Indeed, certain types of ovarian cysts regenerate on their own, but no one can give an absolute guarantee to such a process, since it is unknown how the pathology will behave under the influence of certain factors.
But a functional cyst is quite capable of negatively influencing the function of reproductive and even nearby organs and causing serious complications at a certain stage of development. Therefore, contacting a gynecologist and at least dynamic monitoring of the tumor is mandatory for patients with any type of pathology.
Classification of cysts of the female reproductive system is carried out regarding their location and contents. There are several types of ovarian cysts.
Causes
The etiology of a functional ovarian cyst is not precisely known. It is believed that the main role in this mechanism belongs to hormonal changes that can occur against the background of:
- pathologies of the endocrine glands;
- taking hormone-containing and certain other medications;
- inflammation of the genitourinary and other body systems;
- pituitary diseases;
- frequent abortions;
- absence of pregnancy during childbearing age;
- premenopause and menopause.
The risk of developing a functional ovarian cyst is higher in women of reproductive age, but older women are often diagnosed with functional formations.
After treatment
After the main stage of treatment, anti-relapse therapy is carried out. It is indicated for recurrent follicular cysts, which always indicate anovulation. Anovulatory cycles are dangerous for the female body, because... increase the risk of obesity, endometrial hyperplastic processes and lead to infertility.
In a multidisciplinary medical center, you can undergo a complete diagnosis of the female body and evaluate the correct functioning of the ovaries. If functional cysts are detected, the gynecologist will draw up a personalized management plan, which is aimed at restoring the normal functioning of the hypothalamic-pituitary-ovarian system.
Sign up for a consultation at a convenient time! Our specialists will help set your reproductive system on a healthy course.
Symptoms
Functional ovarian cysts are usually small in size up to 1.5 cm, rarely the formation reaches 5 cm or more. At the beginning of its formation and at first the functional neoplasms do not manifest themselves in any way, so the woman is not aware of the condition of her affected ovary. Sometimes unexpressed manifestations are possible as long as there are no complications.
A gynecologist may suspect a functional ovarian cyst based on the following signs:
- feeling of heaviness in the lower abdomen;
- nagging pain;
- cyclical disorders;
- metrorrhagia not associated with menstruation.
Symptoms become more intense with physical overload, during and after sex. This may cause nausea, weakness, soreness and breast enlargement. If a functional ovarian cyst has reached a large size, then the woman’s abdomen enlarges.
Contact us for qualified help
Do not self-medicate. At the first symptoms of the disease, consult a doctor.
Prevention
There are no specific preventive measures to prevent the formation of a functional ovarian cyst. The main task of women facing this disease is to increase immunity, regularly visit a gynecologist for preventive purposes, lead a healthy lifestyle, and get rid of bad habits.
Other useful tips:
- control body weight;
- have a protected sex life;
- try to eliminate the stress factor;
- limit heavy physical activity;
- promptly treat inflammatory and infectious diseases of the genitourinary system.
Diagnostics
Most often, a woman learns about the presence of a functional ovarian cyst when visiting a gynecologist for a routine examination or for another reason. To confirm the diagnosis, the doctor prescribes transvaginal ultrasonography. Since cystic formations occur only on one side, ultrasound diagnostics determines a functional cyst of only the left ovary or only the right. To exclude inflammation, blood and a smear are taken from the patient for examination. A pregnancy test is required. To exclude a cancerous tumor, testing for a tumor marker (CA-125) is done.
Complicated functional ovarian cysts require more detailed diagnosis:
- diagnostic laparoscopy will reveal torsion of the cystic pedicle, rupture of the capsule and at the same time eliminate these complications, as well as remove the formation itself;
- puncture of the posterior vaginal fornix is performed if there is a suspicion of the presence of abdominal fluid or blood in the peritoneum;
- CT, MRI, and radiography are necessary to differentiate a functional cyst from other neoplasms.
After laparoscopic diagnosis, a fragment of biomaterial is sent for morphological examination.
Treatment at the Yusupov Hospital
Specialists at the Yusupov Hospital provide patients with high-quality medical services that meet international standards. Treatment of ovarian cysts in women at the Yusupov multidisciplinary hospital is carried out with the participation of oncologists who regularly improve their qualifications and improve their existing skills.
During the appointment, oncologists at the Yusupov Hospital tell the patient who has been diagnosed with an ovarian cyst what types there are and what treatment is most appropriate. When developing a treatment plan, specialists choose the most gentle methods that are highly effective.
Modern medications in combination with minimally invasive techniques used at the Yusupov Hospital help preserve women’s reproductive health. If you have been diagnosed with a serous ovarian cyst or other types, make an appointment with an oncologist by calling the Yusupov Hospital.
Treatment methods for functional cysts
As a rule, a thin-walled functional ovarian cyst of a small size (up to 1 cm) without signs of malignancy resolves on its own within two to three months. In this case, treatment is not required; a wait-and-see approach is used, in which the pathology is monitored using ultrasound diagnostics. For inflammation and other health problems, a woman is treated conservatively. Hormonal (COC) and anti-inflammatory drugs are prescribed. The treatment is carried out under ultrasound control, its goal is to prevent growth and complications or reduce the size of the formation.
If the pathological formation does not disappear within three or more menstrual cycles, the patient complains of pain, then the doctor decides on surgical treatment. Surgical treatment aims not only to remove the functional cyst, but also to preserve the integrity of the ovary, as well as reproductive health.
Surgical treatment is carried out using minimally invasive technologies:
- puncture with aspiration;
- laparoscopy of ovarian cyst.
A functional ovarian cyst is punctured with a special needle, which is inserted using a puncture attachment on a transvaginal ultrasound probe. The liquid is aspirated (pumped out) and sent for cytological examination. Instead, ethyl alcohol (10-15 ml) is injected, which has a sclerosing effect. With this treatment, the best results are observed in patients of reproductive age.
Surgical treatment is indicated for ineffective conservative treatment, complicated course of the disease, and space-occupying formations on the ovaries. After mandatory diagnostics confirming the diagnosis, the patient undergoes preoperative preparation before surgical treatment. You need to do an FLG, an ECG, take a vaginal smear for microflora, blood and urine tests, and consult an anesthesiologist.
The laparoscopic technique is most suitable for cystectomy. The patient receives anesthesia. The gynecologist surgeon makes several small holes on the abdominal wall for inserting endoscopic instruments and a miniature camera through them, with the help of which the doctor controls the entire surgical process. Carbon dioxide is supplied to the abdominal cavity to improve visibility of the surgical field. The doctor cuts the capsule of the tumor, removes it with micro-instruments; if it is voluminous, then first the contents are aspirated, part of which is sent for laboratory testing. The incisions are sutured, leaving almost invisible marks in their place.
The operation lasts no more than 50 minutes, the woman is transferred to the ward, after 2-3 days she can go home if the outcome of the intervention is successful.
Ovarian cysts
Ovarian cyst is a common diagnosis. However, most often there is nothing to worry about. Most ovarian cysts are benign and go away on their own, but there are exceptions that are best known in advance.
Concept and symptoms
A cyst is a thin-walled formation filled with liquid contents. Sometimes, instead of fluid, there may be blood, fat, or other tissue inside the cyst. Cysts on the ovaries occur at any age, starting from the prenatal period of development of a female fetus, but are more often found during reproductive age.
Sometimes cysts can cause dull, aching pain in the lower abdomen, which appears for no apparent reason, either during physical activity or during sexual intercourse. And it is extremely rare to feel sudden sharp pain in the lower abdomen, nausea, forcing you to immediately seek help. This means that the cyst has ruptured or twisted.
But in most cases, ovarian cysts do not cause any symptoms at all. Doctors discover them by chance during an examination on a chair or during a pelvic ultrasound (PUS). This means that you can’t focus on “it hurts or it doesn’t hurt.” Scheduled examinations by a gynecologist are needed.
Types of cysts and treatment approaches
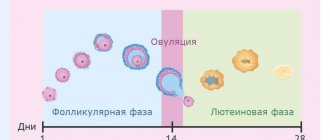
1. Most often, women encounter functional cysts
, which are divided into:
- follicular cysts
are actually an overgrown follicle, growing up to 3 cm or more; - Corpus luteum cysts
are an overly large corpus luteum with a pronounced fluid component. Such a cyst can accompany pregnancy, providing the fertilized egg with a sufficient amount of progesterone.
Most often, functional cysts are an accidental discovery during an examination or ultrasound examination. Sometimes they can make themselves felt by pain or cycle disorders. In any case, such lesions usually completely regress within 6-8 weeks, in most cases without any treatment.
2. Cystadenomas
- more insidious cysts. They can reach large sizes and look quite scary. Ultrasound reveals papillary growths, parietal inclusions - everything is very impressive. This cyst has a malignant form - cystadenocarcinoma, aggressive and dangerous. Treatment is only surgical.
3. Endometriomas
- “chocolate” cysts, filled with viscous, thick contents reminiscent of melted chocolate. They begin to grow on the surface of the ovary and protrude inward. Treatment is only surgical, but the approach must be differentiated. If the endometrioma is small and does not grow, it will not interfere with pregnancy, and during the operation the ovarian reserve will be severely damaged. If the endometrioma is more than 3 cm, then the reserve will suffer - it will crush and damage good follicles, so surgery is necessary.
Teratomas are sometimes found in the ovaries, as in other organs.
(or
dermoid cysts
) - formations consisting of cells of nails, hair, skin, teeth, fat and other passions. The tissues within a teratoma are ALWAYS foreign to the anatomical location (in this case, the “dental tissue” in the ovary is clearly not in place). Teratomas do not resolve in any way; their drug treatment is completely pointless. If the teratoma is very small, it can be monitored using ultrasound. But if the size of the formation is more than 3 cm, treatment is only surgical. Teratomas have a malignant form (immature teratoma that can grow into surrounding tissues and metastasize), so you should not delay the operation.
Polycystic ovary syndrome
is not “horror, horror, a lot of cysts.” This is a completely different disease, which we have already talked about.
In fact, there are many more types of ovarian tumors—several dozen. The final diagnosis, answering the question of what kind of cyst we encountered this time, will be given by a pathologist who will examine the removed tissue and give a histological conclusion. Based on this conclusion, the attending physician will build a further treatment/observation plan.
This is why it is so important not to be lazy and go “for histology” in a couple of weeks or make sure that the conclusion is sent to you by mail. You will then show these documents to your attending physician. But general phrases like “they said that the histology is good” will certainly please the attending physician, but will not help him make important clinical decisions.
Should we observe or operate?
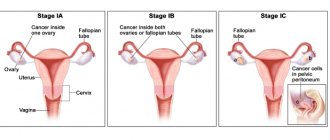
If the cyst is large (more than 5 cm), has a suspicious echostructure, or causes pain, surgery will be the right choice of treatment. Observational tactics depend on the woman’s age, ultrasound picture and the level of the Ca-125 tumor marker.
During reproductive age, if the cyst does not bother the patient in any way, the doctor may suggest repeating the OMT ultrasound in 6–8 weeks. In most cases, the cyst will disappear or shrink in size. If the cyst does not increase in size and its structure does not change over a long period of time, observation can be continued.
In postmenopause, the risks increase, you will have to be examined more often - after 55 years, even a small, seemingly harmless cyst can turn out to be cancer at an early stage, discovered by chance. Therefore, we will need a tumor marker test and frequent monitoring until we are sure that it is not cancer. For diagnosis, the most important thing is that cancer grows: everything that does not grow is not cancer.
What if we miss cancer?
This question always worries both the doctor and the patient. Unfortunately, the world has not yet come up with any method of screening for ovarian cancer. Perhaps because this disease is very diverse and has dozens of varieties. Unfortunately, the diagnosis of ovarian cancer is made almost by accident or late - when a huge belly filled with fluid has grown and pain has appeared. This is why the doctor will be especially picky about any ovarian cysts in high-risk patients:
- age over 55 years;
- family history of breast cancer, ovarian cancer, colon cancer, or endometrial cancer;
- personal history of breast cancer;
- mutations in BRCA1/BRCA2 (see the story about Angelina Jolie and cancer);
- absence of childbirth;
- infertility;
- endometriosis;
- Lynch syndrome (hereditary colon cancer without polyposis).
Tumor markers: urgently?
Many patients place excessive hopes on determining the level of the tumor marker Ca-125 in the blood. Not long ago, they even tried to use this indicator as a screening indicator, including it in the medical examination program.
Unfortunately, ovarian cancer is not diagnosed based on the results of the Ca-125 test, because a normal result does not mean that there is no cancer - that’s just it. Ca-125 can be elevated in other diseases (for example, endometriosis, heart failure, inflammatory diseases, liver and kidney diseases) - to name two. Nevertheless, a significant increase in this marker is diagnostically important. Most likely, cancer has actually been detected. But the norm or a slight increase does not provide information about the presence or absence of cancer.
Ca-125 can be looked at if an ovarian cyst is discovered in postmenopause, if a young woman has a very large cyst or its ultrasound picture is suspicious. There is a whole group of tests for tumor markers that can be used, but the results of these examinations should be treated with great caution. Tests are performed every 3 to 6 months until the cyst disappears or until a decision is made about surgery.
Oksana Bogdashevskaya
Photo istockphoto.com
Expert opinion of a doctor
Butunov Alexey Andreevich
Obstetrician-gynecologist, laparoscopist surgeon, oncologist. Doctor of the highest category.
In advanced cases, with severe complications, oophorectomy is performed according to indications, when the ovary is removed along with the formation, although this is rare in the functional type. Rehabilitation after laparoscopy takes only 2–3 weeks. All this time, the patient is observed by the attending physician, control ultrasound diagnostics, anti-inflammatory and symptomatic therapy are carried out. The patient must follow medical recommendations, avoid physical activity and exercise, do not take a hot bath, refuse other thermal procedures, avoid sex for a while, and adhere to the recommended diet. Control ultrasonography should be performed 2 months after surgical treatment.
Complications
Functional cysts account for 90% of all ovarian tumor formations, of which 80% are follicular. Most of them undergo reverse development, but some reach significant sizes, which leads to overstretching of the cystic membrane, increasing the risk of such complications:
- leg torsion;
- capsule rupture;
- leakage of contents into the peritoneum, which can cause peritonitis;
- hemorrhage;
- menstrual irregularities.
The most dangerous is torsion of the leg, which can lead to rupture of the membrane, leakage of fluid and hemorrhage into the peritoneum.
This causes severe symptoms: febrile temperature up to 40 degrees, dyspeptic disorders, severe pain in the abdomen, tension in the anterior abdominal wall. This condition requires urgent professional help and is subject to further long-term treatment.
Types of treatment
Uncomplicated functional cysts, as a rule, do not require specific treatment, because are a physiological state. However, those causes that lead to menstrual irregularities are subject to treatment. This may include corrective hormonal therapy, anti-inflammatory treatment, and other treatment options.
Usually, without treatment, reverse regression of a functional cyst occurs within 3-6 months, but observation is allowed for 1 year. If regression has not occurred during this time, and the formation is large (more than 10 cm) and causes discomfort to the woman, then surgical treatment is performed. The operation is performed laparoscopically. This method of surgery is characterized by a gentle effect on tissue and a short recovery period.
If a cyst exists for a long time, it is not possible to determine whether it is follicular or luteal. Therefore, such a formation is designated as a simple cyst.