- Classification of non-Hodgkin's lymphomas
- Incidence of non-Hodgkin's lymphomas (NHL)
- Risk factors for non-Hodgkin's lymphoma
- Diagnosis of non-Hodgkin's lymphomas
- Determination of the stage (extent of spread) of non-Hodgkin lymphomas
- Treatment of non-Hodgkin's lymphomas
There are two main types of lymphomas - Hodgkin's disease, named after the author who described this disease, and non-Hodgkin's lymphomas.
Non-Hodgkin's lymphomas (lymphosarcoma) (NHL) develop from lymphoid tissue, which performs a protective function of the body. Lymphoid tissue is represented by lymphocytes and is found in the lymph nodes, spleen, thymus, adenoids, tonsils, bone marrow and gastrointestinal tract.
Lymphocytes include B cells and T cells, from which NHL can develop.
At the same time, B-cell lymphomas are more common (85%) compared to T-cell lymphomas (15%).
Classification of non-Hodgkin's lymphomas
The most commonly used is the European-American classification developed within the World Health Organization (WHO).
According to this classification, NHLs are divided depending on their cellular identity.
Diffuse large B-cell lymphoma accounts for 31% of the total number of lymphomas. This lymphoma occurs most often after age 60 and grows rapidly. At the same time, 40-50% of patients can be completely cured.
Follicular lymphoma , which accounts for 22% of total NHL. This type of lymphoma is usually diagnosed around age 60 and is characterized by slow growth. Long-term (5-year) survival of patients ranges from 60-70%. Over time, follicular lymphoma can develop into a fast-growing diffuse lymphoma.
Chronic lymphocytic leukemia/small cell lymphocytic lymphoma. These related diseases account for 7% of the total number of lymphomas. They are characterized by slow growth, but are difficult to treat. However, patients with these diseases can live for 10 years. Sometimes it is possible to transform them into fast-growing lymphomas.
Mantle cell lymphoma (6%) most often affects men around 63 years of age. Although this type of lymphoma does not grow very quickly, only 20% of patients live for 5 years.
Extranodal marginal zone B-cell lymphomas—MALT lymphomas (8%). The average age of patients is about 60 years. Often found in the stomach, it is characterized by slow local growth. It can be cured well in the early stages.
Nodal marginal zone B-cell lymphoma (2%). Characterized by slow growth. Many patients with early stages of the disease can be completely cured.
Splenic marginal zone B-cell lymphoma occurs in elderly patients, most often males. Often, treatment is not prescribed until severe symptoms appear as a result of an enlarged spleen.
Primary mediastinal B-cell lymphoma (2%) occurs in the mediastinum mainly in women aged 30-40 years and is characterized by rapid growth. 50% of patients can be cured.
Burkitt's lymphoma and Burkitt-like lymphoma (2%) occurs in 90% of cases in men aged about 30 years. Characterized by rapid growth. With intensive chemotherapy, 50% of patients can be completely cured.
Lymphoplasmacytic lymphoma (Waldenström's macroglobulinemia) accounts for 1% of the total number of NHLs. The disease is characterized by a slow progression, but it cannot be completely cured. However, most patients live more than 5 years.
Hairy cell leukemia is a very rare disease and is detected in older people. Characterized by slow growth. Some patients do not need treatment.
Primary central nervous system (CNS) lymphoma can affect both the brain and spinal cord. Previously, this tumor was considered very rare, but now it is detected more often in patients with AIDS. 30% of patients live 5 or more years.
T-lymphoblastic lymphoma/progenitor cell leukemia (2%). This disease can be considered lymphoma or leukemia. The difference depends on the number of tumor cells in the bone marrow. If less than 25% of tumor cells are detected, a diagnosis of lymphoma is made, and more than 25% - leukemia.
75% of patients are men, and the remaining 25% are women. The average age of patients is 25 years. If the bone marrow is not affected, then the probability of cure is high, and if it is involved in the process, the probability of cure does not exceed 20%.
Peripheral T-cell lymphomas (7%) are divided into several types:
Cutaneous T-cell lymphoma (mycosis fungoides, Sezary syndrome) accounts for less than 1% of all lymphomas and is detected at the age of 50-60 years. The 5-year survival rate of patients ranges from 5 to 58%, depending on the rate of tumor growth.
Angioimmunoblastic T-cell lymphoma is characterized by rapid growth and a poor prognosis.
Extranodal T-cell lymphoma of natural killer cells , nasal type, occurs in all age groups. The outcome of the disease depends on the degree of spread of the tumor process.
T-cell lymphoma with enteropathy occurs in people who are sensitive to gluten, a protein in wheat flour. The prognosis (outcome) of the disease is unfavorable.
Subcutaneous T-cell panniculitis-like lymphoma grows slowly at first but can become a fast-growing tumor over time. Chemotherapy is only partially effective.
Anaplastic large cell lymphoma, T/0-cell (2%) occurs more often in young people. Chemotherapy can cure many patients.
Incidence of non-Hodgkin's lymphomas (NHL)
More than 90% of NHL is diagnosed in adult patients. Most often, NHL occurs between the ages of 60 and 70 years. The risk of developing this tumor increases with age.
The lifetime personal risk of developing NHL is approximately 1 in 50.
Since the beginning of the 70s, there has been an almost twofold increase in the incidence of NHL. This phenomenon is difficult to explain. This is mainly associated with infection caused by the human immunodeficiency virus. Part of this increase can be attributed to improved diagnostics.
Since the late 90s, there has been a stabilization in the incidence of NHL.
NHL is more often detected in men compared to women.
In 2002, 5,532 cases of NHL in adult patients were identified in Russia.
In the United States in 2004, according to preliminary data, 53,370 cases of NHL in adults and children are expected.
Risk factors for non-Hodgkin's lymphoma
Risk factors may be genetic (inherited), lifestyle-related, or environmental.
Age is the most important risk factor for NHL. Most cases of NHL are diagnosed in people over 60 years of age.
Congenital defects of the immune system not only predispose to infections, but also increase the risk of developing NHL in children and young adults.
Obesity may increase the risk of NHL.
Radiation increases the risk of leukemia, thyroid cancer, and NHL. Patients who received radiation therapy for cancer later have an increased risk of developing NHL. This risk is further increased when a combination of chemotherapy and radiation is used.
Benzene, herbicides, and insecticides are associated with an increased risk of NHL.
Acquired immunodeficiency caused by the use of various drugs in organ transplant patients increases the risk of developing NHL.
Human immunodeficiency virus infections are associated with an increased risk of some types of NHL.
Epstein-Barr virus is associated with an increased risk of developing Burkitt's lymphoma and other lymphomas, especially in people with AIDS.
The bacterium Helicobacter pylori , which causes stomach ulcers, can also lead to lymphoma of the same location.
Elimination (where possible) of known risk factors can help to prevent this disease to a certain extent.
Prevention of lymphoma
Since the main causes of lymphoma have not been identified, preventive measures regarding this disease are extensive. It is worth undergoing timely examinations with key specialists. In case of infectious diseases, you must carefully follow the recommendations of doctors. If you notice some concerns about your condition, going to the doctor should not be postponed indefinitely. Don't forget about personal hygiene, proper nutrition and exercise. Physical activity and fresh air have never harmed anyone.
Diagnosis of non-Hodgkin's lymphomas
Paying close attention to unusual signs and symptoms may help in early diagnosis of NHL.
NHL can be accompanied by various symptoms depending on the location of the tumor.
Enlarged lymph nodes in the neck, axillary, supraclavicular or groin areas can be easily detected by both the doctor and the patient himself.
If a tumor occurs in the thymus gland or lymph nodes of the chest cavity, compression of the trachea may occur, which leads to coughing, shortness of breath and swelling of the upper half of the body and face.
Damage to the lymph nodes of the abdomen causes an increase in its size due to both tumor nodes and fluid accumulation. Compression of the intestine can cause partial or complete intestinal obstruction, which leads to nausea, vomiting and abdominal pain.
Stomach lymphoma is accompanied by pain in the upper abdomen, nausea, vomiting and loss of appetite.
With NHL of the brain, patients report headache, nausea, vomiting, convulsions, etc.
In the case of skin lymphoma, itching and a subcutaneous thickening of a reddish-purple color appears.
In addition to local symptoms, general symptoms may also occur in the form of unexplained weight loss, fever, severe sweats, especially at night, and severe itching of the skin. These symptoms indicate the presence of a widespread tumor process and worsen the prognosis (outcome) of the disease.
It should be kept in mind that enlarged lymph nodes can also be associated with infection. In this regard, antibiotics are often prescribed. If there is no decrease in the size of the lymph nodes within several weeks, a detailed examination should be carried out: A biopsy (taking a piece of the tumor for examination) is the definitive method for diagnosing lymphoma. In this case, a biopsy can be performed either with a needle or through a minor operation.
A puncture and biopsy of the bone marrow is necessary to determine the presence of tumor cells in it.
A spinal tap makes it possible to detect tumor cells in the cerebrospinal fluid.
In addition, immunohistochemical, cytometric, cytogenetic and molecular genetic studies of the cellular substrate in order to clarify the type of lymphoma, which is important for determining the prognosis of the disease and choosing treatment tactics.
A chest x-ray can reveal enlarged lymph nodes and the thymus gland, as well as fluid in the pleural cavities.
Computed tomography (CT) is especially useful for lymphomas of the head, neck, chest, abdomen, and pelvis, as it allows for detailed examination of the tumor and surrounding organs and tissues.
Magnetic resonance imaging (MRI) is especially useful for examining the brain and spinal cord.
Gallium-67 scanning can detect damage to lymph nodes, internal organs and bones.
A technetium-99 bone scan reveals bone lesions caused by lymphoma.
Ultrasound examination (ultrasound) makes it possible to study in detail the lymph nodes, liver, spleen and kidneys.
Determination of the stage (extent of spread) of non-Hodgkin lymphomas
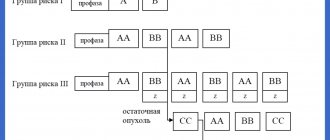
After a detailed examination, including all of the above methods, the stage of lymphoma is specified (from I to IV) depending on the degree of spread of the tumor process.
If the patient has general symptoms, the symbol B (or the Latin letter B) is added to the stage, and if they are absent, the symbol A is added.
To predict the rate of tumor growth and the effectiveness of treatment, an international prognostic index (IPI) has been developed, which takes into account 5 factors, including the patient’s age, stage of the disease, damage not only to the lymph nodes, but also to other organs, the general condition of the patient, and the level of lactate dehydrogenase (LDH) in the serum blood.
Favorable prognostic factors include: age less than 60 years, stages I-II, absence of organ damage, good general condition, normal LDH levels.
Unfavorable prognostic factors include: patient age over 60 years, stages III and IV, damage to lymph nodes and organs, poor general condition and increased LDH levels.
General information
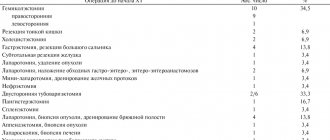
A rare tumor, gastric lymphoma refers to lymphoproliferative processes that develop not in the lymph node, but in the tissues of the stomach. In the group of non-Hodgkin lymphomas, which are very diverse in cellular structure, the proportion of gastric localization is less than 8%.
There are no incidence statistics, but out of 100 thousand adults, gastric lymphoma develops in hardly 5-6 people, mainly in mature and elderly people. It has been noticed that men get sick more often.
Lymphomas are treated by oncohematologists, and the process in the gastrointestinal tract is diagnosed by oncologists, which is explained by the standards for routing a patient with a suspected tumor.
Treatment of non-Hodgkin's lymphomas
The surgical method has limited use in patients with NHL. Typically, the operation involves removing part of the tumor for examination to clarify the diagnosis.
Only in the case of isolated damage to an organ, for example the stomach, is surgical intervention possible. However, even in this case, preference is often given to the radiation method.
In patients with NHL, external irradiation with high-energy sources is usually used. In patients with stages I and II NHL, radiation may be the primary treatment, but a combination of chemotherapy and radiation is most often used.
Radiation therapy can be used as a palliative (temporary relief) method for damage to the brain and spinal cord, as well as to reduce pain in the event of compression of nerve endings.
Radiation therapy may cause minor skin changes and increased fatigue.
Other side effects are related to the location of the radiation.
Thus, radiation therapy to the abdominal area can lead to enteropathy and diarrhea.
Radiation to the chest can cause damage to lung tissue and difficulty breathing.
Irradiation of the lungs, especially in smokers, sometimes leads to the development of cancer of the same location.
Serious side effects of brain radiation take 1 to 2 years to appear and include headaches and memory problems.
It is important to keep in mind that the side effects of chemotherapy may be worsened by radiation.
Chemotherapy refers to the use of anticancer drugs to destroy tumor cells. In this case, many drugs and their combinations are used.
Treatment is carried out in the form of courses at intervals of 2-4 weeks. Chemotherapy can be carried out both in the department and in outpatient (outpatient) settings, depending on the complexity of the treatment, its side effects, the patient’s condition and other factors.
The patient may receive one or more treatment regimens depending on the effectiveness of the therapy.
Antitumor therapy destroys tumor cells, but at the same time damages normal rapidly dividing cells, which include bone marrow, the mucous membrane of the oral cavity and gastrointestinal tract, and hair follicles. The severity of side effects depends on the type, total and total dose of the drug, as well as the duration of chemotherapy.
As a result of treatment, the patient may experience: baldness, the appearance of mouth ulcers, increased susceptibility to infections due to a decrease in the number of white blood cells, bleeding as a result of a decrease in the number of platelets, fatigue due to a decrease in the level of red blood cells, loss of appetite.
These side effects are temporary and disappear after stopping treatment.
Currently, it is possible to prevent and treat complications of chemotherapy by prescribing antiemetic drugs, antibiotics, growth factors that stimulate the production of leukocytes, antiviral and antifungal drugs, etc.
To prevent infectious complications it is necessary:
- avoid contact with infection
- wearing surgical masks by patients, visitors and staff
- use sterile surgical gloves
- wash your hands thoroughly
- do not eat raw vegetables and fruits, as well as foods that may contain germs
- do not contact children, who are more often carriers of infections than adults
Tumor lysis (disintegration) syndrome occurs as a result of the rapid effect of chemotherapy in patients with large lymphomas. The contents of decayed tumor cells enter the bloodstream and impair the function of the kidneys, heart and central nervous system (CNS). This condition can be prevented by prescribing a large volume of fluid and drugs such as soda, allopurinol.
Chemotherapy anticancer drugs can directly damage the kidneys, liver, testicles, ovaries, brain, heart and lungs. However, the use of modern means of prevention and treatment makes it possible to avoid most of these complications.
The most serious complication of chemotherapy is the occurrence of a second malignant disease, in particular leukemia. Fortunately, this complication is rare in patients with lymphoma.
Immunotherapy uses substances that are normally produced by the immune system. These substances can destroy lymphoma cells, slow their growth, or activate the patient's immune system to effectively fight lymphoma.
Interferon is a hormone-like substance that is produced by white blood cells to fight infection. Currently, there are different types of interferon. The use of interferon may cause the lymphoma to stop growing or shrink. The drug is usually used in combination with chemotherapy.
Side effects of interferon treatment include increased fatigue, fever, chills, headache, muscle and joint pain, and mood changes.
Monoclonal antibodies. Antibodies are produced by the immune system to fight infections. Monoclonal antibodies are produced in the laboratory and are used to fight lymphoma cells.
When standard therapy is ineffective in patients with lymphoma, bone marrow or peripheral stem cell transplantation is sometimes used. This allows high doses of chemotherapy to be used to kill resistant tumor cells.
A distinction is made between transplantation of autologous (from the patient himself) and allogeneic (from a donor) bone marrow or peripheral blood cells. Damage to the bone marrow or peripheral blood by lymphoma cells precludes the use of autologous transplantation.
Bone marrow or peripheral stem cells are obtained from the patient or donor before intensive chemotherapy or radiation, and then returned to the patient after treatment to restore blood counts. After 2-3 weeks, the levels of leukocytes begin to increase, and then platelets and red blood cells.
Side effects and complications of bone marrow and peripheral stem cell transplantation are divided into early and late. Early side effects are not fundamentally different from those associated with high-dose chemotherapy.
Complications
Any tumor in the stomach is characterized by complications:
- pain syndrome,
- ulceration with acute or chronic bleeding,
- perforation of the organ wall with the development of peritonitis.
In addition, with lymphoma, there may be a decrease in the specific gamma globulin IgG produced by normal immune cells, which contributes to frequent infections and inflammatory processes. The deficiency is compensated by intravenous administration of immunoglobulin.
In all cases, before starting chemotherapy, prevention of tumor lysis syndrome, which occurs when malignant cells are highly sensitive to drugs, is carried out.