Diffuse large B cell lymphoma (DLBCL) is a group of tumors of the lymphatic system, which is based on the transformation of B lymphocytes into malignant cells.
- Causes and risk groups
- Symptoms of diffuse large cell B lymphoma
- Classification, forms and stages of diffuse lymphoma
- Diagnosis of diffuse large cell lymphoma
- Treatment of diffuse large B-cell lymphoma
- Recovery after treatment for large cell non-Hodgkin lymphoma
- Relapses of large cell lymphoma
- Complications of diffuse large B cell lymphoma
- Prognosis and prevention of large cell lymphoma
Causes and risk groups
The cause of DLBCL is a change in B lymphocytes, i.e., a violation of the DNA structure. Because of this, cells begin to grow and multiply uncontrollably, scattering throughout the body and affecting various organs and systems. Why these mutations occur has not been reliably established. Moreover, there are many people who have characteristic genetic defects but do not have lymphoma. This issue continues to be studied.
Currently, it is customary to talk about risk factors that increase the likelihood of developing this disease:
- Congenital and acquired immunodeficiencies: Wiskott-Aldrich syndrome, Louis-Bart syndrome, AIDS, the need for treatment that reduces immunity: cytostatics, immunosuppressants during organ transplantation, etc.
- Viral infections: HIV, hepatitis C, T-lymphotropic virus.
- Autoimmune diseases: rheumatoid arthritis, lupus, etc.
- Toxic effects of insecticides, herbicides, benzene.
- Treatment through cytostatic and radiation therapy.
Discussion
Based on the data on the increasing incidence of BIA-ALCL, two conclusions can be drawn. The first is that as general awareness increases, so does the number of diagnosed cases. Plastic surgeons and patients themselves have become more wary of any symptoms suspicious for BIA-ALCL. The second conclusion concerns the creation of registers. It is thanks to worldwide and national morbidity registries that it has been possible to combine and process information about patients, causes of BIA-ALCL, prognosis and treatment. Given the rarity of the disease, each diagnosed case is of particular value and should be reported to the scientific community and analyzed.
In France, Singapore, Canada and several other countries, authorities have already suspended licenses for macro-textured breast implants. In the United States, according to a statement by FDA Deputy Commissioner Amy Abernethy, it has been decided for now to limit itself to adding a warning about the risk of BIA-ALCL on the inserts of textured implants. More radical actions will be taken only after receiving complete information about the disease.
Interestingly, there were 4 cases where the diagnosis of BIA-ALCL was made in a patient with a smooth shell implant, but all 4 patients had a history of breast arthroplasty using a textured implant [29]. In the PROFILE study, when analyzing data from 89 patients, the average time from arthroplasty to diagnosis of the disease was 9.0 years [29].
According to recent data demonstrating a possible pathogenetic mechanism of T-cell stimulation during chronic inflammatory processes in genetically predisposed women, experts recommend serious consideration of the 14 points proposed by A. Deva et al. [14]:
1. Use intravenous antibiotic prophylaxis during surgery.
2. Avoid periareolar/transaxillary incisions.
3. Use an aseptic nipple guard to prevent bacteria from entering the pocket.
4. Perform atraumatic dissection to minimize tissue devascularization.
5. Perform careful prospective hemostasis.
6. Avoid dissection of the breast parenchyma.
7. Use a two-plane pocket.
8. Irrigate the pocket with a solution of betadine in combination with an antibiotic.
9. Follow steps to minimize skin contamination.
10. Minimize the time required to open the implant and replace the implant or sizer.
11. Change surgical gloves before implant placement and use new or cleaned instruments and drapes.
12. Avoid the use of postoperative drains, which may be a potential site of bacterial entry.
13. Use multi-layer wound closure.
14. Use postoperative antibiotic prophylaxis.
The twelfth point is controversial because the ingrowth of fibrous tissue into the pores of a textured implant can reduce the likelihood of biofilm formation and bacterial growth, a process that is accelerated by the creation of negative pressure in the periprosthetic pocket. Negative pressure can only be provided by an active drainage system. In addition, it has been demonstrated that blood can increase the formation of endoprosthetic biofilms. This emphasizes the need to eliminate fluid around the implant using a drainage system [28].
Symptoms of diffuse large cell B lymphoma
Large cell lymphoma can manifest itself with many symptoms, but all their diversity can be summarized into three syndromes:
- Enlarged lymph nodes - lymphadenopathy. Most often, lymphoma manifests itself as a painless enlargement of the lymph nodes, which can be detected visually or by palpation. But it happens that nodes that are inaccessible to inspection and palpation are affected (for example, in the chest or abdominal cavity), then this sign may not immediately appear.
- Symptoms of intoxication: fever not associated with infection, heavy sweating, weight loss. The combination of these signs is called B-symptoms. Its presence is important in determining the stage of the disease.
- Symptoms that develop when large cell lymphoma spreads to other organs and systems. This may include chest pain and cough, abdominal pain and bowel dysfunction. When the central nervous system is damaged, headaches, blurred vision and vomiting develop. Due to the destruction of bone marrow, immunity decreases, anemia develops and a tendency to dangerous bleeding.
Diagnosis of the disease
According to the PROFILE registry, based on an analysis of 89 fully documented cases, the most common symptom of BIA-ALCL is periprosthetic seroma - in 73 (85.9%) patients. Capsular contracture occurred in 28 (32.9%) patients, most often grade III or IV. Palpable tumor masses in the mammary gland were detected only in 13 (15.7%) cases. Pain, skin breakdown, and redness were less common but still present. Systemic symptoms included fever, night sweats, weight loss, and non-breast skin lesions. 2 (2%) patients were asymptomatic at the time of diagnosis [29].
In 2/3 of patients with BIA-ALCL, late seroma developed - on average 8-10 years after prosthetics. Therefore, any seroma occurring more than 1 year after prosthetic replacement that cannot be explained by infection or trauma should be considered as a possible sign of disease. In 1/3 of the patients, tumor masses were observed, which indicated a more aggressive clinical course [30].
According to other literature sources [6, 31, 32], 8–24% of patients had a palpable tumor mass, and 4–12% had lymphopathy. Less commonly (<5% of cases), the authors described local and systemic symptoms, including skin rash, fever, and capsular contracture. Most cases of BIA-ALCL were diagnosed during implant revision surgery in the presence of persistent seroma (>1 year), as well as pain, palpable breast masses, swelling or breast asymmetry [33].
B. Adrada et al. [34] reviewed 44 cases of BIA-ALCL using various imaging modalities. They reported sensitivity and specificity for detecting effusions using ultrasound in 84 and 75% of cases, respectively, computed tomography (CT) in 55 and 83%, magnetic resonance imaging (MRI) in 82 and 33%, and positron emission tomography (PET). )/CT in 38 and 83%. Sensitivity and specificity when determining tumor mass using ultrasound (US) is 46 and 100%, CT is 50 and 100%, MRI is 82 and 33%, PET/CT is 64 and 88%. The sensitivity of mammography has been found to be low for visualizing both effusion and tumor masses and is therefore not considered an acceptable imaging modality for diagnosing BIA-ALCL. Based on these data, ultrasound is used as a screening method, while PET/CT is used after diagnosis, for examination before surgery.
The first stage of diagnosis should include ultrasound to collect periprosthetic fluid, fine-needle biopsy of tumor masses and enlarged regional lymph nodes. Involvement of the axillary (93%) lymph nodes is most often followed by enlargement of the internal mammary and supraclavicular lymph nodes, while involvement of non-regional groups of lymph nodes is very rare [35]. Fine needle aspiration is optimal for sampling periprosthetic fluid. During suction, ultrasound can be used to gently move and protect the implant. To diagnose the disease, collect as much fluid as possible (minimum 50 ml). Periprosthetic fluid from BIA-ALCL is typically more viscous than benign seroma due to its higher protein content and cellularity. Fluid samples do not require storage in any specialized media and should be delivered to the laboratory within 48 hours. Although cells can lyse if left for an extended period, diagnostic protein markers in tumor cells are not destroyed, making diagnosis possible from fixed cells blocks years later [6]. The assessment of fine needle aspiration is difficult after a series of previous punctures, since the titer of tumor cells in the puncture may be artificially reduced. The presence of a tumor mass requires a biopsy. Specimens should be sent for morphological cytological examination using cytometry and IHC to quantify the T cells in the specimen and determine CD30 expression. CD30 IHC testing is a fundamental part of diagnostic tests, but is not pathognomonic in itself because CD30 expression is nonspecific. The CD30 antigen can be expressed on benign inflammatory cells. Rare CD30± lymphocytes with normal morphology are considered normal and do not require further investigation [13, 36].
Once a diagnosis of BIA-ALCL has been made, the physician is strongly recommended to conduct a consultation with the individual patient to determine treatment tactics. In patients with aggressive local invasion or lymph node metastasis, a bone marrow biopsy is recommended to exclude the possibility of systemic ALCL. All patients with confirmed BIA-ALCL should undergo preoperative PET/CT scanning, which is optimal for visualizing associated capsular masses, chest wall invasion, regional lymphadenopathy, and/or metastasis to distant organs. The resection strategy and timing of the operation will depend on the data obtained [10].
Classification, forms and stages of diffuse lymphoma
The modern classification of large cell lymphoma is based on clinical data and the extent of the tumor process.
Ann Arbor classification:
- Stage 1. The lesion is limited to one lymphatic zone or one extralymphatic organ or one segment of extralymphatic tissue.
- Stage 2. Two or more areas of lymph nodes on one side of the diaphragm are affected. When extralymphatic organs or tissues are affected, metastases are detected in regional lymph nodes.
- Stage 3. There are single lesions on both sides of the diaphragm.
- Stage 4. There are multiple foci of damage to extralymphatic organs, or limited damage to extralymphatic organs with distant metastases, or damage to the liver and bone marrow.
The Ann Arbor classification is supplemented by the Cotswold modification:
- A - no B-symptoms.
- B - there is at least one of the B-symptoms.
- E - there are localized extranodal lesions.
- S - lymphoma has affected the spleen.
- X - there is massive tumor tissue and internal organs.
Diagnosis of diffuse large cell lymphoma
The diagnosis of non-Hodgkin lymphoma is made on the basis of histological and immunohistochemical examination of tumor tissue. In order to obtain material, an incisional or excisional biopsy of the lymph nodes is performed. In addition, molecular genetic and immunophenotypic studies are performed, which will help determine the type of tumor, the presence of certain genetic changes and select the optimal treatment method.
To determine the stage of lymphoma, the following studies are performed:
- Trephine biopsy of bone marrow.
- Radiation diagnostic methods - ultrasound, CT, PET-CT, MRI.
- A number of laboratory tests are also prescribed - a complete blood count, determination of markers of parenteral hepatitis, HIV testing, biochemical studies, etc.
Treatment of diffuse large B-cell lymphoma
Treatment of diffuse lymphoma is determined based on the following data:
- Risks of relapse according to IPI.
- Patient's age.
- His condition (whether the patient can tolerate high-dose chemotherapy).
The main treatments for large cell lymphoma are chemotherapy and, in some cases, radiation. Before starting therapy for fertile patients, the issue of cryopreservation of gametes (sex cells) is discussed, since treatment can cause infertility.
The main criterion for selecting therapy is the international prognostic index IPI, which includes the following aspects:
- Age. Under 60 years old - 0 points, over - 1 point.
- The patient's condition according to ECOG (patient activity and ability to self-care). 1-2 points on ECOG is 0 on IPI, and 3-4 points on ECOG is 1 point on IPI.
- LDH level. Normal - 0 points on IPI, elevated - 1 point.
- Lymphoma stage. 1-2 - 0 points, 3-4 - 1 point.
- The presence of more than 1 extranodal lesion. No - 0, yes - 1.
The IPI interpretation is as follows:
- 0-1 point - low-risk lymphoma.
- 2 points - intermediate-low risk lymphoma.
- 3 points - intermediate-high risk lymphoma.
- 4-5 points - high-risk lymphoma.
Patients from the low and intermediate-low risk group begin their treatment with 6 cycles of immunochemotherapy according to the R-CHOP-21 protocol. This regimen, in addition to cytostatics, involves the use of the immunotherapeutic drug rituximab. This scheme allows achieving five-year survival in 80% of patients. For patients with stage 3-4 disease, treatment is supplemented with radiation therapy to areas of massive and extranodal tumor lesions.
Treatment of patients from intermediate-high and high risk groups is selected individually, taking into account the patient's age and ECOG status. Young patients in good physical condition are prescribed more aggressive treatment regimens, involving high-dose chemotherapy with hematopoietic stem cell transplantation (HSC). At high risks of damage to the nervous system, several cycles of intrathecal chemotherapy are performed, when drugs are injected into the spinal canal. For elderly and weak patients, more gentle regimens are selected. The effectiveness of treatment is assessed in the middle of chemotherapy cycles and after their completion.
Current state of the problem
In August 2012, the American Society of Plastic Surgeons (ASPS), the Plastic Surgery Foundation (PSF), and the Food and Drug Administration (FDA) signed an agreement on joint research and development aimed at developing an infrastructure in which all BIA-ALCL cases would be centrally collected. The result of this joint work was the Patient Registry and Outcomes For breast Implants and anaplastic large cell Lymphoma etiology and Epidemiology - PROFILE.
In 2021, the National Comprehensive Cancer Network (NCCN) developed guidelines for the diagnosis and treatment of BIA-ALCL [5, 6]. The NCCN guidelines for BIA-ALCL have subsequently been recognized by the FDA as well as national plastic surgery societies.
The incidence of BIA-ALCL has been estimated by various authors to range from 0.1 to 0.3 per 100,000 women with breast implants per year. However, 1 in 500,000 women with textured breast implants are at risk of developing disease 1 year after surgery [7].
Recent studies in Australia and New Zealand have found a sharp increase in the incidence of BIA-ALCL. A total of 56 cases of BIA-ALCL have been confirmed by 2021, with a further 26 new cases diagnosed between January 2021 and April 2021. The incidence was subsequently revised from 1 in 300,000 to 1 in 1000–10,000 women with implants1.
In January 2021, there were 414 reported cases of BIA-ALCL, including 9 deaths2. By February 2021, 518 patients with BIA-ALCL had been reported in 25 countries, including 194 in the United States3. According to data from April 2021, the number of patients worldwide has increased to 570, including 16 deaths4 [8].
As of December 1, 2021, the PROFILE registry included information on more than 250 patients with BIA-ALCL, and ASPS has tracked a total of more than 573 cases, including 33 deaths5 [9].
The latest data on the number of diagnosed cases is currently available on the ASPS website. As of September 3, 2021, 779 patients have been registered worldwide4.
An analysis of the occurrence of BIA-ALCL by G. Brody et al. [10], revealed significant variability in incidence worldwide, with the lowest relative incidence in the eurozone, China and Brazil. Currently, the highest reported incidence is in Australia and New Zealand (1/2832 depending on implant type) [10]. In Scandinavian countries, until recently, there have been virtually no reported cases of BIA-ALCL. Interestingly, according to manufacturers, 70-80% of implants sold in Europe are textured. Therefore, it can be assumed that, as with most tumor diseases, genetic predisposition and ethnicity in BIA-ALCL may play an important role [11].
According to a review of the world literature, the highest incidence is found in countries that have national registries of patients with BIA-ALCL, such as the USA, Australia, France, Italy and the UK. Apparently, this is mainly due to the fact that there is a standardized collection of data on all implants, as well as cases of their removal or replacement. On the other hand, the presence of registers indirectly indicates a high level of awareness of the medical community of these countries about the problem of BIA-ALCL. There may still be no real understanding of the prevalence of BIA-ALCL among women with breast implants.
Following US FDA guidelines, in 2011 implant manufacturers added a warning about the risk of BIA-ALCL to breast implant package inserts. All patients scheduled for breast replacement are required to sign an informed voluntary consent, which has three main goals: 1) informing patients about the existence of this rare disease; 2) explaining to the patient common symptoms, such as the appearance of tumor masses in the mammary glands and the occurrence of periprosthetic effusion; 3) a strong recommendation for patients to urgently consult a doctor if these symptoms appear [12].
Relapses of large cell lymphoma
When treating diffuse large B-cell lymphoma, long-term remission can be achieved in 70-80% of cases, but a number of patients experience relapse. Treatment of relapses is carried out according to the following scheme:
- Second line chemotherapy. It should suppress tumor growth while not harming hematopoietic stem cells.
- GSK collection.
- High-dose chemotherapy. High doses of cytostatics are used, which destroy the most resistant tumor cells, but they also destroy hematopoiesis, so the next stage is carried out to restore it.
- Transplantation of hematopoietic stem cells, which is designed to restore hematopoiesis.
In patients from high-risk groups who have already undergone autologous transplantation and have received a relapse of diffuse lymphoma, allogeneic transplantation is performed, i.e., donor stem cells are used. In these cases there is also a chance of complete remission, but they do not exceed 50%.
Complications of diffuse large B cell lymphoma
Chemotherapy and radiation therapy for diffuse large cell lymphoma have a detrimental effect not only on the malignant tumor, but also on all rapidly dividing cells. These are hematopoietic cells, epithelium of the skin and mucous membranes, etc. Therefore, in the process of treatment and recovery, much attention is paid to the prevention of complications. First of all, it is the fight against infections (bacterial, viral, fungal), disorders of the blood clotting system and the functioning of the digestive tract.
In addition, in the long term there is a risk of developing the following complications:
- The occurrence of other malignant tumors: lung cancer, breast cancer, stomach cancer, as well as leukemia and other types of lymphomas. The greatest risks are observed in the first decades after cessation of treatment.
- Cardiovascular complications: disruption of myocardial function, rapid atherosclerosis of blood vessels, damage to heart valves, etc.
- Lung damage: pulmonitis, pneumosclerosis and pneumofibrosis.
- Complications from the endocrine system: hypothyroidism, infertility, impaired spermatogenesis.
Etiology of the disease
In light of recent research, it is suggested that the risk of BIA-ALCL is most likely directly related to the surface texture of the breast implant and is highest in genetically predisposed women [12]. Textured implants are susceptible to the formation of biofilms on their surface [11], which are communities of bacteria that form at phase interfaces, such as solid/liquid. Biofilm bacteria are remarkable in that they are surrounded by a mucus-polymer matrix of the extracellular substances they produce and are extremely resistant to ultraviolet radiation, dehydration and viruses, antibiotics and immune defense factors. M. Kadin et al. [13] hypothesized that BIA-ALCL is associated with chronic bacterial stimulation of Th1/Th17 antigen-driven memory T cells in periprosthetic capsule tissues and the resulting sustained proliferation of T cells with subsequent genetic events in the pathogenesis of BIA-ALCL [14] . H. Hu et al. [15] compared implant capsules from patients with BIA-ALCL and capsular contracture, finding a higher bacterial load and significantly different microbiome in BIA-ALCL samples. The authors identified a large number of bacteria Ralstonia pickettii
(a common gram-negative contaminant in drinking water), which may play an important role in the etiology of the disease, which remains to be determined.
Initial insight into the pathogenesis and molecular drivers of BIA-ALCL was gained through flow immunohistochemical (IHC) cytometry and functional experiments in characterizing the immunophenotypes of cell lines derived from patient tumors. BIA-ALCL cells showed positive staining for CD30 (a cell membrane protein), which, in the presence of anaplastic cytomorphology and corresponding clinical presentation, should be considered a hallmark of BIA-ALCL [16, 17]. Normally, the pool of CD30+ T cells ranges from 0.1 to 5% of all circulating T cells, and during inflammatory conditions in the body their concentration can increase significantly. Increased expression of CD30 can be induced on both T cells and B cells as a result of viral infection. It has been described that CD30± lymphocytes are able to temporarily increase from a background level of 0.1 to 95% [18]. Other T cell antigens expressed on malignant cells are CD3, CD4/8, CD5 and CD7 [19]. In most cases, BIA-ALCL tumor cells stain positive for multiple myeloma 1 (MUM1) (interferon regulatory factor 4) during IHC examination [20]. Genomic characterization of BIA-ALCL shows similar molecular abnormalities to ALK-negative systemic anaplastic large cell lymphoma (sALCL), including JAK/STAT activation and MYC/TP53 dysregulation, but clinically the disease is much less aggressive [20]. Other studies have also noted the occurrence of BIA-ALCL in women with acquired germline JAK/STAT mutations [21] and, in addition, the association of the disease with Li-Fraumeni syndrome, which occurs in the presence of a mutation in the p53 oncogene [22, 23]. In such cases, breast reconstruction using textured breast implants in women after mastectomy for breast cancer is completely inappropriate.
Prognosis and prevention of large cell lymphoma
The prognosis for diffuse large B cell lymphoma depends on the IPI score. The higher the score, the worse the prognosis. For patients with a score of 4-5 (high risk), the five-year survival rate ranges from 31%. At low risks, the five-year survival rate is about 91%.
As for specific prevention, it does not exist today, and all recommendations for minimizing the risk of the disease boil down to maintaining a healthy lifestyle and proper nutrition.
Book a consultation 24 hours a day
+7+7+78
Impact of implant texture on disease risk
The surface texture of the implant varies depending on the manufacturer and can usually be classified as macrotextured - polyurethane and Biocell (Allergan plc, Ireland), intermediate textured (TRUE Texture; Sientra, USA) or microtextured (Siltex, Mentor Worldwide”, USA) [24, 25]. Aggressive macrotextured implants (polyurethane and Biocell) demonstrate higher numbers of periprosthetic bacteria than microtextured ones (Siltex and Poly Implant Prothèse) and, as a result, a higher T-cell response [15]. This makes sense given that more aggressive texturing provides space for bacterial growth [26].
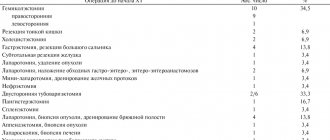
According to some researchers, the risk of developing BIA-ALCL is approximately 16.5 times higher for Biocell and 23.4 times higher for polyurethane implants (Silimed, Brazil) compared to Siltex texture, if taken as one ( table 1)
Table 1. Characteristics of breast implants [27].
Macrotextured (or high surface area) Biocell implants (Allergan, Inc., USA) are produced using “salt loss technology,” in which the implant shell is pressed against a layer of salt. In contrast, Siltex microtextured (or low surface area textured) implants (Mentor Worldwide, USA) are manufactured by reverse negative imprinting with textured foam, resulting in a less aggressive form of texturing [28].
in 2021, it completely recalled the Biocell line of macrotextured implants from the market. However, it is too early to draw definitive conclusions about the role of a specific type of implant in the incidence of BIA-ALCL.