Classification of pathology
There are several classification systems for aortic dissection.
Cardiac surgeon Michael de Baiki proposed a system based on the anatomical location and extent of damage to the vascular wall. The types of dissection are as follows: • Type I – the pathological process involves the ascending part, the arch and, often, the descending part of the aorta;
• Type II – only the ascending aorta is affected;
• Type III – the descending aorta is subject to dissection:
a – the process is limited to the thoracic region;
b – the process also affects the abdominal region.
The clinical classification, called Stanford, divides two options:
• A – the ascending section is affected, regardless of the location of the initial tear of the internal choroid;
• B – the lesion does not affect the ascending part, that is, it begins below the origin of the left subclavian artery.
According to the course, the process of aortic dissection is divided into acute and chronic . A dissection is considered chronic when more than 14 days have passed since its onset, or it is discovered accidentally in the absence of clinical manifestations.
Complications during aortic surgery
Open surgery has a greater risk of early postoperative complications and mortality than endovascular aortic stent graft placement. Mortality after open surgery is about 5%, while after endoprosthetics it is 0.5%.
Other possible complications after resection of an aortic aneurysm:
- Acute renal failure
- Spinal cord stroke with leg paralysis
- High intermittent claudication (pain in the buttocks when walking) claudication
- Colon ischemia
- Embolism of the lower extremities with acute ischemia
- Bleeding from the surgical site and hemorrhagic shock
- Suppuration of the vascular prosthesis
These complications are quite rare. In our clinic, isolated cases of such complications were observed.
Reasons leading to the development of pathology
Dissection of the aortic wall is a multifactorial disease, but almost always occurs against the background of inferiority of its middle choroid. Defects of smooth muscle cells and elastic fibers can be congenital or acquired during life.
The etiological factors for the development of dissection are as follows:
• hypertension, sharp fluctuations in blood pressure;
• atherosclerotic changes;
• genetic defects in the structure of connective tissue (Marfan, Ehlers-Danlos syndromes);
• congenital heart pathology (bicuspid aortic valve, coarctation of the aorta);
• vasculitis (systemic, infectious, toxic);
• damage during diagnostic or therapeutic procedures (catheterization, plastic surgery, prosthetics, etc.);
• chest and abdominal injuries;
• excessive physical and neuro-emotional stress;
• final trimester of pregnancy.
This pathology is diagnosed twice as often in male patients. With age, especially after 60-70 years, the risk of developing the disease increases.
Aortic dissection in people under 40 years of age is usually caused by congenital processes. Women of this age are most susceptible to the disease in the last months of gestation.
Acute traumatic aortic injury: imaging and management
Acute traumatic injury of the aorta (ATI) is fatal in most cases - with such damage, about 80% of victims die before arriving at the hospital. Among the causes of death as a result of road accidents, traumatic brain injury is second only to traumatic brain injury in frequency. With improved imaging options and advances in surgical treatments and percutaneous interventions, mortality among patients with OTPA has decreased from 50% to 5%. OTPA occurs in approximately 2% of blunt chest trauma cases, approximately 70% of which occur in motor vehicle accident victims.
The exact pathogenesis of OTPA is not entirely clear, but the proposed mechanisms are a sharp increase in intravascular pressure (like a water hammer effect) and rupture of the aorta, sandwiched between the vertebral body and the sternum displaced towards the spine (Fig. 1). .
Figure 1 | Mechanisms of aortic injury in patients with blunt chest trauma
The method of choice for diagnosing OTPA is CT angiography, which replaces conventional angiography. It allows you to evaluate intimal disorders and indirect signs of aortic damage, such as periaortic hematoma. In emergency settings, performing ECG-gated CT to visualize the aorta is impractical due to lengthy setup times, the need for additional preparation, and prolonged patient breath holding. With the advent of new dual-source CT scanners with ultra-fast acquisition speeds, it has become possible to obtain virtually “still” images without the motion artifacts seen in the heart and aortic root with traditional CT scanning. With these images, radiological assessment of OTPA can be used to determine patient management and prognosis.
Next, we will describe current aspects of imaging, radiological classification, diagnosis and management of patients with OTPA, as well as recent advances that have a significant impact on the accuracy of imaging in patients with this injury.
Due to its diagnostic capabilities and availability of the method, CT angiography is the study of choice for diagnosing OTPA. The most commonly injured areas are the aortic isthmus, ascending aorta, and aortic hiatus, and arterial phase CT scans of the chest and upper abdomen should be obtained in patients with blunt trauma. Most often, CT angiography is performed as part of a general computed tomography when examining patients with polytrauma.
The advent of dual-source CT scanners and scanners with 64 or more slices has revolutionized the use of CT in cardiac and vascular imaging. These scanners have spatial resolutions ranging from 0.25 to 0.47 mm, with most new scanners providing a resolution of 0.33 mm. Also, such scanners have very fast gantry rotation, which leads to a higher speed of image acquisition - still images of even the ascending aorta can be obtained without ECG synchronization (Fig. 2). In addition, motion artifacts from the patient's breathing are minimal, which provides the necessary diagnostic image quality.
Figure 2
ECG-unsynchronized axial CT image at the level of the sinuses of Valsalva (the space between the semilunar valves and the aortic wall) obtained using a new dual-source CT scanner (A) MSCT on a 64-slice scanner in the same patient. Note the absence of ripple artifacts (indicated by arrows) in the new dual-source scanner, even without ECG synchronization.
The rationale for arterial phase imaging of the chest and upper abdomen is that most vascular injuries anatomically occur in these areas unless the patient has additional risk factors such as a pelvic fracture and therefore possible pelvic vascular injury. In addition, arterial phase imaging of the chest alone does not preclude the detection of any serious pulmonary pathologies.
A low-dose delayed phase scan of the abdomen and pelvis is performed if damage is confirmed during the portal venous phase of the study or if kidney or bladder damage is suspected. An initial noncontrast phase is useful in diagnosing intramural hematoma, but is not performed as part of the trauma protocol. The chest and abdominal CT protocol for patients with blunt trauma is shown in Table 1.
Table 1 | CT examination protocol for blunt trauma of the chest, abdomen and pelvis
In each case, sagittal and coronal 3D models are generated through images in the axial plane. Other 3D methods, including maximum intensity projection (MIP) and volume rendering (VR), are created on a separate workstation. Curved aortic reconstructions are created only in cases where stent placement is planned later during surgery. This 3D data modeling is always read in combination with raw data, which greatly assists in surgical planning.
MRI is almost never used to identify injuries in patients with blunt trauma. However, MR angiography is also used to diagnose trauma: this method is mainly used after placement of an endovascular stent or if renal failure precludes CT angiography. The MRI protocol for aortic imaging is highlighted in Table 2. If CT and MR angiography cannot be performed due to renal failure (eGFR < 30), patients are best treated with non-contrast CT for interval changes in aortic diameter.
Table 2 | Protocol of MR angiography of the aorta
Although CT angiography is the definitive modality in most cases, the initial evaluation of injury often begins with a chest x-ray. Data suspicious for OTPA with this research method include:
- mediastinal widening of 8 cm at the level of the aortic arch (or superior mediastinum, measuring approximately 25% of the width of the chest);
- uneven contour of the aortic arch;
- inability to determine the aortopulmonary window;
- darkening of the border of the lung with the aorta;
- deviation of the trachea or nasogastric tube to the right;
- omission of the left main bronchus;
- dilated left paratracheal stripe.
CT angiography has very high sensitivity (approximately 98%) and almost 100% specificity for diagnosis. Signs of OTPA on CT angiography can be divided into direct and indirect.
Indirect signs of PAAD include mediastinal or periaortic hematoma, retrocrural hematoma, or a small caliber of the aorta distal to the injury site. The location of the mediastinal hematoma is critical because if there is a clear layer of fatty tissue between the aorta and the hematoma, alternative sources of bleeding (from a vein, intercostal artery, or bone) should be considered (Figure 3). Periaortic hematoma without any obvious signs of aortic injury may be associated with occult intimal injury. Conventional angiography may not provide sufficient diagnostic imaging in patients with occult intimal injury, so additional use of intravascular ultrasound or transesophageal echocardiography is better. .
Figure 3
A 36-year-old man presented with a mediastinal hematoma and hemothorax. Sagittal (A) and coronal images (B, C) of CT angiography. A clearly defined layer of adipose tissue is identified between the descending aorta and the hematoma (indicated by arrows). This suggests that the aorta is not the source of the hematoma. The source of ongoing bleeding is the intercostal artery (arrow in image C)
Direct signs of OTPA include active contrast extravasation, rupture (or traumatic pseudoaneurysm), intramural thrombus, aortic displacement, and aortic contour abnormality (including sudden change in caliber, also known as pseudocoarctation). When there is a high risk of a mechanism of injury, as in a motor vehicle injury, evaluation of other associated conditions is also critical. Typically, PAH is accompanied by severe head injuries, damage to the lungs and heart, rupture of the diaphragm, intra-abdominal bleeding, and fractures of the pelvis and long bones.
The term minimal aortic injury (MAI) is an evolving concept that was introduced in 1999 by the Presley Center Aortic Trauma CT Grading System (Table 3) to describe injuries that are minor in nature.
Malhotra et al. were the first to describe this injury and defined it as a small (<1 cm) post-traumatic intimal valve with minimal or no periaortic hematoma. Most of these injuries cannot be diagnosed by other imaging modalities before routine use of CT angiography. MPA was initially found in approximately 10% of patients with OTPA, but more recent studies have shown that it occurs in approximately 25% to 35% of OTPA cases. The increase in the detection rate of MPA may be due to a number of factors, such as increased availability of CT angiography, improved CT technology, and improved vehicle safety. The descending aorta is the most common location of MPA, with the aortic isthmus being the second most common site. Although the generally accepted criterion for MPA is minimal or absent mediastinal hematoma, there is no standard finding that defines MPA. Variations in the definition of minimal or negligible aortic injury in various studies are given in Table 3.
Table 3 | Definition of the group of patients with minor/minimal aortic injuries in various studies
The use of different signs of minimal or minor aortic injury is misleading to radiologists and surgeons, as this may influence tactical decisions. Among the key features, most studies considered a “small” intimate flap, intraluminal thrombus, or intramural hematoma without any external contour abnormalities and with minimal or no periaortic hematoma as MPA (Figs. 4, 5). In most studies, an intimal flap was considered “small” if it measured less than 1 cm, as untreated intimal flaps or thrombi larger than 1 cm had a higher incidence of disease progression. .
Figure 4
Frontal (A) and sagittal (B) CT images of the chest of a 32-year-old man (jumped from the roof of a building). A tiny intraluminal thrombus (arrows) is identified in the aorta at the level of the isthmus, without external hematoma or irregular contour shape suggesting aortic damage.
Figure 5
Axial CT image of the chest in a 41-year-old man (fall from a motorcycle). A small intimal flap (indicated by a black arrow) is identified in the anterior descending thoracic aorta without external hematoma or deformation of the external contour, which corresponds to minimal damage to the aorta. We also see a fracture of the left rib (indicated by a white arrow) and bilateral accumulation of fluid in the pleural cavity.
As with the diagnosis of MPA, there is also no consensus regarding the management and monitoring of these injuries. Most studies suggest that they can be treated noninvasively by monitoring heart rate and blood pressure and anticoagulant or antiplatelet therapy. The choice of appropriate treatment strategy should be individualized, taking into account other concomitant diseases. The initial use of negative inotropes (most often beta-blockers) is suggested to achieve target blood pressure and heart rate values to reduce vascular shear stress—systolic blood pressure of 120 mmHg. Art. or an average blood pressure of 80 mm Hg. Art., as well as a heart rate less than 80 beats per minute. Second-line drugs are calcium channel blockers or arterial vasodilators. The Society of Vascular Surgery (SVS) guidelines suggest a “watchful waiting” approach with serial monitoring of the intimal condition.
Recent Eastern Association for the Surgery of Trauma (EAST) guidelines note that there is insufficient evidence to make recommendations for the conservative treatment of MPA, with more research needed. Even the SVS guidelines lack any specific recommendations on the “expected” course of the disease and follow-up protocol. Visual observation of MPA usually varies depending on the experience of each individual institution and its ongoing observations. Although a recent study from Harborview Medical Center by Heneghan et al. suggest that after conservative treatment of MPA there is no need for follow-up imaging, a previous study from the same institute in 2014, Gunn et al. suggested the use of CT angiography on day 3, 1 week, and 1 month after injury. In another study, Mosquera et al. recommended CT angiography at 1, 3, 6, and 12 months after injury, followed by annual cardiac and vascular MR scanning. Although there is no consensus regarding the timing of prophylactic testing, most investigators suggest that surveillance usually ends when the aorta returns to normal appearance. Almost all studies show that in most patients the disease does not progress, and if it does, it occurs within the first month after injury. This pattern of disease progression is also supported by experimental animal studies, which show that maximum intimal cellular activity and thickening occur 3–4 weeks after injury. If after this time there are signs of stabilization or improvement in the imaging appearance of the injury, further observation may not be necessary. Ultimately, there is a need for a prospective multicenter study using a “fixed” anatomical definition of “minor” aortic injury, in which a cohort of patients with MPA should be serially monitored with a predetermined CT frequency and duration of follow-up.
There are several different OTPA classification systems (Table 4). One of the most widely used OTPA assessments was proposed by Azizzadeh et al. (approved by the Society of Vascular Surgery) and divides injuries into 4 degrees: class 1 - intimal tears (Fig. 5), class 2 - intrathoracic hematoma or large intimal valve (Fig. 6), class 3 - pseudoaneurysm (Fig. 7, and 4 grade—free tear (Figure 9).Although this grading system provides a straightforward description of the injury, it is not a guide to treatment.
One of the most widely used OTPA assessments was proposed by Azizzadeh et al. (approved by the Society of Vascular Surgery) and divides injuries into 4 degrees: class 1 - intimal tears (Fig. 5), class 2 - intrathoracic hematoma or large intimal valve (Fig. 6), class 3 - pseudoaneurysm (Fig. 7, and 4 grade—free tear (Figure 9).Although this grading system provides a straightforward description of the injury, it is not a guide to treatment.
Table 4 | OTPA classifications
Figure 6
A 45-year-old man with blunt chest trauma. Axial (A), coronal (B) and sagittal (C) planes of CT angiography image. A PA is detected in the proximal descending aorta, causing an intramural hematoma in the area of the aortic arch, branches of the aortic arch (curved arrow in image C) and the descending thoracic aorta (white arrows) with thrombus (hollow arrows in images A and C).
Figure 7
A 63-year-old woman suffered as a result of a motorcycle injury. Axial (A) and sagittal (B) sections of CT scan of the chest. A small pseudoaneurysm (indicated by white arrows) is identified in the area of the aortic isthmus with a mediastinal hematoma (indicated by a hollow arrow).
Figure 8
Male, 33 years old, OTPA. Axial (A) and coronal (B) images of CT angiography with ECG synchronization. A pseudoaneurysm of the ascending thoracic aorta is visualized from the area above the sinotubular junction. The dimensions of the pseudoaneurysm are 1.4 x 0.7 cm. There are no signs of active contrast extravasation. An open arrow indicates slight bleeding from mediastinal fat.
Figure 9
A 70-year-old woman with a traumatic aortic rupture. Axial (A) and coronal (B) CT images. There are signs of complete rupture of the anterior wall of the descending thoracic aorta (indicated by an arrow), causing extravasation of contrast material (indicated by an asterisk). Note the mediastinal hematoma and bilateral fluid collections in the pleural cavities.
There are many treatment options for a patient with OTPA, such as traditional open surgery, endovascular stenting, and the choice of conservative management for some groups of patients. Thus, evaluation of CT angiography of the OTPA is highly valuable for treatment planning. In addition to information about the severity and type of injury, CT findings should include a description of the aortic arch anatomy, signs of vertebral artery dominance, any significant pre-existing atherosclerotic disease or stenosis, previous postoperative changes (such as coronary artery bypass graft), length of aortic injury, greater aortic diameter and below the injury, as well as the proximity of the left subclavian artery (in case of injury to the aortic isthmus). This information helps the doctor choose treatment options and type of surgery. For example, surgical repair of the aorta typically involves a left posterolateral thoracotomy, often requiring the patient to be placed on a heart-lung machine. Imaging helps the surgeon determine the exact area of injury and provides information about other injuries that can be treated using the same approach.
A few additional important radiological findings to consider when planning endovascular stenting are the presence of any focal lesion or thrombus, information about the proximal and distal stent site (preferred length is 2 cm), the presence of calcification in the stent site, aortic tortuosity and diameter of access vessels.
There are differing opinions regarding the best management option for patients with this type of injury. Studies have shown that the increased use of endovascular stents among patients requiring surgical treatment has led to a decrease in the incidence of early complications and shorter hospital stays. Recent EAST guidelines recommend the use of endovascular grafting in patients who have no contraindications to the procedure.
The guidelines also suggest that in hemodynamically stable patients, definitive treatment with OTPA should be delayed until other acute life-threatening injuries have resolved. Early treatment with OTPA may be associated with a higher incidence of paraplegia and renal failure. But if the patient is hemodynamically unstable and there is direct evidence of aortic injury on CT, urgent treatment of the aortic injury is necessary. The proposed management algorithm for OTPA in patients with blunt trauma, based on the recommendations of the EAST Practice Work Group, is shown in Table 5.
Table 5 | Tactics for OTPA, based on the recommendations of the Eastern Association of Surgeons and Traumatologists (EAST practice work group)
Analysis of a national inpatient sample by Ultee et al. showed that treatment using endovascular methods (TEVAR - thoracic endovascular aortic repair) increased from 6.5% of surgical volume in 2005 to 87% in 2011. Overall mortality from aortic trauma has also decreased, due to the use of TEVAR, expanded indications for use, improved surgeon skills, and increased technical capabilities. Aortic injury, relatively common in younger age groups, presents many unique challenges related to its management and outcome. The average aortic size in this population is much smaller than in aneurysmal disease, and therefore early experience with endovascular aortic repair (EVAR) encountered problems in determining graft size. The arch geometry in younger patients is also more acute, which is associated with poor compatibility of the endograft with the aortic arch. A 0–18% rate of infolding, migration, stent collapse, and even acute aortic occlusion requiring reintervention has been reported, with most complications occurring early after surgery. Aortic remodeling in these patients may also differ in that the aorta distal to the left subclavian artery dilates at a faster rate than the proximal segments. In addition to technical advances, the use of procedural modifications, such as limiting excess graft size to 10% to accommodate subsequent remodeling, has been proposed. The influence of these factors on long-term results requires further study.
With hybrid operating rooms becoming more common, parallel advances in imaging such as cone beam CT, fusion imaging, and intravessel ultrasound (IVUS) are also facilitating operative and interventional procedures by minimizing radiation exposure and use of contrast agents. This, along with better image quality, is critical to the technical success of complex endovascular aortic procedures. Better planning software and fusion visualization are helpful for accurate graft deployment and this can be further confirmed by IVUS. The use of IVUS in aortic procedures improves understanding of complex anatomy and has been shown to reduce the amount of contrast used and overall operative time.
The patient with blunt trauma requires a multidisciplinary approach to treatment. Because OTPA is a life-threatening condition with almost always unpredictable outcomes, multidisciplinary teams are needed to rapidly assess, triage, and manage patients suspected of having OTPA (based on physical examination, external or CT findings, or known prior history). This group includes specialists in cardiovascular imaging, interventional radiology, cardiac surgery, vascular and endovascular surgery, cardiology, and anesthesiology and resuscitation. The team should provide expert judgment for all acute situations and discuss various options for approaches to the treatment of OTPA, including the use of endovascular techniques, minimally invasive and open surgery. In the researchers' experience, it is the interdisciplinary team approach to the management of patients with OTPA that is critical for appropriate treatment.
Sources:
- Fox N, Schwartz D, Salazar JH, et al. Evaluation and management of blunt traumatic aortic injury: a practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2015;78(1):136–46.
- Neschis DG, Scalea TM, Flinn WR, Griffith BP. Blunt aortic injury. N Engl J Med. 2008;359(16):1708–16.
- Heneghan RE, Aarabi S, Quiroga E, Gunn ML, Singh N, Starnes BW. Call for a new classification system and treatment strategy in blunt aortic injury. J Vasc Surg. 2016;64(1):171–6.
- Ungar TC, Wolf SJ, Haukoos JS, Dyer DS, Moore EE. Derivation of a clinical decision rule to exclude thoracic aortic imaging in patients with blunt chest trauma after motor vehicle collisions. J Trauma. 2006;61(5):1150–5.
- Steenburg SD, Ravenel JG, Ikonomidis JS, Schonholz C, Reeves S. Acute traumatic aortic injury: imaging evaluation and management. Radiology. 2008;248(3):748–62.
- Nagpal P, Khandelwal A, Saboo SS, Bathla G, Steigner ML, Rybicki FJ. Modern imaging techniques: applications in the management of acute aortic pathologies. Postgrad Med J 1078;2015(91):449–62.
- Seimens Healthineers USA
- Starnes BW, Lundgren RS, Gunn M, et al. A new classification scheme for treating blunt aortic injury. J Vasc Surg. 2012;55(1): 47–54.123
- Lamarche Y, Berger FH, Nicolaou S, et al. Vancouver simplified grading system with computed tomographic angiography for blunt aortic injury. J Thorac Cardiovasc Surg 2012;144(2):347–54.
- Rogalla P, Kloeters C, Hein PA. CT technology overview: 64-slice and beyond. Radiol Clin North Am. 2009;47(1):1–11.
- Voitle E, Hofmann W, Cejna M. Aortic emergencies-diagnosis and treatment: a pictorial review. Insights Imaging. 2015;6(1):17–32.
- Nagpal P, Saboo SS, Khandelwal A, Duran-Mendicuti MA, Abbara S, Steigner ML. Traumatic right atrial pseudoaneurysm. Cardiovasc Diagnosis Ther. 2015;5(2):141–4.
- Soto JA, Anderson SW. Multidetector CT of blunt abdominal trauma. Radiology. 2012;265(3):678–93.
- Fishman EK, Ney DR, Heath DG, Corl FM, Horton KM, Johnson PT. Volume rendering versus maximum intensity projection in CT angiography: what works best, when, and why. Radiographics. 2006;26(3):905–22.
- Sammer M, Wang E, Blackmore CC, Burdick TR, Hollingworth W. Indeterminate CT angiography in blunt thoracic trauma: is CT angiography enough? AJR Am J Roentgenol. 2007;189(3):603–8.
- Fabian TC, Richardson JD, Croce MA, et al. Prospective study of blunt aortic injury: Multicenter Trial of the American Association for the Surgery of Trauma. J Trauma.1997;42(3):374–80 (discussion 80–83).
- Kram HB, Appel PL, Wohlmuth DA, Shoemaker WC. Diagnosis of traumatic thoracic aortic rupture: a 10-year retrospective analysis. Ann Thorac Surg. 1989;47(2):282–6.
- Gavant ML. Helical CT grading of traumatic aortic injuries. Impact on clinical guidelines for medical and surgical management. Radiol Clin North Am. 1999;37(3):553–74.
- Malhotra AK, Fabian TC, Croce MA, Weiman DS, Gavant ML, Pate JW. Minimal aortic injury: a lesion associated with advanced diagnostic techniques. J Trauma.2001;51(6):1042–8.
- Forman MJ, Mirvis SE, Hollander DS. Blunt thoracic aortic injuries: CT characterization and treatment outcomes of minor injury. Eur Radiol. 2013;23(11):2988–95.
- Gunn ML, Lehnert BE, Lungren RS, et al. Minimal aortic injury of the thoracic aorta: imaging appearances and outcome. Emerg Radiol. 2014;21(3):227–33.
- Paul JS, Neideen T, Tutton S, et al. Minimal aortic injury after blunt trauma: selective nonoperative management is safe. J Trauma. 2011;71(6):1519–23.
- de Mestral C, Dueck A, Sharma SS, et al. Evolution of the incidence, management, and mortality of blunt thoracic aortic injury: a population-based analysis. J Am Coll Surg. 2013;216(6):1110–5.
- Osgood MJ, Heck JM, Rellinger EJ, et al. Natural history of grade I–II blunt traumatic aortic injury. J Vasc Surg. 2014;59(2):334–41.
- Kidane B, Abramowitz D, Harris JR, DeRose G, Forbes TL. Natural history of minimal aortic injury following blunt thoracic aortic trauma. Can J Surg Journal canadien de chirurgie.2012;55(6):377–81.
- Mosquera VX, Marini M, Lopez-Perez JM, et al. Role of conservative management in traumatic aortic injury: comparison of long-term results of conservative, surgical, and endovascular treatment. J Thorac Cardiovasc Surg. 2011;142(3):614–21.
- Erbel R, Aboyans V, Boileau C, et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur Heart J 2014;35(41):2873–926.
- Lee WA, Matsumura JS, Mitchell RS, et al. Endovascular repair of traumatic thoracic aortic injury: clinical practice guidelines of the Society for Vascular Surgery. J Vasc Surg. 2011;53(1):187–92.
- Neville RF, Padberg FT Jr, DeFouw D, Hernandez J, Duran W, Hobson RW 2nd. The arterial wall response to intimal injury in an experimental model. Ann Vasc Surg 1992;6(1):50–4.
- Azizzadeh A, Keyhani K, Miller CC 3rd, Coogan SM, Safi HJ, Estrera AL. Blunt traumatic aortic injury: initial experience with endovascular repair. J Vasc Surg. 2009;49(6):1403–8.
- Forcillo J, Philie M, Ojanguren A, et al. Outcomes of traumatic aortic injury in a primary open surgical approach paradigm. Trauma Mon. 2015;20(2):e18198.
- Fanelli F, Dake MD. Standard of practice for the endovascular treatment of thoracic aortic aneurysms and type B dissections. Cardiovasc Intervent Radiol. 2009;32(5):849–60.
- Ultee KH, Soden PA, Chien V, et al. National trends in utilization and outcome of thoracic endovascular aortic repair for traumatic thoracic aortic injuries. J Vasc Surg.2016;63(5):1232–9.
- Forbes TL, Harris JR, Lawlor DK, Derose G. Aortic dilatation after endovascular repair of blunt traumatic thoracic aortic injuries. J Vasc Surg. 2010;52(1):45–8.
- Farber MA, Mendes RR. Endovascular repair of blunt thoracic aortic injury: techniques and tips. J Vasc Surg. 2009;50(3):683–6. 36. Kolbel T, Dias N, Resch T, Holst J, Sonesson B, Malina M. In situ bending of thoracic stent grafts: clinical application of a novel technique to improve conformance to the aortic arch.
- J Vasc Surg. 2009;49(6):1613–6.
- Neschis DG, Moainie S, Flinn WR, Scalea TM, Bartlett ST, Griffith BP. Endograft repair of traumatic aortic injury—a technology in evolution: a single institution's experience. Ann Surg. 2009;250(3):377–82.
- Stangenberg L, Shuja F, Carelsen B, Elenbaas T, Wyers MC, Schermerhorn ML. A novel tool for three-dimensional roadmap- ping reduces radiation exposure and contrast agent dose in complex endovascular interventions. J Vasc Surg. 2015;62(2):448–55.
- Song TK, Donayre CE, Kopchok GE, White RA. Intravascular ultrasound use in the treatment of thoracoabdominal dissections, aneurysms, and transections. Semin Vasc Surg. 2006;19(3):145–9.
- Guo BL, Shi ZY, Guo DQ, et al. Effect of intravascular ultrasound-assisted thoracic endovascular aortic repair for ''complicated'' type B aortic dissection. Chin Med J (Engl). 2015;128(17):2322–9.
- Dijkstra ML, Eagleton MJ, Greenberg RK, Mastracci T, Hernandez A. Intraoperative C-arm cone-beam computed tomography in fenestrated/branched aortic endografting. J Vasc Surg. 2011;53(3):583–90.
- Bashore TM, Bates ER, Berger PB, et al. American College of Cardiology/Society for Cardiac Angiography and Interventions Clinical Expert Consensus Document on cardiac catheterization laboratory standards. A report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2001;37(8):2170–214.
- Alberta HB, Secor JL, Smits TC, et al. Comparison of thoracic aortic diameter changes after endograft placement in patients with traumatic and aneurysmal disease. J Vasc Surg. 2014;59(5):1241–6.
- Watson J, Slaiby J, Garcia Toca M, Marcaccio EJ Jr, Chong TT. A 14-year experience with blunt thoracic aortic injury. J Vasc Surg. 2013;58(2):380–5.
- Fearn S, Lawrence-Brown MM, Semmens JB, Hartley D. Follow-up after endovascular aortic aneurysm repair: the plain radiograph has an essential role in surveillance. J Endovasc Ther. 2003;10(5):894–901.
- Riesenman PJ, Brooks JD, Farber MA. Acute blunt traumatic injury to the descending thoracic aorta. J Vasc Surg. 2012;56(5):1274–80. 47. Estrera AL, Miller CC 3rd, Guajardo-Salinas G, et al. Update on blunt thoracic aortic injury: fifteen-year single-institution experience. J Thorac Cardiovasc Surg. 2013;145(3 Suppl):S154–8. 48. Rabin J, DuBose J, Sliker CW, O'Connor JV, Scalea TM, Griffith BP. Parameters for successful nonoperative management of traumatic aortic injury. J Thorac Cardiovasc Surg. 2014;147(1):143–9.
Clinical manifestations
Many variants of localization and extent of dissection, the possibility of occlusion of various branches of the aorta give such a variety of clinical manifestations that they make their systematization quite difficult. The most typical symptoms are:
• sharp pain, most intense at the moment of occurrence, more often - behind the sternum, in the heart area, less often - in the interscapular region, epigastrium, lower back;
• motor excitement;
• shortness of breath;
• pale or bluish skin;
• increased blood pressure (higher values are typical for a low location of the dissection);
• hypotension (often the result of cardiac tamponade and aortic valve insufficiency);
• loss of consciousness;
• arrhythmia;
• pulse asymmetry;
• transient disturbances of sensitivity and movements in the limbs;
• visual and speech disorders.
Prognosis after aortic replacement
The immediate postoperative period usually takes 10-14 days and depends on the immediate results of the operation. Within 1-3 days, patients require intensive care, and prolonged artificial ventilation is possible. We usually start lifting patients on the 3rd day after the intervention. We are allowed to walk by 5 days. If the postoperative period proceeds smoothly, the patient is discharged home on the 10th day.
After discharge, you must wear a special bandage on your stomach for a month. A month later, a control ultrasound scan is performed to assess the patency of the artificial prosthesis and the state of blood flow in the legs.
After open aortic surgery, the patient returns to normal daily activities after 3-6 months. The patency of vascular grafts is maintained at 93% over a five-year period after surgery. Ultrasound monitoring allows you to identify possible developments of problems and take timely measures to eliminate them.
Treatment
Aortic dissection requires prompt transfer of the patient to the vascular surgery department. Equipping with high-tech equipment and the qualifications of our specialists allow us to provide the necessary assistance at the proper level and in full compliance with modern standards.
An emergency operation is performed on a dissection affecting the ascending part and the arch. The duration of the disease is not taken into account in this case - the risk of complications is too high. The same tactics are also required by the pathology of the descending section, when the possibility of further detachment of the vascular wall is real. If there is no direct threat to life, the operation can be delayed.
Severe concomitant pathology forces patients to be treated conservatively. It should be noted that, nevertheless, the most effective method of treatment is surgical .
The essence of the operation is to eliminate the false passage and replace the affected area with a synthetic prosthesis, and, if necessary, restore the function of the aortic valve.
Definition
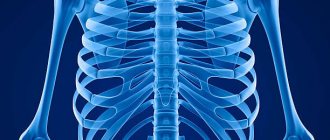
A thoracic aortic aneurysm is a condition that occurs when the walls of the top of your body's main artery (aorta) become weakened and bulging.
A thoracic aortic aneurysm is a weakened and bulging area at the top of the aorta, the main blood vessel that carries blood to different parts of your body. The aorta, which is approximately the thickness of a garden hose, runs from the heart through the center of the chest and abdomen. Aneurysms form anywhere along the aorta, which runs from the heart through the abdomen. When they occur in the upper part of the aorta, they are called thoracic aortic aneurysms. Most often, aneurysms form in the lower part of the aorta and are called abdominal aortic aneurysms. In rare cases, an aneurysm develops in both the upper and lower parts of the aorta. This type of aneurysm is called a thoracoabdominal aneurysm.
Because the aorta carries blood to various parts of the body, rupture can cause life-threatening bleeding. Most small, slow-growing thoracic aortic aneurysms do not rupture, but large, rapidly growing aneurysms are at very high risk of rupture. Depending on the size and growth rate of the thoracic aortic aneurysm, treatment may range from watchful waiting to emergency surgery. If a thoracic aortic aneurysm is identified, doctors will closely monitor its condition to plan surgery if necessary. Emergency surgery for a ruptured thoracic aortic aneurysm is very risky.
Description
The aorta is one of the large human vessels through which oxygenated arterial blood from the left ventricle flows to all organs and tissues, with the exception of the lungs. Since the walls of the aorta, even normally, constantly experience blood pressure with an average value of 100 mm Hg. Art., when exposed to various pathological factors, the structure of the vessel may be disrupted.
The aortic wall consists of three layers, which from the middle outwards have the corresponding names - intima, media and adventitia.
At the very beginning, only the intima is damaged. The pathological formation may be completely insignificant, but due to the high pressure in the vessel, the intima is gradually destroyed and when the damage reaches the medial layer, blood begins to spread in the middle layer of the vessel, promoting its delamination. If medical assistance is not provided at this stage, complete rupture of the aorta and instant death of the patient may occur.
There are different types of aortic dissection, which differ in the location of the dissection. At Stanford University in 1970, they proposed dividing DA into two types:
- Type A - the dissection begins in the area of the ascending aorta, which either remains in the same area or extends to the arch and descending part of the vessel.
- Type B - the dissection is located only along the descending aorta (from the subclavian artery and below), but can also extend to the abdominal part of the vessel.
Understanding the differences between these two types is extremely important because it allows for more effective treatment of the disease. Type A requires immediate surgery to prevent death from stroke, heart attack, congestive heart failure or bleeding. Type B dissection is considered a non-urgent condition that can initially be treated with increased blood pressure control. Additional procedures usually complement the protection of the patient from complications arising from the rupture.
Symptoms
The classic triad of signs makes it possible to establish a diagnosis. If all three symptoms are present, there is a 100% probability. If there are only some manifestations, then they speak of a greater or lesser probability.
- Severe, abrupt onset of tearing or tearing pain in the chest, which may radiate to the back.
- Deficiency or difference in pulse rate in the upper extremities; different blood pressure > 20 mmHg may also be detected.
- Mediastinal widening on chest x-ray.
Additionally, patients often feel as if they are having a heart attack. The following symptoms may also be observed:
- Inability to take a comfortable position.
- Extremely high blood pressure.
- Loss of consciousness.
- Hesitant breathing.
- Feeling very weak.
- Feeling of doom (extreme anxiety).