How the disease develops
In a woman's body, one egg matures every menstrual cycle. This happens in the most mature follicle, which is called dominant.
Reference! Follicle is a structural unit of the ovary in the form of a vesicle that contains immature eggs (ovocytes).
The dominant follicle secretes hormones that inhibit the development of other germ cells, so only one of them matures. After the egg has matured, the follicle ruptures and it begins its movement through the fallopian tubes to the uterus, gradually maturing and preparing for fertilization. If the follicle does not rupture, its contents turn into a cyst - a bubble-like tumor formation.
Reference! A cyst is a hollow formation in tissues or organs that has a wall and contents.
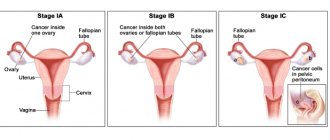
Based on their location, they are divided into the following types:
- unilateral (right- or left-sided);
- bilateral (extremely rare).
For any complications that arise:
- ordinary (uncomplicated);
- complicated.
Typically, cysts are small in size (3–5 cm), but it happens that they grow up to 10 cm. Most often, right-sided cysts occur. This happens because the right ovary is supplied with blood from the abdominal aorta, and the left one from the renal artery. This means that a more intense blood supply determines greater activity of the right ovary.
Cysts can be hormonally active and additionally produce the female sex hormone estrogen. This leads to its excess in the woman’s body, and as a result – disruption of the menstrual cycle.
A follicular ovarian cyst cannot develop into a malignant neoplasm. But it is dangerous because it can become a source of inflammation, which disrupts the function of the entire ovary, which can lead to menstrual disorders and even infertility. In addition, an inflamed cyst can rupture and cause a serious illness - peritonitis.
Ovarian cysts - symptoms, signs, clinical manifestations, diagnosis and treatment methods
Hello Konstantin Viktorovich.
Elena Pavlova writes to you, (Samara), for the last 2 years I have lived like in a nightmare, I remember my last “favorable visit” to the gynecologist when, after an examination, she said that everything was fine with me and there was no reason to worry, after 6 months At an appointment with another gynecologist, she immediately sent me for an ultrasound. The diagnosis sounded like a death sentence: uterine fibroids of 8 cm, a large ovarian cyst, adhesions and obstruction of the tubes and a bunch of other ailments. And the examinations began, each time there were more and more new sores, each doctor gave me his own diagnosis and it was more and more terrible, all these endless queues in hospitals, tests, tears, despair, mistakes, indifference and indifference of doctors and none of them did not promise me to save my female organs. Then I was 31 years old and had not yet given birth, but no one cared. I did not agree to the operation, continuing to go to doctors, calling all my friends, looking for information on the Internet, in other cities, with the hope that someone would still help me. For all these consultations and examinations, I paid quite a large amount of money. So this time flew by, the cyst increased several times, the fibroid also grew, and 3 more small fibroids were discovered. The doctors at our oncology center didn’t even want to talk about preserving organs, having lost all hope, I opened the Internet for the last time, before the operation, sat there all day, and only late at night I accidentally found a website about the Swiss University Clinic and Konstantin Viktorovich Puchkov. I read the reviews until the morning and didn’t believe that it was all true. I no longer had a choice, because the doctors in my city refused to help me and I wrote a letter to Konstantin Viktorovich, although, to be honest, I did not even hope that I would receive a letter in response. And suddenly OH MIRACLE!!! After 2 days, Konstantin Viktorovich sent me a letter saying that organs can and should be preserved. I went to Moscow with little hope and faith in the best surgeon in the world. Everyone tried to dissuade me from going, the doctors insisted that miracles don’t happen and you’ll just leave all your money there and come back to us for help. At the clinic, I couldn’t believe myself, as if I was in a fairy tale: sweet and polite girls at the reception, kind, attentive, responsive doctors. The entire examination and tests went so quickly and painlessly that I did not expect it; I received competent and clear advice. Konstantin Viktorovich immediately warned that it would be necessary to do 2 operations and reassured me by promising to save the organs, first to remove a huge ovarian cyst, and after a few months to remove the fibroids. I had my first operation in February 2015, and a few days later I was already at home. Having been in the golden hands of a most experienced surgeon and his colleagues, I no longer had any doubt that I would perform the second operation only in a Swiss clinic. I went to the next operation, which took place in December 2015, without fear - with full confidence that Konstantin Viktorovich would save my organs. At that time, I only had 3 small lines left, traces reminiscent of the operation. During the second operation, 11 fibroids were removed, instead of the discovered 4, one of which was 12 cm. Despite the fact that abdominal surgery was performed, the next day I was already moving around, and 4 days later I was going home to Samara.
I would like to thank all the employees of the Swiss University Clinic, and especially Lyubimova Elena Anatolyevna, Agisheva Valeria Vladislavovna for their attentive attitude, careful and very careful examinations, for their kind eyes and understanding, for their clear and competent consultation. Thanks to Leonid Venidiktovich, the anesthesiologist who worked during the operation, the nurse Nastenka, who nursed me after anesthesia, and the other nurses who looked after and helped after the operation. Special thanks to Olga Troitskaya for prompt preparation for the operation.
The Swiss University Clinic employs not just doctors, but DOCTORS with extensive experience and ability, who are not afraid to trust with their lives. The clinic has not just a team - it is one team working clearly and harmoniously.
Dear Konstantin Viktorovich, I express my sincere gratitude and low bow to you for saving my life, for giving me hope for the opportunity to become a mother and I will try to make it come true. For your golden hands, energy, sunny smile, experience, talent, kindness, cheerfulness, for your kind heart. I thank the Lord God that he directed me to your clinic. God bless you. Sorry if I forgot someone or wrote something wrong, for the verbosity.
Sincerely, Elena Pavlova, Samara [email protected]
Follicular cyst - causes
The main reason is a hormonal imbalance in a woman’s body, which leads to a cycle without ovulation (anovulation). The cause of hormonal imbalance and the development of a follicular tumor may be:
- termination of pregnancy (abortion);
- inflammatory diseases of the genitourinary system;
- sexual infections;
- genetic predisposition;
- misuse or abuse of contraceptives;
- too strong stimulation of ovulation in the treatment of infertility;
- excessive physical or emotional stress;
- endocrine diseases (thyroid, adrenal glands, diabetes);
- stress.
Reference! Hormonal imbalance can occur due to a common cold.
Causes of cyst formation
So far, experts cannot say unequivocally why ovarian cysts form. However, it is believed that hormonal imbalances are the basis, which can be triggered by various factors:
- inflammatory diseases (both pelvic organs and other body systems);
- endocrine pathology;
- absence of pregnancies during the reproductive period of life;
- repeated artificial termination of pregnancy;
- menopause, as well as the period preceding its onset (perimenopause);
- taking certain medications.
There is evidence of a certain proportion of hereditary predisposition.
Formations are detected both during reproductive age and after the onset of menopause.
Follicular cyst - symptoms
The disease is sometimes practically asymptomatic and is detected during a preventive gynecological examination.
However, more often it is characterized by the following manifestations:
- various disorders of the menstrual cycle: changes in the duration and interval between menstruation, the abundance of discharge;
- bleeding not associated with menstruation;
- pain in the lower abdomen, aggravated by physical activity or sex;
- general weakness.
Similar symptoms are observed with uncomplicated small cysts. They may resolve on their own over time. If the body fails to cope, the cyst progresses, and the severity of painful manifestations increases.
With complicated and large formations, the following symptoms appear:
- nausea, vomiting;
- dizziness;
- increased heart rate;
- presyncope and fainting;
- abdominal enlargement;
- decreased blood pressure;
- sudden sharp pain in the lower abdomen;
- bleeding.
These are life-threatening conditions for the patient that require prompt medical intervention.
Dangerous consequences
Cystic formations, depending on their type, affect the body differently. Thus, a corpus luteum cyst and a follicular cyst can disappear on their own or during hormonal therapy. And endometrioid and mucinous have a risk of degeneration into cancer cells. This is why it is so important to promptly diagnose and begin treatment for ovarian cysts. In the most dangerous cases, surgical intervention is resorted to. Removal of an ovarian cyst is currently carried out with minimal trauma to surrounding tissue. This allows a woman to maintain reproductive function. If possible, gynecologists perform laparoscopy of an ovarian cyst, a minimally invasive operation.
At the ABC-Medicine network of clinics, you can always undergo a gynecological examination, which will allow you to promptly identify this disease and take appropriate measures to treat it.
Our offices are equipped with all the necessary equipment to identify this pathology and determine the degree of its development. Gynecologists perform both a traditional examination with medical history, as well as colposcopy, ultrasound and MRI. With an uncomplicated course of the disease, expectant management and hormonal treatment are possible. Our gynecologists resort to surgery for ovarian cysts only if conservative therapy does not bring the desired result. After completing the course of treatment, specialists will provide detailed recommendations on how to prevent this disease.
To make an appointment for a gynecological examination, please call + 7.
Complications
If the follicular cyst was not diagnosed and treated in time, the following consequences are possible:
- Cyst rupture. Happens spontaneously. Accompanied by sharp pain. Possible bleeding, even to the point of shock. The likelihood of rupture increases due to intense physical activity or sexual intimacy.
- Hemorrhage into the cavity. Penetration of blood into the cystic bladder.
- Torsion. With a sudden change in body position, torsion of the ovary can occur, during which the blood vessels are compressed and its blood supply is limited. Accompanied by sharp pain until loss of consciousness
- Inflammation. The contents of the cystic vesicle can become inflamed and even fester, forming an abscess. Rupture of an inflamed cyst is dangerous by infecting surrounding tissues.
Ruptured ovarian follicular cyst
Apoplexy or cyst rupture is a common complication of the disease. The reason can be both internal and external factors. A cystic blister cannot grow indefinitely. When it becomes significant (7 centimeters or more), its shell becomes thinner and rupture may occur.
Internal causes of rupture presumably include:
- disturbed hormonal balance;
- irregular menstrual cycle;
- inflammatory processes of the abdominal cavity;
- gynecological diseases.
External reasons include:
- intense physical activity;
- lifting weights;
- sudden movements such as jumping;
- falls;
- traumatic effects directly to the abdominal area.
In the event of a rupture, the contents spill into the abdominal cavity of the small pelvis and can cause serious consequences, including peritonitis. If the blood vessel supplying the follicle is injured, heavy bleeding may occur, both through the uterus outward and inward into the abdominal cavity.
Based on symptoms, ruptures are divided into three types:
- painful apoplexy (pseudoappendicular) - accompanied by sharp pain and reminiscent of an attack of acute appendicitis;
- anemic - accompanied by internal bleeding;
- mixed type - internal bleeding is accompanied by acute pain.
According to the degree of manifestation, the gap is divided into the following types:
- light, in which case the blood flows out slightly (up to 150 ml);
- moderate, significant hemorrhage (up to 500 ml);
- severe, blood loss exceeds 500 ml.
The rupture is accompanied by severe pain, up to painful shock. Bleeding can also cause loss of consciousness.
In the event of a rupture, urgent surgical intervention is almost always required.
Hemorrhage into the cyst cavity
With an active blood supply to the dominant follicle from which the tumor was formed, blood can actively penetrate into the bladder. This threatens ruptures and bleeding into the abdominal cavity. This structure often serves as a source of acute inflammatory process. A cyst with hemorrhage into the cavity is called hemorrhagic.
Signs of torsion of a follicular ovarian cyst
Quite large tumors are susceptible to twisting - more than 7 cm in diameter. As a result, the neurovascular bundle of the ovary is compressed, and the following symptoms occur:
- weakness;
- dizziness;
- a sharp decrease in blood pressure;
- nausea, vomiting;
- rapid heartbeat (tachycardia);
- stopping bowel functions;
- the pain does not subside in any position of the body.
Torsion can be partial or complete (more than 360 turns). It can only be eliminated by surgical intervention (usually laparoscopic).
To avoid such a complication, during treatment it is necessary to exclude active training, extreme travel and switch to a gentle regime of physical activity.
What are ovarian cysts?
Ovarian cysts are divided into:
- functional, the formation of which is directly related to the activity of the ovary. Detected in 90% of cases;
- organic, which are essentially tumor-like formations. These cysts, unlike functional ones, do not shrink or resolve on their own over time.
Let's take a closer look at the classification of ovarian cysts, which is based on their structure and method of formation.
Follicular cyst
This is the most common formation. Most often it develops in women of reproductive age. Much less often, follicular cysts are detected in the postmenopausal period (within 5 years after the last menstruation). Their development is due to the fact that the dominant follicle, due to a number of changes in the hormonal profile, did not undergo ovulation. As a result, it remains, increases in size and releases high levels of estradiol, which can disrupt the normal menstrual cycle.
There are cases where follicular cysts were found in newborns. This is due to the hormonal surge during childbirth. In approximately 50% of cases, they disappeared on their own within 1.5 months.
In some cases, treatment of a follicular cyst is required. It will be conservative, medicinal.
Luteal cyst
A corpus luteum cyst is formed in the second half of the menstrual cycle from the corpus luteum that appears after ovulation. This can be facilitated by various factors: changes in the endocrine system, characteristics of the blood supply to the ovary, chronic inflammatory diseases and other disorders. In this case, the corpus luteum, which appears in place of the dominant follicle, develops incorrectly. It increases in size, turning into a cyst.
Paraovarian cyst
It is formed from the tissue of the epididymis and is filled with transparent contents. It grows quite slowly, but over time it can reach large sizes (up to 30 centimeters in diameter). As a rule, it is diagnosed in women of reproductive age, less often it is detected in adolescents. It does not regress on its own, so a paraovarian cyst in some cases requires surgical treatment.
Endometrioid cyst
Hemosiderin, contained in blood cells, gives the cyst a specific color, which is why it is also called chocolate. The defeat can be unilateral or bilateral.
An endometrioid cyst is a manifestation of endometriosis. The formation can be of very different sizes (from 10 to 120 mm in diameter), and can cause an increase in the CA-125 tumor marker. It is diagnosed in women of reproductive age, in some cases in combination with pathologies such as fibroids and endometrial hyperplasia (overgrowth).
Cystadenomas
Also benign formations include cystadenomas; they are serous and mucinous. Mucinous cystadenoma tends to grow rapidly and has mucin-containing mucus inside. Most often it is diagnosed in patients of late reproductive age, as well as after menopause. Malignant transformation occurs in approximately 15% of cases.
Dermoid cyst
Teratomas (dermoid cysts) can be detected at any age in ovarian tissue and carry the rudiments of other tissues. These can be dermoid derivatives (the rudiments of skin, hair) or other tissues. Teratoma can reach 15 centimeters or more in diameter. This is a unilateral formation, which malignizes on average in 2% of cases.
Diagnosis of the disease
The following methods are used to detect pathology:
- Two-handed palpation - during the initial gynecological examination allows you to identify large tumors.
- Ultrasound diagnostics (ultrasound) makes it possible to examine the structure of the ovary and identify even small tumors. The procedure does not cause discomfort or pain.
- Dopplerography - examination of the state of the pelvic vessels allows you to assess the degree of blood supply to the ovaries.
- Serological tests - blood tests for hormones, allows you to determine the hormonal status of a woman. The result is important for the choice of drug treatment.
For a more accurate diagnosis, several methods are usually prescribed, such as ultrasound and serology.
Diagnostics
Typically, an ovarian cyst is discovered randomly during a routine examination. The doctor prescribes:
- ultrasound examination of the pelvic organs;
- clinical blood test;
- blood test for hCG (to exclude pregnancy);
- smear microscopy;
- analysis to determine the tumor antigen CA-125.
If there is a suspicion of complications, additional diagnostic laparoscopy, puncture of the posterior vaginal vault, computed tomography (CT) or magnetic resonance imaging (MRI) may be required.
Follicular cyst during pregnancy
Most often, the tumor occurs before pregnancy. A pregnant woman should avoid physical and emotional stress. Sharp bends and turns are not allowed.
With a small cyst, vaginal delivery is possible. If it reaches a large size, a cesarean section is necessary, since it may rupture or twist during childbirth. If the condition of the cyst is acceptable, only medical observation is carried out. If rupture or torsion occurs, surgical intervention is necessary. Pregnancy can often be saved.
To avoid such troubles, when planning a pregnancy it is necessary to undergo a complete examination.
Methods for treating ovarian cysts
Treatment of cysts is carried out in two ways - conservatively, that is, with the help of medications, and operatively, that is, surgically.
Conservative therapy
Conservative therapy in this case is based on the use of hormonal drugs. Hormonal contraceptives are widely used to treat cysts; MARVELON is most often prescribed.
Hormonal contraceptives are prescribed for the treatment of functional ovarian cysts and in the postoperative period after removal of remaining ovarian cysts to prevent their re-formation.
For endometrioid ovarian cysts in the postoperative period, in order to prevent relapse, hormonal agents that cause artificial menopause are usually used.
Surgery
Surgical treatment for functional cysts is required only in case of complications, such as cyst rupture or torsion. Organic cysts most often require surgical intervention.
Surgeries to remove ovarian cysts are performed using laparoscopic access (special instruments inserted into the abdomen through small incisions under video camera control). Laparoscopy is also possible during pregnancy, if complications arise from an ovarian cyst. Only for large cysts is it necessary to make an incision on the anterior abdominal wall.
A feature of ovarian surgery is the removal of a cyst or tumor within healthy tissue, that is, the ovarian tissue, which contains many follicles, must remain intact, and the cyst, along with its capsule, is carefully “removed” from the ovary. In rare cases, a so-called ovarian resection is performed, that is, part of it is removed. If the cysts are very large, then in some situations it is practically impossible to find ovarian tissue. In this case, the entire ovary is removed.
After surgical treatment using laparoscopic access, the woman recovers quickly, usually a week after the operation she can already go to work.
Management of pregnancy with ovarian cyst
Planning a pregnancy usually depends on the type of cyst. Most often, conception is recommended 3-6 months after surgery.
During pregnancy, ovarian cysts are monitored using ultrasound and Doppler studies - studying the blood flow in the ovary and in the cyst, monitoring the tumor marker CA-125, the concentration of which increases sharply if the cyst degenerates into a malignant tumor.
If surgical treatment is necessary during pregnancy, it is safest to perform laparoscopy at 16-18 weeks.
Treatment of follicular cyst
If its size is not very large and there is no threat of rupture, conservative treatment is prescribed. For systemic therapy, hormones derived from progesterone are used. Antibiotics are used to eliminate inflammation or avoid infections.
Vitamins are also prescribed: folic acid, ascorbic acid, vitamin E.
In case of severe pain, non-steroidal anti-inflammatory drugs can be prescribed.
If the cause of the disease is hormonal disorders caused by dysfunctions of other endocrine glands (thyroid, adrenal glands), you should consult an endocrinologist.
Surgical intervention
If the formation has reached a large size and complications arise, surgical treatment methods are used.
According to the technique used, surgical intervention is of two types:
- Laparoscopy. Minimally invasive surgery is carried out using a special device - a laparoscope. To carry out the operation, small punctures are made through which a manipulator and a video camera are inserted. It is used in case of large cysts or inflammation.
- Laparotomy. Abdominal surgery. Used in case of complications such as rupture or torsion.
Types by degree of impact:
- Cystectomy. This is a method of enucleating a cyst. Usually only part of the ovary is removed. The remaining portion remains functional.
- Ovariectomy. Removal of the entire ovary. The operation is performed if it has been severely damaged as a result of complications. Since the ovaries are a paired organ, reproductive function is preserved thanks to the remaining one.
The choice of surgical intervention method is influenced by the severity and degree of development of the disease. In any case, doctors try to preserve reproductive function in a patient of reproductive age.
Treatment
In most cases, functional cysts regress on their own within a few months, so dynamic monitoring is required. Ultrasound monitoring will allow you to assess the changes occurring and prevent the development of possible complications.
Based on the results of the examination, the following may be prescribed:
- anti-inflammatory drugs;
- COOK.
If the formation has not disappeared within six months, then we are not talking about a functional, but about a true formation of the ovary. Surgery may be recommended.
Cystectomy is a laparoscopic operation. Gaining access to the ovary requires only a few small punctures, so it is minimally traumatic.
If there is a suspicion that the tumor is malignant or borderline, the scope of surgical intervention can be expanded by the surgeon.