs).
To ensure that ammonia is less absorbed in the intestines and does not damage the brain as much, lactulose preparations are used. To speed up bowel movements, enemas with a solution of magnesium sulfate are given. Of course, therapy with hepatoprotectors (ursodeoxycholic acid, ursosan) is prescribed to increase the protection of liver cells.
For end-stage liver failure and coma, the only effective treatment is liver transplantation.
FORECAST AND PREVENTION
Survival rate for hepatic coma does not exceed 20%, the highest mortality is observed among patients under the age of 10 years and over 40.
Prevention of hepatic coma consists of:
- Adequate treatment of liver diseases;
- Taking medications only as prescribed by a doctor;
- Excluding self-treatment with medications, as well as folk remedies (herbs, decoctions, tinctures, etc.);
- Preventing poisoning by toxic substances, using personal protective equipment (PPE);
- Proper nutrition, limiting alcohol.
Kinds
Depending on the clinical manifestations, there are several types of hepatic comas:
- Endogenous type. Toxic substances are contained in large quantities in the blood, are produced in it, and are carried through the bloodstream throughout the body. The main cause of endogenous coma is toxic liver damage. They often appear in chronic alcoholism, when metabolic acidosis develops, then alkalosis, and later the effect of poisons affects the brain.
- Exogenous type. Toxic substances enter directly into the blood, leaving the liver itself unaffected. Exogenous coma often develops in liver diseases with pronounced portocaval anastomoses.
- Mixed type. It means a combination of endogenous and exogenous factors. At the same time, the amount of toxic substances in the body increases rapidly, they are in the bloodstream, various organs of the gastrointestinal tract, and brain damage quickly occurs.
There is also a fourth type - false hepatic coma. The main reason for its development is potassium deficiency, which develops against the background of chronic cirrhosis of the liver. A person may take diuretics incorrectly or in excessive amounts, which flush out this substance. Potassium deficiency can also occur against the background of frequent diarrhea and vomiting, when the body is constantly struggling with dehydration. Metabolic alkalosis gradually develops, due to which ammonia cells penetrate into the brain and affect it.
Stages and symptoms
The severe condition of the body during hepatic coma develops gradually. The intensity of progression of inflammatory processes depends on the causes that provoke them, the general condition of the human body, the presence of chronic diseases, and other factors.
The following stages of coma are distinguished:
- Prekoma. Symptoms of hepatic coma at this stage affect the mental state of the person. He develops increased anxiety, melancholy, unjustified fears, sleep disturbances, and decreased performance. Confusion and loss of consciousness occur periodically. From the gastrointestinal tract, nausea, vomiting, and frequent abdominal pain are observed.
- Threatening stage (decompensated). It is characterized by severe disturbances of consciousness, in which a person cannot control himself. Fainting, hallucinations, and memory loss often occur. Coordination of movements is seriously impaired, it is difficult for a person to walk in a straight line, he gets tired quickly, his hands tremble all the time. Difficulty in breathing appears - it becomes noisy and intermittent.
- Complete coma. The person completely loses consciousness, reflexes, including pathological ones, are absolutely absent. The skin acquires a pronounced yellow color, which allows doctors to quickly determine the cause of the lack of consciousness. During diagnosis, it is discovered that the size of the liver is much smaller than normal.
In complete coma, various breathing disorders appear; Cheyne-Stokes breathing (with a constantly changing frequency) or Kussmaul breathing (deep, noisy) is more often diagnosed.
Signs of deterioration develop alternately, depending on the stage of the coma.
Causes
Hepatic coma is the most severe stage of hepatic encephalopathy, the algorithm for its development is the same in all cases:
Blood test indicators for liver cirrhosis
- metabolic processes are disrupted;
- metabolic products are not eliminated from the body naturally, they accumulate or toxins immediately enter the bloodstream;
- with an increase in their number, the poisons affect the central nervous system;
- When the brain is damaged by toxins, coma occurs.
There are many reasons why these processes occur, often acute or chronic liver diseases. These include hepatitis of various types (alcoholic, viral, toxic), cirrhosis, the appearance and increase of tumors in the liver, and all kinds of diseases associated with general intoxication.
A common cause is complications after portacaval shunt surgery.
There are also predisposing factors that themselves cannot cause such a severe pathological condition, but can contribute to its development against the background of acute or chronic liver diseases. These include:
- bad eating habits, abuse of fatty, fried, and other heavy foods;
- eating too much protein;
- prolonged diarrhea, vomiting, developed against the background of gastrointestinal diseases, which remain without proper treatment and lead to dehydration;
- frequent or uncontrolled use of diuretics;
- uncontrolled use of sedative drugs.
Some weight loss diets suggest taking diuretics daily. If you start taking them without a doctor's prescription, you can cause dehydration and deterioration of the liver, which will lead to serious consequences.
Viral hepatitis
Which doctors should I contact?
Any viral hepatitis is an infectious disease and is treated primarily by infectious disease doctors.
In addition, there are other specialists in liver diseases (gastroenterologists and hepatologists) who also take an active part in the treatment of patients suffering from viral hepatitis. Treatment of viral hepatitis
For mild acute hepatitis, treatment can be carried out on an outpatient basis; moderate and severe forms are treated in a hospital. In case of chronic pathology (beyond a significant exacerbation), treatment is carried out at home. In cases of severe exacerbation or decompensation, hospitalization in an infectious diseases hospital is indicated.
Basic treatment is prescribed, which includes a gentle regime and a specialized diet - exclude fried, smoked, pickled foods, refractory fats (pork, lamb), alcoholic and carbonated drinks. It is recommended to drink plenty of fluids (up to 2–3 liters per day).
Detoxification measures are used (intravenous administration of hemodez, glucose solution with vitamin C or Essentiale, lactulose is prescribed). If necessary, sorbents, hepatoprotectors, antioxidants, diuretics, probiotics, antihistamines, anti-inflammatory and hormonal agents, and vitamins are recommended.
Alpha interferon has immunomodulating and antiviral effects, inhibits the synthesis of viral proteins, and enhances the activity of natural killer cells in hepatitis B and C.
In the case of a chronic course of the disease, it may be necessary to prescribe drugs with direct antiviral action, leading to the complete disappearance of the hepatitis C virus or persistent suppression of viral replication in hepatitis B and D. The hepatitis B virus is able to integrate into human genetic material, and therefore completely recover from this disease fails. Treatment of hepatitis B with delta agent is one of the most difficult tasks in hepatology today.
Complications
Complications of viral hepatitis can include functional and inflammatory diseases of the biliary tract, as well as hepatic coma, which occurs due to massive necrosis of liver cells and leads to death in almost 90% of cases. Hepatitis B and C are dangerous due to the development of a chronic process and are the most common cause of cirrhosis and liver cancer.
The most severe course of the disease is caused by a combination of two or more viruses. In this case, the prognosis is extremely unfavorable. Often the signs of chronic viral hepatitis are mild, which allows a person to ignore the disease for the time being. Often, obvious clinical manifestations of the disease are detected already at the stage of liver cirrhosis.
In addition to the development of cirrhosis and liver cancer, a connection between chronic hepatitis C and B-cell lymphoma has been proven - damage to the endocrine glands, organs of vision, skin, muscles, joints, nervous system, and bile ducts.
Prevention of viral hepatitis
Today, the most effective method of preventing viral hepatitis is vaccination:
- The hepatitis A vaccine is administered twice and provides protection against the disease for up to 20 years. In Russia, vaccination against viral hepatitis A is included in the National Calendar of Preventive Vaccinations for epidemic indications.
- Vaccination against hepatitis B (N532) protects not only against the hepatitis B virus, but also against the delta agent. In Russia, vaccination is carried out within the framework of the National Calendar of Preventive Vaccinations. If no contraindications are identified for the newborn, the first vaccination is given in the maternity hospital, on the first day of life. The second one is done one month later, and the third one 6 months after the start of vaccination.
- There is no specific vaccine against hepatitis C. Several vaccines are in development.
Nonspecific prevention of viral hepatitis includes ensuring food and water safety (hepatitis A and E), careful testing of donor blood, sterile injection equipment and infection control (hepatitis B and C).
Hepatitis prevention measures are simple and accessible:
- Strict adherence to the rules of personal hygiene: washing hands before eating, after visiting the toilet, when returning from work, walking, refusing to use someone else’s manicure tool, toothbrush, razor.
- Avoid contact with the biological fluids of strangers. When treating wounds, use disposable gloves.
- Wash vegetables, berries, fruits, greens under strong pressure of tap water, rinse with boiled water.
- Drink only boiled or bottled water. Do not swim in polluted waters.
- If parenteral hepatitis is detected, it is necessary to examine the sexual partner and follow all prescriptions of the attending physician.
- Avoid contact with used syringes, needles and other medical and non-medical equipment.
Sources:
- ;
- ;
- ;
- ;
- ;
- ;
- ;
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment. In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor.
Diagnostics
The sooner the diagnosis is made and the causes of a person’s serious condition are established, the greater the likelihood of a successful recovery. During precoma, that is, the first stage, patients often go to the clinic themselves for help; during the second stage, it is difficult for them to even get to the hospital. Having noticed the first signs of precoma in yourself or your loved ones, it is important to react immediately, before consciousness is lost and other complications develop.
Changes in mental state (depression, apathy, fears, etc.) are often a cause for concern; a person is encouraged to go to the hospital by relatives
Diagnostics includes the following laboratory and instrumental studies:
- Psychometric testing. With the help of tests, an experienced doctor will immediately detect changes in the activity of the central nervous system and assess the degree of their development.
- Blood analysis. Due to metabolic alkalosis, the level of ammonia in the blood increases, which can be determined by passing a clinical test or biochemistry.
- Cerebrospinal fluid analysis. It increases the protein level and some others.
- MRI. Allows you to assess the condition of the brain, the degree of its damage, and morphological changes in its tissues.
The patient is examined urgently, regardless of the stage of development of the coma. The duration of each of them may be short and the person’s condition will deteriorate sharply.
Hepatic encephalopathy (HE), or portosystemic encephalopathy, is a potentially reversible syndrome of brain dysfunction in patients with progressive liver failure. However, P.E. is not a single category and may reflect the clinical manifestations of reversible metabolic encephalopathy, brain atrophy due to hepatocerebral dystrophy, cerebral edema, or any combination of these conditions. The mechanisms that impair brain function in liver failure are still not fully understood, but it is clear that they are directly related to liver failure and impaired ammonia metabolism. If the underlying liver disease is not curable, PE is associated with poor survival and a high risk of relapse [1, 2]. Even in its mildest form, PE reduces health-related quality of life and is a risk factor for episodes of severe PE [3, 4].
Pathogenesis
Despite more than 100 years of research, the pathogenesis of PE is still not entirely clear. This is mainly due to the difficulty of studying the brains of patients with PE in vivo
. Most published data come from experimental models of PE, which are far from perfect. The most common hypotheses for pathogenesis reflect the role of neurotoxins, impaired neurotransmission due to metabolic disturbances in liver failure, changes in brain energy metabolism, amino acid imbalance, systemic inflammatory response and disturbances in the permeability of the blood-brain barrier [5–7]. Various hypotheses for the pathogenesis of PE are not mutually exclusive. It is likely that many of the described disorders may act simultaneously and ultimately lead to the development of PE.
Neurotoxins.
The most studied neurotoxin associated with HE is ammonia, which is produced primarily in the gastrointestinal tract and travels through the portal vein to the liver. A healthy liver detoxifies incoming ammonia by converting it into glutamine, thereby preventing it from entering the systemic circulation. With progressive liver diseases, an increase in the concentration of ammonia in the blood occurs both as a result of a violation of its conversion by the liver into glutamine, and as a result of porto-systemic shunting, in which blood, bypassing the liver, enters the systemic circulation [3].
When the concentration of ammonia in the blood increases, it penetrates the blood-brain barrier and has a neurotoxic effect primarily on astrocytes, the most numerous cells in the brain, closely associated with the functioning of neurons. A key mechanism for the development of PE is astrocyte swelling due to hyperammonemia [8–11].
Excess ammonia leads to the accumulation of glutamine formed in astrocytes, which is accompanied by an increase in intracellular osmolarity and in high concentrations causes brain edema [12].
Impaired neurotransmission.
Impaired functioning of cerebral cortex neurotransmitters and their receptors plays an important role in the pathogenesis of PE. Abnormalities in several neurotransmitter systems have been studied in experimental models of liver failure. Most of these studies describe changes in the GABAergic neurotransmitter system, dopaminergic, serotonergic and glutamatergic neurotransmitter systems [13, 14]. In particular, the role of GABAergic influences in the development of PE may be associated with the activation of benzodiazepine receptors in the brain and the associated increase in the synthesis of neurosteroids [15].
Amino acid imbalance.
An important role in the pathogenesis of PE is played by amino acid imbalance in the form of an increase in the level of aromatic amino acids (tyrosine, phenylalanine, tryptophan), which are precursors of false neurotransmitters, and a decrease in the content of branched-chain amino acids (valine, leucine, isoleucine). Under these conditions, there is an excessive supply of aromatic amino acids to the brain, which serve as the starting product for the synthesis of false neurotransmitters. These changes in amino acid composition are also accompanied by a decrease in dopamine synthesis, which also contributes to the formation of false neurotransmitters [16].
Clinic
The clinical picture of PE is a wide range of nonspecific neurological and mental disorders [17]. Signs of encephalopathy in patients with chronic liver diseases depend on the etiology of the underlying disease, the nature and severity of pathogenic factors.
The severity of PE varies from latent (stage 0) and mild (stage I) to coma (stage IV). With minimal PE, it is manifested mainly by disturbances in abstract thinking and a general mild decline in cognitive functions without impairments of memory, intelligence, speech, and learning ability, which remain intact for a long time [18, 19]. In some patients with liver failure, for a number of years only disorders of higher brain functions are detected without any other neurological symptoms [20].
As PE progresses, personality changes increase, such as apathy, irritability and decreased behavioral control, as well as obvious changes in consciousness and motor function [21]. Sleep-wake cycle disturbances with excessive daytime sleepiness are common, although complete sleep-wake cycle disruption is usually absent [22–24]. With increasing liver failure, progressive disorientation in time and space, behavioral disturbances develop, episodes of confusion with agitation or drowsiness, stupor and, finally, coma occur [25]. The consensus of the International Society for Hepatic Encephalopathy and Nitrogen Metabolism (ISHEN) considers the appearance of disorientation or asterixis (“flapping” tremor) as the initial signs of overt HE [26].
In noncomatose patients with PE, motor dysfunction such as muscle hypertonia, hyperreflexia, and a positive Babinski reflex is observed. As coma progresses, deep tendon reflexes usually decrease [27] and even disappear, although pyramidal signs may persist. Occasionally, focal neurological deficits may occur [28]. Convulsions in PE are very rare [29–31].
Frequent manifestations of the disease are extrapyramidal disorders in the form of facial hypomia, muscle rigidity, bradykinesia, hypokinesia, monotony and slow speech, Parkinson-like tremor and dyskinesia with limitation of voluntary movements [27].
Asterixis (“flapping tremor”) is often noted in the early and middle stages of PE, which precedes stupor or coma. It is not actually a tremor but a negative myoclonus and is caused by hyperextension of the patient's wrist with the fingers spread apart. It is noteworthy that mental and motor disorders in PE may be mild or do not progress equally in different patients, which leads to difficulties in determining the stage of PE.
Classification
According to the practical recommendations of the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver [32], PE is classified according to four criteria: depending on the reasons that led to its development; by duration and nature of the flow; according to the severity of the course (stages) and depending on the presence of provoking (trigger) factors.
A - hepatic encephalopathy as a result of acute liver failure;
B — portosystemic shunting in the absence of liver cirrhosis (LC);
C - hepatic encephalopathy in patients suffering from cirrhosis.
Classification of PE by duration and nature of the course:
1) episodic PE;
2) recurrent PE - these are attacks of PE that occur with a time interval of 6 months or less;
3) persistent PE represents behavioral disturbances that are constantly present and interspersed with relapses of overt PE.
Classification of the severity of PE by stages (West Haven scale)
I. Minimal (latent) stage: there are no clear clinical symptoms, but there is a violation of standardized psychomotor tests (number connection test, line test).
II. The first (mild) stage: apathy, excitement, irritability, anxiety, euphoria, fatigue, disturbances in the rhythm of sleep and wakefulness, mild tremor, impaired coordination of movements, asterixis.
III. Second (middle) stage: drowsiness, lethargy, disorientation in time and space, inappropriate behavior, asterixis, dysarthria, ataxia.
IV. Third (severe) stage: stupor, severe disorientation, unclear speech, hyperreflexia, the presence of pathological reflexes (Gordon, Zhukovsky), myoclonus, hyperventilation.
V. Stage four: hepatic coma, decerebrate rigidity, oculocephalic phenomenon, lack of response to any stimuli.
Depending on the presence of provoking (trigger) factors, PE is divided into unprovoked and provoked (in this case, the provoking factor must be indicated). It is advisable to identify precipitating factors (infections, gastrointestinal bleeding, diuretic overdose, electrolyte disturbances, constipation) for all episodes of type C HE and eliminate them if present.
Diagnostics
Diagnosis of obvious PE
The diagnosis of overt PE is based on an objective clinical examination. It involves assessing the symptoms of HE, as well as excluding other causes of brain dysfunction. In the clinical picture, patients with obvious PE have symptoms of diseases of the hepatobiliary system, for example, in most patients the development of PE is preceded by jaundice. A liver odor and hyperventilation can often be detected in patients with encephalopathy [33]. Also, the diagnosis of PE is confirmed by identifying provoking factors (infections, bleeding and constipation, etc.).
The “gold standard” for diagnosing overt PE is the West-Haven criteria, however, they have limited diagnostic value due to the subjectivity of the assessments, especially in stage I PE, since mild hypokinesia, psychomotor retardation and absent-mindedness can be missed during clinical examination. The leading diagnostic symptoms of obvious PE are the presence of disorientation and asterixis in the patient [32].
To describe the condition of patients with significantly altered consciousness, it is recommended to use the Glasgow Coma Scale (GCS). The Glasgow scale involves calculating points that reflect the severity of the patient's reaction to stimuli. The ability to open the eyes, the nature of motor and verbal reactions to simple stimuli (voice and pain) are determined. Coma is preceded by less profound forms of depression of consciousness: confusion, stupor and stupor.
Diagnosis of minimal PE
Minimal HE is defined as abnormal brain function detected by tests in patients with chronic liver disease who are not confused or have not developed asterixis. The examination of such patients may include two main types of tests: psychometric and neurophysiological. ISHEN recommends the use of at least two tests, depending on their availability and local conditions. The importance of testing for minimal HE is that it predicts the development of overt HE.
To diagnose minimal PE, it is recommended to carry out neurophysiological and psychometric tests, among which the most important are both simple ones performed on paper with a pen (psychometric scale of PE) and computerized ones (reaction time delay test, Stroop test, inhibitory control test and SCAN test ) and neurophysiological (critical flicker fusion frequency test) tests [32]. Electroencephalography can detect changes in cortical brain activity in PE, but this method is not specific enough, since it can be influenced by concomitant metabolic disorders and medications.
Laboratory tests.
In patients with PE, serum-biochemical liver syndromes of varying severity are detected, depending on the predominant direction of pathological processes in the liver [34].
Cytolysis syndrome, or hepatocyte damage syndrome (violation of integrity, necrosis of hepatocytes), is characterized primarily by an increase in aminotransferases (aspartate and alanine aminotransferase), as well as other enzymes - lactate dehydrogenase-5, aldolase, ornithine carbamyltransferase, sorbitol dehydrogenase, glutamate dehydrogenase.
Cholestasis syndrome is characterized by an increase in bilirubin, mainly conjugated (direct), alkaline phosphatase, gamma-glutamyl transpeptidase, 5-nucleotidase, cholesterol and bile acids.
Inflammation syndrome is characterized by increased levels of various globulin fractions, dysproteinemia, and increased levels of serum immunoglobulins.
The AASLD/EASL guidelines [32] note that in patients with chronic liver disease, only high blood ammonia levels have diagnostic or prognostic value. However, if ammonia levels are within normal limits, the diagnosis of PE is questionable. Repeated ammonia measurements may be used to assess the effectiveness of treatment when patients are taking medications that lower ammonia levels.
Computed tomography or magnetic resonance imaging and other imaging methods do not provide complete diagnostic information and are of limited value. They are mainly used to exclude structural damage to the brain in patients with cirrhosis.
Differential diagnosis
AASLD/EASL guidelines indicate the need to exclude other diseases that may resemble PE [32]:
1) diabetes mellitus (hypoglycemic, hyperglycemic and hyperosmolar coma, lactic acidosis);
2) alcohol abuse (intoxication, withdrawal syndrome, Wernicke syndrome);
3) overdose of drugs (benzodiazepines, antipsychotics, opioids);
4) neuroinfections and electrolyte disorders (hyponatremia, hypercalcemia);
5) non-convulsive epilepsy, mental illness;
6) intracerebral hemorrhage and ischemic stroke;
7) dementia (primary and secondary);
 brain damage (traumatic, neoplastic, normal pressure hydrocephalus, obstructive sleep apnea syndrome).
brain damage (traumatic, neoplastic, normal pressure hydrocephalus, obstructive sleep apnea syndrome).
Treatment
Treatment of PE includes elimination of precipitating factors, dietary measures and drug therapy. Elimination of precipitating factors is the primary goal in the treatment of overt PE, since in 90% of patients this is sufficient to improve the condition [32].
Diet
Correction of disorders of protein-nitrogen metabolism is crucial in the treatment of all degrees of PE, since 75% of patients with PE have moderate or severe protein-calorie deficiency, accompanied by loss of muscle mass. Long-term restriction of protein intake is harmful for patients with PE, since the protein requirement in these patients is relatively higher than in healthy individuals.
Therefore, according to the AASLD/EASL recommendations, daily energy intake should be maintained at 35–40 kcal per 1 kg of body weight, and daily protein intake should be within the range of 1.2–1.5 g/kg [32]. Limiting protein intake is recommended only during the first few days after the development of PE, but then this measure should be abandoned. Animal proteins should be replaced with milk and plant proteins, and foods enriched with branched chain amino acids should be consumed.
Drug therapy
Drug therapy is an important part of the treatment of overt P.E. With minimal PE in the absence of its clinical manifestations, pharmacotherapy, as a rule, is not used. At the same time, it can be prescribed to this category of patients in cases of a noticeable impact of minimal PE on the quality of life. To correct HE, various drugs can be used (non-absorbable disaccharides, antibiotics, branched chain amino acids, L-ornithine-L-aspartate) with varying levels of evidence of effectiveness.
Non-absorbable disaccharides.
Lactulose is a synthetic disaccharide that prevents the formation of ammonia. Lactulose is the drug of first choice in the treatment of overt P.E. Lactulose syrup is prescribed 25 ml every 1-2 hours until at least 2 bowel movements with soft or unformed stools occur during the day. Subsequently, the dose of the drug is titrated individually to maintain 2- or 3-fold bowel movements during the day [35]. Taking excessively high doses of lactulose can lead to complications such as aspiration, dehydration, hypernatremia, irritation of the perianal skin, and in some cases even worsen the course of PE [36].
Antibiotics.
Rifaximin is a non-absorbable antibiotic that inhibits ammoniogenic proteolytic bacterial microflora of the intestine [37]. The results of a number of studies have shown the effectiveness of rifaximin in the treatment of P.E. According to AASLD/EASL guidelines [32], rifaximin is an effective addition to lactulose for the prevention of recurrence of overt PE. In comparative studies, 3-6 months of rifaximin therapy improved cognitive function and reduced ammonemia in patients with PE [38]. Rifaximin is prescribed at a dose of 200-400 mg 2-3 times/day (1200 mg/day) for 5-7 (up to 14) days.
Among other antibiotics, neomycin is still used for the treatment of PE; metronidazole can be used for short-term therapy, however, due to side effects, the long-term use of these drugs is limited [39, 40].
Branched chain amino acids.
A number of studies have shown the effectiveness of therapeutic nutrition with the consumption of food enriched with branched chain amino acids [15]. Due to the preferential absorption of these amino acids, the relative content of aromatic amino acids, which serve as precursors of false neurotransmitters, decreases. In addition, branched chain amino acids help increase muscle mass, resulting in increased ammonia detoxification, which partially occurs in skeletal muscle. The AASLD/EASL guidelines only recommend oral administration of branched-chain amino acids as an alternative or adjunctive treatment for patients who have not responded to conventional therapy [41, 42].
L-ornithine-L-aspartate (LOLA).
Since ornithine and aspartate play a major role in the conversion of ammonia to urea, taking LOLA helps reduce the clinical manifestations of PE. Over the past 10 years, several randomized studies have been conducted, the results of which have shown the high efficacy and safety of this drug in the treatment of PE [43]. LOLA is available as a solution for intravenous infusion and as a granule for oral administration. The standard regimen of use involves intravenous drip administration of 20-30 g of the drug for 7-14 days, followed by transition to oral administration of 9-18 g/day. To achieve a faster and more lasting result, a combination of intravenous and oral administration is possible.
Flumazenil
- an antagonist of benzodiazepine receptors, directly affecting the functions of the central nervous system. Flumazenil is used quite rarely, since giving a short-term effect of restoring consciousness, it promotes only a transient improvement in mental state, but does not affect recovery and survival rates [15].
The effectiveness of the therapy is determined by the reverse development of clinical symptoms.
In case of acute liver failure with the development of hepatic coma and cerebral edema, treatment is carried out in the intensive care unit using the same medications as for chronic liver failure, but in higher doses.
Liver transplantation for cirrhosis with recurrent PE, difficult to respond to conservative therapy, can increase the life expectancy of patients. The average 5-year survival rate of patients after transplantation exceeds 72% [15].
The authors declare no conflict of interest.
Urgent Care
Treatment of hepatic coma at home is impossible; qualified medical care is required. The first thing to do to help a person is to call an ambulance. If the patient is conscious, he needs to be provided with peace and immobility; if the psycho-emotional state is severe, he must be reassured.
If upon arrival the ambulance crew assesses the person’s condition as critical, assistance is provided before he is taken to the hospital. It includes:
- oxygen therapy with humidified oxygen;
- administration of isotonic saline solutions to eliminate signs of shock and, if possible, maintain consciousness;
- administration of a fast-acting glucocorticoid intravenously;
- if necessary, the introduction of an antibiotic, its choice is considered on an individual basis.
Emergency assistance can only be provided by a doctor; it is prohibited to try to alleviate the patient’s condition on your own, including by giving painkillers.
How a patient is treated
Most often, doctors have the opportunity to prevent the development of coma in a person who seeks medical help in time. In more rare conditions, patients arrive at the hospital already in a coma.
In any case, hepatic coma is a life-threatening condition. This means that the victim is being treated in the intensive care unit. Self-medication and treatment at home by relatives is unacceptable; all medications must be selected and prescribed only by a doctor.
Since it is easier for someone to prevent than to treat, preventing its development is primarily aimed at treating the underlying liver disease:
- for viral hepatitis - therapy with antiviral agents;
- in case of toadstool poisoning - administration of an antidote (antidote);
- in case of poisoning with other substances, including alcohol, detoxification of the body;
- in the case of autoimmune hepatitis, the administration of hormones is necessary.
Liver cirrhosis is an incurable disease. But you can prevent its progression and (if possible) cure the disease that can lead to it in time.
In addition to measures aimed at eliminating the causes of liver damage, doctors prescribe symptomatic treatment and therapy that reduces the likelihood of complications of liver disease:
- For example, antibiotic therapy helps reduce the formation of toxins in the intestine, and, accordingly, their effect on the nervous system.
- Along with this, laxatives are used to accelerate the removal of bilirubin and toxins from the intestines.
- Medications may be prescribed to eliminate psychomotor agitation. They are usually selected after consultation with a psychiatrist.
- In the diet, doctors usually recommend reducing the proportion of protein (a precursor to the ammonia toxin) and salt.
However, the above measures apply to conditions preceding coma. Treating a patient already in a coma is a difficult and often unsuccessful undertaking, since there is no cure for coma. All measures in such a situation are aimed at maintaining vital functions, and, if possible, reducing the degree of intoxication and brain damage.
Treatment
Treatment is carried out in the intensive care unit after hospitalization. Therapy is prescribed on an individual basis, taking into account the degree of coma and other characteristics of the patient. Typically treatment includes:
- administration of glucocorteroids (if they have already been administered by the ambulance team - after 8 hours);
- the use of antibiotics is often prescribed Ceftriaxone, administered intravenously for greater effectiveness;
- antiviral drugs;
- Arninine or glutamic acid to neutralize the effects of ammonia;
- Dopamine or its analogues against arterial hypertension;
- detoxification therapy for general intoxication.
Previously, blood transfusions were widely used in our country for hepatic coma, but today more and more doctors prefer bloodless methods of therapy, given the risks
In severe cases, doctors immediately recommend emergency liver transplantation. Unfortunately, in our country its implementation is complicated by a lack of donors and documentary issues. Therefore, many people prefer to go to foreign clinics. In case of successful recovery, the doctor gives clinical recommendations, which include following a diet and taking medications for life.
Sometimes hepatorenal coma develops or hepatic coma becomes a complication of renal coma. In such cases, hemodialysis is performed, but the likelihood of death is high.
What is the prognosis and how long do they live after hepatic coma?
How long patients live after hepatic coma depends on the timeliness of treatment and other factors. The survival rate is about 20%; people often die because the disease was diagnosed on time, but it had already progressed, and they never got their turn for a transplant.
Some live for several months, others up to 10 years, doctors explain this by saying that coma is a complication. Much depends on how long the disease that caused the coma lasts, what kind of lifestyle the person led, and what other chronic diseases they have.
Hepatic coma is the final stage of chronic or acute diseases of the organ; its occurrence indicates a person’s inattention to health and neglect of timely treatment. Knowing the pathogenesis, stage, and characteristics of its course, doctors select treatment, but the prognosis for recovery is often unfavorable.