Warts are skin growths in the form of nodules or papillae. This is the most common skin pathology, occurring in more than 90% of the world's population. Warts can appear in any person, at any age, on absolutely all areas of the skin, from the face to the feet. The disease is often contagious, it all depends on the person’s immune system.
COST OF TREATING WARTS IN OUR CLINIC IN ST. PETERSBURG
| Wart removal price | from 500 rub. |
| Dermatologist appointment | 1000 rub. |
| Dermatoscopy | 500 rub. |
| Call free: 8-800-707-1560 *The clinic is licensed to provide these services | |
What causes warts
The content of the article
There is a common belief that touching a frog causes warts to appear. It's a delusion. The causative agent of the disease, which results in the formation of warts, is human papillomavirus infection. According to statistics, this infection causes about 20% of all cancers.
The risk of HPV infection increases significantly:
- when using other people's personal hygiene items and items of common use;
- in public places (swimming pool, bathhouse, etc.), especially when walking there barefoot;
- in case of skin damage;
- with increased sweating of the hands and feet;
- upon contact with an infected person (handshake, sexual contact, etc.);
- when walking in tight, uncomfortable shoes that cause friction on the skin of the foot;
- when using non-sterile instruments (in a beauty salon, etc.).
The infection can remain in the human body for 3 to 6 months without showing itself in any way. Its “activator” and indirect culprit for the appearance of warts is weakened immunity.
What is the best way to treat?
Warts can be removed in almost any way. The surgical method, electrocoagulation, laser and cryodestruction, as well as radio wave surgery are used.
Radio wave surgery
, in my opinion, is a more effective method that allows you to remove wart tissue under visual control. When using this method, the tissue is not burned, but is excised along with a small piece of healthy skin. Thus, the likelihood of warts reappearing becomes minimal.
See all photos before and after removal
Histological examination during removal is mandatory if there is the slightest doubt.
Are warts always dangerous?
Most warts are completely harmless and can theoretically disappear in a few weeks or at most a month. In this case, patients are more likely to be concerned about a serious cosmetic defect, which causes psychological discomfort and interferes with leading a full lifestyle.
Warts are often painless unless they are on the soles of the feet or another part of the body that is subject to shock or constant contact. But there are cases of itching and discomfort in the affected area.
But as mentioned above, warts are viral in nature, so you cannot expect that the neoplasm will go away on its own or will not bother you for the rest of your life. Any wart should be shown to a dermatologist, and if he deems it necessary, it should be removed using one of the safe methods.
My bad experience of getting rid of a wart on my finger
I was no exception and was attacked by this wart virus. I am one of the “lucky” ones who carry and constantly fight this virus. I can't say that I suffer much from this. I remember as a child you always came across a friend or acquaintance who constantly and even had warts in large numbers. In my case, the wart could have appeared somewhere on a finger or toe. After cauterization, she left and did not manifest herself for quite a long time. But I always knew that it could grow again somewhere and again I would have to look for a way to get rid of a wart on a finger or somewhere else. This time, too, I wasn’t particularly surprised when I noticed a small painful lump on my finger. But everything turned out to be more complicated. The location turned out to be very unfortunate.
A wart appeared on the fingertip of my right hand (and I’m right-handed). Very soon I realized that the case was more serious than it seemed. We have a huge number of nerve endings at our fingertips. The wart gradually tore the tissue, which caused pain and the inability to do anything at all. Under heavy loads, not to mention punches (if you also do any martial arts, you will understand), I had to feel quite unpleasant sensations or exclude my poor finger from the process.
After enduring a little and waiting for the wart to break through the skin and appear, I, without hesitation, anointed it with Verukkatsid. I once used Feresol, but it disappeared from sale. He helped me well.
And after a while big troubles began. The finger began to swell, and pus began to appear under the skin around the wart. The finger began to hurt so much that it was completely unable to participate in the processes of grasping, pressing, striking, etc. It was difficult to understand what caused such a reaction and pain. This is a place where everything comes together: damage to tissues and nerve endings, constant injury to this part of the body that is active in life, exposure to chemical acid from a wart remedy. After all, it is this finger that presses the right button of the computer mouse. So horror, horror!
On top of everything else, the wart began to bleed and my finger became swollen. Realizing that I needed to do something faster, I went to the doctor. At a nearby medical center there was a dermatovenerologist and cosmetologist rolled into one. I ended up with him.
How to recognize warts: symptoms and signs
An inexperienced person may confuse warts with other skin growths, for example, moles, calluses, melanomas.
The main differences between warts and moles:
- moles have a dark or black tint, while warts have a light color;
- warts grow tightly together with the skin, moles are separate structures, as if glued to the body;
- moles are soft and smooth to the touch, warts are hard, hard and rough.
It is also easy to distinguish a wart from a callus. When pressing on the growth, painful sensations will occur, and if it peels off, traces of hemorrhages will be visible underneath it. Under the callus is new, tender skin.
You can distinguish a wart from a melanoma by color and shape. This dangerous disease is characterized by heterogeneous red and black shades, proliferation and an uneven contour.
It is not difficult for a dermatologist to make the correct diagnosis using a visual examination. But a good specialist will not be content with just a simple inspection. He will definitely use a special magnifying device - a dermatoscope. If there is a suspicion of a pathogenic process, scraping of the surface layer will be required.
In the case of anogenital warts (located around the anus and on the genitals), consultation with a gynecologist or proctologist is necessary.
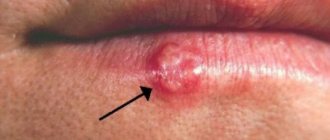
Common (simple, vulgar) warts
Common warts are dense, dry growths characterized by an uneven and rough surface to the touch, variable size and rounded shape. They look like a hard, keratinized bubble up to 1 cm in diameter, significantly rising above the surface of the skin.
The surface of common warts is often covered with grooves and projections, which is why the new growth vaguely resembles a cauliflower or raspberry with black dots inside.
This is the most common type of wart, accounting for up to 70% of all such skin neoplasms. Simple warts can appear on the skin at any age, but most often they affect children and young people. This is due to the fact that they have weaker immunity than adults.
Common warts usually appear on the hands (fingers and backs of the hands), knees and elbows, sometimes on the face or feet, and extremely rarely on the mucous membrane of the mouth.
A scattering of small growths may form next to the large “parent” wart. Young neoplasms usually remain flesh-colored; over time, they acquire a dirty gray or grayish-brown tint, less often yellow or pinkish. This is due to their uneven porous surface, which accumulates dirt.
Vulgar warts usually do not cause concern: they do not cause unpleasant symptoms, do not hurt or itch. However, they may cause pain if they are in areas subject to impacts or in contact with clothing. The growths may heal on their own over time, especially if they occur in childhood.
Causes of warts
Viral warts are most common on the face.
The main reason for their formation is the papillomavirus.
It enters the skin and causes excessive cell division.
As a result, small benign tumors form.
This virus is transmitted by contact.
For infection, an important condition is the presence of damaged epidermis.
Therefore, warts and papillomas on the face appear more often in men.
After all, they regularly shave their beard hair.
The blade causes microdamage to the skin.
Through these defects, a virus enters it, causing warts to grow on the face.
They look unattractive.
In addition, they can be damaged during shaving.
Other types of warts on the face are less common.
There are hereditary diseases that cause their multiple occurrence.
Also, a number of pathologies lead to the formation of a rash that looks like warts.
Plantar (spike) warts
Plantar warts are a type of vulgar wart. The manifestation of the disease is most often observed in children and at the age of 20-30 years. Of all skin warts, plantar warts occur in 30%.
Warts on the soles appear as hard, round lumps with papillae in the middle. Inside the wart, characteristic black dots are visible - many small thrombosed capillaries. Along the edges there is a small roll of keratinized skin. The visible part, rising above the surface of the skin by only 1-2 mm, can reach 2 cm in diameter and is only a quarter of the total size of the plantar wart, which mainly forms in the deep layers of the epithelium (skin).
Externally, the spine resembles a callus. A plantar wart can be differentiated (distinguished) from a callus by the visible interruption of the skin pattern in accordance with the wart.
This type of neoplasm usually affects the feet (sole, sides and toes), and less commonly the palms. They appear on the skin as small whitish, pinpoint skin lesions, sometimes itchy. Over time, their surface becomes rougher and changes color - from yellow to dark brown.
Plantar warts themselves do not pose a threat to health, but when walking they cause a person significant discomfort, cause pain, which often intensifies, and can even bleed. This is due to the location of the tumor and the specifics of its growth. Since the spine grows inward, the weight of the body when walking compresses the pain receptors.
The incubation period of the disease ranges from several days to several years. The infection enters the body and goes into waiting mode for a favorable environment to activate. Plantar warts regress without treatment in 50% of cases. But this process lasts from 8 months to one and a half years.
Without treatment, plantar warts will enlarge and multiply, even to the point of producing large clusters of tumors. This can even lead to temporary loss of a person's ability to work due to unbearable pain that prevents walking.
Based on the characteristics of the lesion and its location, plantar warts are divided into 3 types:
- simple;
- periungual;
- mosaic.
Bibliography:
1) Cockayne S, Hewitt C, Hicks K, Jayakody S, Kang'ombe AR, Stamuli E, Turner G, Thomas K, Curran M, Denby G, Hashmi F, McIntosh C, McLarnon N, Torgerson D, Watt I; EVerT Team. Cryotherapy versus salicylic acid for the treatment of plantar warts (verrucae): a randomized controlled trial. BMJ. 2011 Jun 7; 342:d3271. doi: 10.1136/bmj.d3271.
2) Dall'oglio F, D'Amico V, Nasca MR, Micali G. Treatment of cutaneous warts: an evidence-based review. Am J Clin Dermatol. 2012 Apr 1; 13(2): 73-96. doi: 10.2165/11594610-000000000-00000.
3) Nguyen NV, Burkhart CG. Cryosurgical treatment of warts: dimethyl ether and propane versus liquid nitrogen – case report and review of the literature. J Drugs Dermatol. Oct 2011; 10(10): 1174-6.
4) Ahn CS, Huang WW. Imiquimod in the treatment of cutaneous warts: an evidence-based review. Am J Clin Dermatol. 2014 Oct; 15(5): 387-99. doi:10.1007/s40257-014-0093-5.
Periungual plantar warts
Periungual warts are small, rough formations with cracks on the surface, located on the hands and feet of a person, namely near the nail plate or deep under it. Externally they resemble cauliflower heads.
They can be flat, pointed or hemispherical. As a rule, periungual warts are gray, but they can also be flesh-colored. They are not too dense, like simple plantar ones, but have a fairly deep root.
This disease mainly affects children and young people. The main factor in contracting the infection is skin microtraumas around the nail. At particular risk are those who bite their nails and pet stray animals, as well as people who carelessly remove cuticles, use undisinfected tools, and work in water without gloves.
This type of neoplasm does not pose a threat to human health; it is mainly only a cosmetic defect. Periungual plantar warts do not cause discomfort or pain when pressed. However, a wart under the nail is not so harmless - over time, the neoplasm provokes depletion of the nail plate and its further destruction.
In addition, various bacteria and viruses enter through cracks on the surface of the growths, which easily form due to frequent hand work, causing re-infection. Also, as warts grow, the cracks can cause pain. The cuticle is often lost and a tendency to become inflamed (paronychia) develops.
Removal of the tumor is necessary to stop the proliferation of growths, which easily spread to healthy fingers. Localization of the wart under the nail plate makes treatment and removal very difficult. When it appears in childhood or adolescence, it can go away on its own.
Mosaic plantar warts
Mosaic warts are a special type of neoplasm. They are plaques, so-called clusters, formed as a result of the fusion of many small plantar warts tightly pressed together. The arrangement of the plaques resembles a mosaic (hence their name).
This formation is usually observed in a small and localized area. It can reach a diameter of about 6-7 cm. In the early stages of development, mosaic warts look like small black punctures. As they develop, they take on the appearance of a white, yellowish or light brown cauliflower, with dark spots in the middle. These spots are formed due to thrombosis of blood vessels.
This type of wart is quite rare. They usually affect the hands or soles of the feet, and are especially common under the toes. Unlike simple plantar warts, mosaic warts cause little or no pain when walking because they are flatter and more superficial.
Mosaic warts are highly contagious. They are difficult to treat due to the multiplicity of foci of viral infection. The success of treatment is facilitated by its timely initiation. As a rule, mosaic growths are prone to recurrence even after surgical removal.
Flat (juvenile) warts
Flat warts are a fairly common type of tumor and the least problematic. They present as small lenticular lesions (several mm in diameter) or smooth papular lesions. They can grow either singly, which is quite rare, or in large numbers, close to each other.
There are several stages of the disease:
- mild – one or several painless warts;
- medium – from 10 to 100 painless growths;
- severe – more than 100 neoplasms.
If they are localized in places that experience excess pressure (friction from clothing, shoes, etc.), they cause pain.
Flat warts are easily identified and have a white, brown, yellowish or pink hue, similar to the color of meat. They are about the size of a pinhead and, compared to other types of warts, are smoother and flatter. In fact, at the point where a flat wart develops, the skin rises slightly (to a height of about 5mm), forming a sort of raised circular area.
The growths typically appear on the face, knees, elbows, back, legs, and arms (especially the fingers). People of absolutely any age become victims of this disease. But most often it affects children and adolescents (20% of schoolchildren have it), hence the second name for warts - juvenile.
In a close group of schoolchildren, 80% show resistance (resistance) to the virus. In adults, irritation and inflammation after shaving contribute to the proliferation of tumors.
The incubation period of infection can last up to 8 months. Mostly the disease is only a cosmetic defect. Juvenile warts are painless unless caused by mechanical pressure or injury and can sometimes cause itching, but are extremely contagious.
The virus is practically not transmitted through shared objects; the main route of infection is skin contact. Flat warts multiply so easily that it is enough to touch a healthy part of the body to cause the birth of a new formation.
The peculiarity of this type of wart is that in most cases no treatment is required: they can disappear as suddenly as they appeared, especially in children. In adults, the disease must be treated, and the virus is very resistant to drug treatment.
General information
Warts are hypertrophied areas of the epithelium, usually resulting from infection with papillomavirus.
They are benign formations on the skin or mucous membrane. They appear more often in children and adolescents who have a weak immune system. Warts can be single or multiple, oval or round, lighter or darker than the surrounding tissue. If left untreated, they can increase in size and cause discomfort.
Neoplasms are localized in different parts of the body:
- face;
- fingers, especially around nails;
- articular surfaces (knees, elbows);
- soles.
Sometimes found on the mucous membrane of the larynx and nose. Such warts often degenerate into cancerous tumors, and therefore require immediate medical attention.
Anogenital warts (condylomas)
Among sexually transmitted diseases, anogenital warts are especially common. They are flat and elongated neoplasms or elastic elastic growths in the form of cauliflower or cockscomb. Such warts reach 1-1.5 cm and are gray, pink or flesh-colored.
Typically, this type of neoplasm is transmitted sexually: during vaginal/anal sex or even simply through contact with intimate areas without penetration. After oral sex, warts can appear on the mucous membranes of the mouth, throat, vocal cords or trachea. Such growths are called oral, or acute, condylomas. In rare cases, infection occurs through household contact or from mother to newborn.
Based on their appearance and structure, there are several types of genital warts:
- Pointed - loose polyps of pink, flesh-colored or red color, on a stalk or a wide base, reminiscent of cauliflower. They can occur either individually or in the form of multiple clusters. Genital warts are prone to rapid reproduction;
- Papillary - round, smooth growths without a stalk, rising above the surface of the skin by several millimeters;
- Keratotic - very dense, thickened formations that protrude significantly above the skin. Typically affects the female labia majora;
- Giant (Buschke-Levenshtein condylomas) are a rare type of wart. They are prone to rapid growth, accompanied by destruction of surrounding tissues. In extremely rare cases, giant condyloma degenerates into a malignant form;
- Flat - formed both singly and in the form of multiple clusters. There are practically no symptoms, sometimes itching and discharge may occur. The affected area of flat growths is the vaginal mucosa and cervix in women.
The appearance of anogenital warts and the deterioration of their condition are often accompanied by other sexually transmitted diseases (ureaplasmosis, trichomoniasis, chlamydia, etc.). It is impossible to protect yourself or your partner from infection using a condom, since in this case it is ineffective. It is necessary to completely abandon intimate relationships until complete recovery.
Anogenital warts occur equally often in people of both sexes who are sexually active (usually from 20 to 25 years). The incubation period for this disease varies from three weeks to nine months, with an average of about three months.
In men, condylomas are most often found on the foreskin, scrotum, inside the urethra and on the penis. They can be localized around the anus and rectum, especially in homosexual men. In women, warts appear mainly at the level of the vulva, vaginal wall, cervix and perineum; The urethra and anal area may also be affected.
Genital warts are more common in immunocompromised patients. The rate of growth varies, but pregnancy, immunosuppression (suppression of the immune system), discharge from the urethra, vagina or rectum, accumulation of smegma, or skin maceration (the natural process of swelling of the epidermis (layer of skin) with prolonged contact with liquid) can accelerate the growth and spread of warts.
Characteristic symptoms of the disease:
- severe itching at the location of the growth;
- painful and uncomfortable sensations;
- burning;
- pain during and after sexual intercourse;
- foreign body sensation;
- problems with defecation when the wart is located in the anus;
- bleeding when condyloma is damaged.
In most cases, anogenital warts are benign, but they can degenerate into carcinoma. For this reason, in order to prevent cancer, condylomas, regardless of their position, shape and size, are always removed.
Anogenital warts are usually diagnosed clinically. Their morphology distinguishes them from typical lateral condylomas of secondary syphilis, but in any case, serological tests for syphilis are necessary in the initial phase and after 3 months. A biopsy is required to rule out carcinoma and is mandatory in cases of bleeding, ulceration or persistent warts.
Endocervical and anal warts can only be visualized by colposcopy and anoscopy. Application of a solution of 3-5% acetic acid for a few minutes before colposcopic examination causes the growth to change color to white, improving visualization and detection of small warts.
Recurrence of anogenital warts is promoted by:
- promiscuity;
- lack of personal hygiene;
- installation of an intrauterine device, termination of pregnancy using surgical traumatic methods or other medical procedures.
This type of wart is dangerous due to a number of complications:
- Lack of careful intimate hygiene or irritation of growths due to constant friction against underwear leads to ulceration of growths by secretion of purulent discharge with an unpleasant odor;
- In the absence of timely treatment, genital warts are prone to suppuration;
- Lack of therapy leads to the formation of a large number of warts. In particularly advanced cases, not even a small area of healthy skin remains;
- In the presence of anogenital warts, a strong decrease in immunity is observed, which is associated with a person’s susceptibility to any infectious disease. If the patient already has a chronic inflammatory disease (in particular, of the pelvic organs), it will necessarily get worse;
- Threat of degeneration into a malignant form.
Filiform (acrochord) warts
Filiform warts, also known as facial warts, are the most unusual type of these growths. They are thin, long, racem-like shoots that are usually found on the eyelids and surrounding areas, on the neck, near the lips and nose, and less commonly on the legs, in the groin folds, under the mammary glands and in the armpits.
The typical color of acrochords is flesh-colored, which is why people do not immediately notice them. Sometimes they may turn yellow, brown or pink. Usually they reach a length of 5 to 10 mm, extremely rarely - several centimeters. Depending on the severity of the virus, acrochords form singly or in multiple clusters. This distinctive type of filamentous wart is usually diagnosed visually.
Filiform warts form when a strain of the human papillomavirus causes the top layer of skin to grow too quickly. At the inception stage, the growth looks like a yellowish bump. As it grows, it stretches out, transforming into an elongated formation on a stalk. To the touch, the wart has an elastic and dense structure.
People of absolutely any age can become a “target”, but often elderly patients suffer from this disease. According to statistics, about 50% of the world's population over 50 years of age have facial warts.
Infection with the virus often occurs through cracks and abrasions on the face, so people with dry skin are at high risk. Also, the appearance, growth and spread of facial warts is facilitated by various hormonal changes (pregnancy, obesity, menopause, ovarian dysfunction, diabetes, etc.).
Although highly contagious (infectious) and unattractive in appearance, this type of wart is benign, painless, and often responds well to treatment.
When they appear in sensitive areas, such as skin folds, or areas often subject to pressure and injury, some symptoms may occur:
- itching;
- bleeding;
- soreness;
- irritation.
This type of wart almost never develops into a malignant form. However, if the acrochord is injured, there is a high risk of developing an inflammatory process. Unlike many other similar neoplasms, the filamentous type does not disappear on its own. When a wart falls off, a new one grows in its place. Sometimes there is keratinization of the growth and its transformation into a cutaneous horn.
Facial papillomas are contagious and can be spread by sharing towels or facial cosmetics. Touching the acrochords puts a person at risk of spreading them to other parts of the body. Warts will increase in size and number if they are not removed.
Their location and ugly appearance make facial growths a cause of emotional stress and embarrassment for many people, sometimes affecting their self-esteem and self-confidence.
Who to contact if you have warts and other cosmetic diseases
Let’s take a brief look at the specialists who deal with skin problems and diseases. There are just dermatologists, just venereologists, just cosmetologists. In any case, the doctor must be competent in determining and correctly making a diagnosis. If something is not within his competence, then send it to another specialist closer to the problem. It is necessary not only to diagnose and eliminate the problem, but also to prescribe treatment for the cause of the disease.
A dermatovenerologist is a doctor who combines knowledge of dermatology and venereology and is able to recognize and prescribe treatment for both dermatological and venereological diseases: viral infections and diseases, genitourinary infections.
A dermatologist is a doctor specializing in skin diseases: neoplasms, allergic reactions, psoriasis, warts, etc.
A cosmetologist is a doctor who deals with cosmetic and aesthetic problems of the skin, hair, and nails. This specialist cannot prescribe treatment and prescribe medications, perform anesthetic procedures and generally penetrate beyond the skin.
A doctor of medical cosmetology , unlike a simple cosmetologist, already has an education in the field of dermatology and is able to eliminate skin problems that have arisen and prescribe treatment.
I think that we have figured out the definitions of specialists. Now you know who you can go to to get rid of a wart on your finger or toe, and who you shouldn’t go to.
After the examination, it was decided to immediately begin removing the wart. Using ultrasound, the doctor removed the wart for more than half an hour. As it turned out, it was necessary to remove not only the wart, but also its already deep roots. The matter was complicated by the presence of inflamed tissues and pus that were already infected and changed under the influence of acid.
Strange affair. I underwent three surgeries on the knee joint, a bunch of injections in the knee, and even once had a post-operative stitch on my knee stitched up. But with a finger it was scary. I repeat, there are a lot of nerve endings there. The finger may feel unpleasantly sore for 24 hours even after taking blood.
In my case, the most painful and unpleasant thing was the injections of ice (ice caine) into the sore finger. To my question, is there anything to spray for freezing, like football players, the answer was that it is used only superficially or on the mucous membranes. In my case, only deep injections. But even in this case there were painful sensations, and I had to endure it here too. Who would have thought that some kind of wart could cause so many problems!
I am writing this article with a bandaged and already operated finger. It still hurts to click the mouse, but I feel that the pain is no longer the same. Now at the site of the wart, a large open wound is sufficient. I don’t attach a photo: sometimes Google swears at shocking content in my articles.
Why am I writing all this? Of course, to suggest what and how can or cannot be done in such a situation. If you have read up to this point, then something similar has probably happened to you, and not for the sake of “reading something interesting.” If everything is fine, then thank you for your attention.
Now let's begin to explain the important points and process of treatment, medication use and recovery.
Senile (age-related keratomas, seborrheic keratoses) warts
Senile warts are one of the most common skin lesions that appear in old age as a general sign of skin aging. Despite their name, they are not caused by the human papillomavirus.
Seborrheic keratoses are extremely common. According to statistics, more than 90% of the population over the age of 60 have one or more of them. They are equally common in both men and women. It is not uncommon for the disease to affect people aged 30-40 years, as well as young people under 20 years of age.
Keratomas and keratoses can appear on any part of the body, including the scalp, face and genitals. The exception is the palms, soles of the feet and mucous membranes. It is rare for a person to develop only one growth. Over time, age-related keratomas become more and more numerous. Many people inherit a tendency to develop a very large number of these tumors. Some of them may have hundreds of wart-like growths scattered throughout their body.
In the early stages, aging warts appear as slightly raised light brown spots or papules. They can remain very flat and resemble freckles in appearance, or they can gradually thicken and develop a rough, warty surface, like a tumor on the skin. In most cases, they darken slowly and may eventually turn black.
These color changes are harmless. Many senile warts remain pinkish in color. Typical of these are small keratin plugs that can be seen on the surface of the wart.
Keratoses are usually round or oval in shape. Some seborrheic warts are irregular in shape. Their size can vary from one to several centimeters in diameter.
The cause of age-related keratomas is unknown. They are generally considered to be degenerative in nature and appear in large numbers as the skin ages. It is assumed that ultraviolet radiation increases the likelihood of their development.
There are five traditional forms of age-related warts:
- Spotted, or popularly “death freckles” . They form in numerous clusters on the hands and face. Such growths are round with an uneven contour and a smooth or slightly rough surface. It has several color options: light brown, brown-brown or pinkish-yellow;
- Papular or nodular . Larger growths tend to grow. Their typical color is gray or yellow. The surface of the wart is covered with horny layers;
- Classic keratoma . It is a collection of plaques tightly connected to each other. It is characterized by a jagged outline and a copper or pinkish color. As it grows, the middle part of the wart sinks;
- Cutaneous horn. It is a modification of keratoma. It is expressed as a cluster of dense keratinized dark brown plaques up to 1.5 cm.
Adverse reactions to certain medications and many chemotherapy drugs can contribute to the formation of irritated seborrheic keratoses—inflamed, red, crusty lesions. This leads to the development of eczematous dermatitis around the growth. Dermatitis can also cause new seborrheic keratoses to appear.
Age-related keratomas are always benign. This means that they do not spread and do not degenerate into a malignant form. The main problem is a cosmetic defect, especially if they develop on the face.
There are rare cases of skin cancer called melanoma that develops in a seborrheic wart. It is unknown whether this is just a coincidence or represents a true change in the cells in a seborrheic wart. A large number of age-related keratomas may be a sign of cancer of internal organs.
Typically, seborrheic keratoses are treated for cosmetic reasons or because they become itchy and irritating. If the growths, especially large and warty ones, are injured (rubbed against clothing, touched by something), they may bleed or become inflamed.
Diagnosis of the disease is usually made through a clinical examination. This type of wart is difficult to distinguish from skin cancer without histological examination. Therefore, very dark lesions that have changed in some way or that are growing rapidly require a biopsy to confirm the diagnosis and rule out the possibility of cancer. Darker lesions should also be checked by a doctor to make sure they are not melanoma.
Flat warts: features and treatment options
In their clinical practice, doctors of various specialties often encounter human papillomavirus (HPV) - associated diseases of the skin and mucous membranes. The sharp increase in the infection rate of the population, the diversity of clinical pictures, and the characteristics of the course of these conditions arouse interest and active discussion about the tactics of managing such patients among a large number of clinicians. The relevance of the problem of HPV infection, along with the negative trend of spread, is associated with a significantly pronounced negative effect of the virus on the immune system, which leads to its long-term persistence, reluctance to therapy and frequent recurrence of the disease.
Papillomaviruses were allocated to a separate family Papovaviridae, which, according to modern concepts, consists of 16 genera, representatives of five of which are pathogenic for humans [1, 2]. Virions do not have an envelope; their diameter is 50–55 mm. The capsid has the shape of an icosahedron and consists of 72 capsomeres. The genome is represented by double-stranded circularly twisted DNA and includes about 8000 base pairs [3]. During the replication cycle, the viral genome expresses 8 to 10 protein products. Early proteins that control viral replication, transcription and cellular transformation are represented by oncoproteins E6 and E7. The E1 and E2 proteins regulate viral DNA replication and gene expression. Late proteins L1 and L2 are structural proteins of the virion. Protein L1 forms capsomeres [4]. Invasion of the virus occurs through microdamage to the skin and mucous membranes with infection of predominantly immature, dividing cells of the basal layer, followed by replication of the virus and assembly of viral particles in the differentiated cells of the surface layer of the epidermis/epithelium. The entire development cycle of the infectious process is closely associated with the division of cells of the integumentary epithelium of the skin and mucous membranes and is not accompanied by signs of inflammation. In this case, HPV can have a productive or transformative effect on the epithelium. With productive exposure, benign neoplasms arise - papillomas, warts and condylomas of the skin and mucous membranes. The result of the transformative effect is dysplasia of varying severity, the progressive development of which leads to cancer [5].
Currently, more than 100 types of HPV have been identified that can infect the skin and mucous membranes and provoke the development of changes characterized by papillomatous growths. The human papillomavirus has tissue specificity—the ability of certain types of HPV to infect tissue specific to their localization. In this case, the type of virus determines the clinical features of the infectious process.
One of the most common pathologies resulting from infection of the skin and mucous membranes with papillomaviruses are warts, which are benign epithelial tumors.
Among warts, there are 8 clinical varieties, each of them is associated with certain HPVs: vulgar warts (1–4, 27th, 29th, 57th HPV genotypes); deep palmoplantar warts (1st, 3rd, 27th, 29th, 57th); mosaic plantar warts (2nd, 4th); cystic warts (60th); flat warts (3rd, 10th, 28th); “butcher’s” warts (7th); focal epithelial hyperplasia (13th, 32nd); verruciform epidermodysplasia (5th, 8–10, 12th, 15th, 19th, 36th) [1].
The group spread of warts, as a result of direct and indirect contact with patients, is characterized by a high incidence rate, amounting to 7–12% in adults, and up to 10–20% in school-age children [1]. The incubation period varies from 1 to 6 months, but can be over three years. Within two years, up to 40–65% of warts regress on their own. In other cases, they continue to increase in size and over time may become more resistant to therapeutic effects [1, 6].
The most common types of warts encountered in clinical practice are vulgar and flat warts. Vulgar warts, which are predominantly caused by HPV types 2 and 4, clinically present as multiple painless dense round gray papules with a diameter of 0.2–0.5 cm with an uneven, keratinized surface of flesh-colored or yellow-brown color, most often located on dorsum of the hands. However, rashes can also be located on other areas of the skin [7].
Flat warts, most often localized on the back of the hands, forearms, face and mucous membranes, are clinically presented as small multiple papules the color of normal skin. They occur in any age category, but are especially common in children and adolescents.
Currently, there are quite a lot of methods for treating warts; they are divided into destructive, chemical, and immunotropic. Depending on the specific clinical situation, preference is given to a certain method of therapy.
The most common methods for removing warts are the use of salicylic acid and cryotherapy with liquid nitrogen. The manual by J. Sterling et al. salicylic acid has been named the drug of choice for the treatment of flat warts on the face, as well as flat and common warts on the hands. Over-the-counter medications contain less than 20% salicylic acid, while prescription medications may contain up to 70% salicylic acid. However, 15–20% salicylic acid is usually sufficient to cure a wart. The use of salicylic acid preparations is considered first-line therapy in the treatment of common non-genital warts [1]. The effectiveness of this effect is quite high; cure is observed in 70–80% of patients [1, 8].
Given the ability of retinoids to influence keratinization processes, accelerating wart removal, some authors recommend their use orally and topically as a second line in the treatment of flat warts [6, 9].
Of the destructive methods in practice, cryotherapy using liquid nitrogen applications is the most widely used. The method is based on rapid freezing of intra- and extracellular fluid, which is subsequently accompanied by cell death and lysis during thawing. Most researchers estimate its effectiveness at 70–75% and recommend its use in the treatment of flat and simple warts as first-line therapy. The method does not require anesthesia or special equipment, large material costs, and is quite simple to implement, which greatly facilitates its use.
Laser therapy, which leads to necrotization of the tissue area with the wart as a result of coagulation of blood vessels, according to some authors, leads to a positive result in up to 50–80% of cases, but the recurrence rate is quite high and amounts to 4–22% [10]. At the same time, it should be remembered that long-term non-healing wounds are fraught with the addition of a secondary infection and the formation of scars at the site of removal. Therefore, it is recommended to use laser for plantar warts as a second-line therapy, and for common and flat warts as a third-line therapy [9].
The ability of HPV to persist in the human body and the formation of secondary immunodeficiency makes it advisable to include in the complex of treatment of patients drugs that disrupt viral replication and improve regeneration. Therefore, in world practice, local agents with antiviral and immunomodulatory effects are widely used to treat warts, the effectiveness of which increases significantly when used sequentially or in parallel in combination with methods of destruction.
At the same time, despite the seemingly wide variety of methods for treating warts, none of them provides a one hundred percent guarantee of a complete cure for the patient. Until now, despite the fundamental discoveries and achievements of modern medicine, for papillomavirus infection, unlike other viral lesions of the skin and mucous membranes, there are no specific treatment methods with an almost complete absence of systemic therapy. Every year, the statistics of HPV-related diseases are steadily worsening, the frequency of recurrence of the pathological process remains high, which dictates the need to search for drugs and new techniques that increase the effectiveness of therapy. This problem becomes especially relevant when it comes to young patients, where it is necessary to eliminate the risk of unwanted drug reactions and complications as much as possible. According to many studies, the most effective method of treating HPV-induced skin tumors is a combination one, combining the simultaneous or phased use of local destructive effects and the systemic use of antiviral and immunoprotective agents. Since only destruction, according to a number of authors, gives a high percentage of relapses within six months, and warts in most cases appear on the same areas of the skin as before. This is probably explained both by the stages of the HPV life cycle, the DNA of which can be detected at a distance of up to 1 cm from the visible boundaries of the tumor, and by a violation of general and local immunity [4].
The purpose of this study was to evaluate the effectiveness and safety of combination therapy for flat warts in children, including the interferon drug Genferon Light and cryodestruction with liquid nitrogen.
Material and research methods
We observed 73 children aged 2 to 9 years with a diagnosis of human papillomavirus infection of the skin, with clinical manifestations in the form of HPV-induced flat warts. The duration of the disease varied from two months to 2.5 years. Almost 90% of children (65 patients) had previously been treated for this disease with local antiviral drugs for 2–3 months, without effect. Warts were localized mainly on the face and the back of the hands. The number of elements on the skin ranged from 2 to 9. All patients were divided into two groups, 35 and 38 children in the first and second, respectively.
In the first group, patients were treated with a destructive method using liquid nitrogen in the form of cryomassage. The applicator with a cotton swab was placed parallel to the surface of the skin and moved with rapid rotational movements with slight pressure over the treated area until the skin became slightly pale. The procedure was repeated 3–5 times depending on the patient’s skin reaction at short intervals (1–2 minutes). More pronounced, raised warts were frozen additionally, with the applicator positioned perpendicular to the lesion, without pressure, for 10–15 seconds, without affecting the surrounding skin. The number of procedures varied from 4 to 5–6. A repeat session was carried out after the reaction (hyperemia) caused by the procedure disappeared. The interval between procedures was 3–4 days.
In the second group, in addition to cryomassage (cryodestruction), an immunomodulatory drug with an antiviral effect, Genferon Light, was simultaneously prescribed according to the following regimen: 1 suppository rectally 2 times a day with a 12-hour break for 10 days before destruction and for 10 days after destruction, in appropriate cases age doses (a single dose for children under 7 years old was 125,000 IU, for children over 7 years old - 250,000 IU). Genferon light, specially created for a special category of patients (pregnant women and children), contains a reduced dose of active ingredients (interferon α-2b (IFNα-2b) at a dose of 250,000 IU and taurine at a dose of 0.005 g). IFNα-2 has pronounced antiviral, immunomodulatory and anti-inflammatory activity. The amino acid taurine has antioxidant and membrane-stabilizing properties, which significantly increases the biological activity of IFNα. All patients were recommended to wipe their skin with a 2% solution of salicylic alcohol as skin care during the treatment period. To prevent the occurrence of hyperpigmentation at the site of removed warts, it was recommended to avoid active insolation for 5–6 months and use sunscreen. The effectiveness of the treatment was assessed by the absence of clinical manifestations of the disease during the year.
results
At the end of therapy, a complete absence of skin rashes (as a result of exfoliation of the stratum corneum along with warts) in the first group was observed in 23 children, which amounted to 65.7%. In 2 (5.7%) patients in this group, flat warts were partially preserved, in 6 (17.1%) children there was a relapse within 1–2 months, in 4 (11.5%) there was a relapse within six months, which required in the future, additional therapy will be prescribed in the form of a combination of cryodestruction with the immunomodulatory drug Genferon light.
In patients of the second group, who received Genferon Light in addition to cryomassage, the effectiveness of therapy was 92.1% (35 children), relapse was recorded in 3 (7.9%) children by the end of the year of clinical observation, and reinfection could not be excluded.
Tolerability of Genferon Light was good in all children. No side effects from the therapy were recorded.
Thus, the inclusion of the immunomodulatory drug with antiviral effect Genferon Light in the complex treatment of flat warts in children can significantly increase the effectiveness of therapy, avoid complications and unwanted drug reactions, which is extremely important in this category of patients.
Literature
- Khlebnikov A.N., Selezneva E.V., Dorokhina O.V. // Bulletin of Dermatology and Venereology. 2015. No. 1. pp. 122–128.
- Manykin AA Papillomavirusa // Medical virology under editions Lvova DK 2008. P. 269–276.
- Kungurov N.V., Kuznetsova Yu.N., Gorbunov A.P., Tolstaya A.I. Combined method of treatment of palmoplantar warts // Pharmacotherapy in dermatovenerology. 2011. No. 2. P. 62–69.
- Molochkov A.V., Khlebnikova A.N., Lavrov D.V., Gureeva M.A. Genital papillomavirus infection. Tutorial. 2010. 10 p.
- Rogovskaya S.I. Human papillomavirus infection in women and cervical pathology. M.: GEOTAR-Media, 2005. pp. 15–17.
- Belyaev V.V., Myasnikov L.L. Plantar, flat, vulgar warts: modern approaches to treatment // Clinical dermatology and venereology. 2012. No. 6. P. 55–58.
- Stirschneider Yu. Yu., Volnukhin V. A. // Vest. dermatology and venereology. 2013. pp. 65–70.
- Cockayne S., Hewitt C., Hicks K. et al. EVerT Team. Cryotherapy versus salicylic acid for the treatment of plantar warts (verrucae): a randomized controlled trial // Br. Med. J. 2011: 342: d3271.
- Bacelieri R., Johnson S. Cutaneous Warts: An Evidence-Based Approach to Therapy // Am Fam Physician. 2005, Aug 15; 72(4):647–652.
- Mavrov G.I., Shcherbakova Yu.V., Chinov G.P., Nagorny A.E. Methods for diagnosing and treating skin lesions caused by the human papillomavirus // Dermatology and Venereology. 2010. No. 2. P. 49–60.
E. I. Yunusova1, Candidate of Medical Sciences L. A. Yusupova, Doctor of Medical Sciences, Professor G. I. Mavlyutova, Candidate of Medical Sciences Z. Sh. Garayeva, Candidate of Medical Sciences
GBOU DPO KSMA Ministry of Health of the Russian Federation, Kazan
1 Contact information
Treatment of warts in St. Petersburg
Treating warts requires a lot of patience. Warts may appear and disappear for no apparent reason or for reasons that are difficult to identify. High infectivity and autoculation of warts are arguments in favor of removal.
There are many different treatment methods. Therapeutic choices differ depending on the type of wart, its location, depth, number and extent of the affected area of skin.
Treatment for warts can produce very different results. Some warts respond to treatment while others do not, even if it is given to the same person.
Treatment often requires repetition over several weeks, months and in extreme cases even years before success is achieved. But in any case, wart removal should be performed in a clinic by a dermatologist. Self-medication is highly discouraged, as the consequences may be irreparable.
The most gentle and universal ways to get rid of warts of all types are laser and radio wave therapy.
Laser wart removal
Today, laser surgery is one of the best ways to get rid of warts. This is a painless and safe procedure that can be used in areas of maximum sensitivity. Laser removal of tumors is very effective: the likelihood of relapse is minimal. This is significantly influenced by the severity of the disease.
Warts are removed by layer-by-layer cauterization of the affected area, thanks to which the doctor controls the depth of the effect. At the same time, the laser beam cauterizes the blood vessels, thereby preventing bleeding at the site of exposure.
Three methods of laser coagulation are common:
- Carbon dioxide (CO2) laser. Procedures using this laser are more painful. Although the CO2 laser seals the blood vessels, it also kills the wart tissue. In this process, there is a possibility of damage to healthy tissue. Wound healing usually takes longer, and scar formation is possible. The efficiency is about 70%.
- Erbium laser. It is characterized by a shorter wavelength. The likelihood of scar formation after healing is significantly reduced.
- Pulsed dye laser. This laser more effectively seals the blood vessels that feed the wart. It does not damage much of the healthy tissue like a CO2 laser does. It is also the only type of laser approved for use on children. The effectiveness of this treatment method is about 95%.
| Advantages | Flaws |
| Minimum likelihood of scar formation (depending on the degree of neglect of the pathology) | High price |
| Fast tissue healing | |
| High efficiency of the method | |
| Minimal damage to healthy tissue | |
| Speed of the procedure |
Wart removal is performed under local anesthesia. A crust remains at the cauterization site, which disappears within 14 days. After the procedure, the patient quickly returns to his normal lifestyle, provided that all doctor’s recommendations are followed.
Removal with a radio knife
The most effective modern method of getting rid of warts is removal by radio waves. First of all, this is due to the fact that in this procedure the instruments do not contact the patient's body: they are produced at a radio wave frequency.
Under the influence of radio waves, the skin does not overheat, blood vessels do not bleed, and all types of viruses die instantly. Thus, the growth is easily removed, and the likelihood of further development of the virus is completely eliminated.
Other advantages of radio wave wart removal should be noted:
- complete painlessness;
- speed of the procedure;
- exclusion of edema and infiltration;
- absence of postoperative complications;
- absence of scars at the site of wart removal;
- quick rehabilitation period.
The procedure is also performed under local anesthesia. After exposure, a crust forms on the affected area of the skin, which disappears on its own within 7-10 days.
As noted above, warts often affect the genital area. Removing anogenital growths (condylomas) usually frightens patients. However, the radio wave method in this case is the most effective and causes minimal pain.
If you find an error, please select a piece of text and press Ctrl+Enter
Strengthening the immune system
Modern medicine has not yet learned to kill viruses. But an important fact is that HPV carriage is not lifelong. In addition, medicine has a small number of means at its disposal that allow it to remove some of the viruses from the body. The use of these drugs is fully compatible with immunomodulatory therapy.
The amount of virus in the body is directly related to the state of the body’s immunity - the better the immunity, the less virus. Therefore, the most promising way to reduce the concentration of HPV in the body is to strengthen the immune system. For this purpose, a separate course of treatment is carried out, after which the person begins to feel much better.
Finally, there are very effective preparations for topical use - creams, gels, sprays that increase local immunity and reduce the concentration of the virus in the affected tissues.