Subcutaneous emphysema - causes, symptoms, treatment of air bubbles under the skin
Contents
hide
1 Subcutaneous emphysema - causes, symptoms, treatment of air bubbles under the skin
2 What is emphysema?
3 What are the causes of subcutaneous pneumothorax?
4 Symptoms of subcutaneous pneumothorax - how to recognize air under the skin?
5 Treatment of pneumothorax - how to get rid of air bubbles? 5.1 Related posts:
Subcutaneous emphysema is a condition in which air bubbles are visible under the skin. Typically, subcutaneous emphysema is located on the chest, neck or face. The cause is trauma in these areas, medical procedures (for example, after laparoscopy, tracheotomy) or dental procedures (for example, after tooth extraction). Symptoms of pneumothorax include pain and fullness in the neck and difficulty breathing. Treatment for subcutaneous pneumothorax is usually not required because the air is self-absorbed.
Fotolia
What is emphysema?
Subcutaneous emphysema is the presence of air in the subcutaneous tissue. There are many reasons for its occurrence. It often coexists with mediastinal pneumothorax (air in the mediastinum) or pneumothorax (air in the pleural cavity), where air passes under the skin of the neck.
The most important causes of subcutaneous pneumothorax:
- perforation of the gastrointestinal tract,
- chest injury
- trauma to the structures of the respiratory tract (larynx, trachea, bronchi),
- complication of medical procedures,
- soft tissue infection (gas gangrene).
Subcutaneous pneumothorax in newborns, on the contrary, can occur after a difficult birth.
What are the causes of subcutaneous pneumothorax?
Subcutaneous emphysema can occur as a result of trauma to the chest, such as during a traffic accident. In this case, the cell walls (ribs) and lung parenchyma are often damaged. Trauma causes air to enter the pleural cavity or mediastinum. From here, the air penetrates the soft tissues in search of an outlet, causing hypodermis on the neck and swelling of the face.
Subcutaneous pneumothorax can also be caused by rib fractures caused by trauma or intense, prolonged coughing (for example, during an asthma attack). According to statistics, every fourth patient with a rib fracture suffers from comorbid hypodermia.
About
Diagnostics
Diagnostic measures are carried out by a pulmonologist. In case of traumatic genesis of the symptom, the participation of a traumatologist is required; in case of facial lesions, consultation with a maxillofacial surgeon is necessary. During the collection of anamnesis, the specialist finds out what happened in the period preceding the formation of emphysema, identifies other complaints, and assesses the dynamics of the development of the disease. The following procedures are carried out:
- Visual inspection
. The presence of subcutaneous accumulation of air is indicated by an uneven increase in the volume of soft tissues, sometimes creating the impression of “bloat”. Palpation is painless, a gentle crunch is detected by palpation. Possible lag of half of the chest in the act of breathing, expansion of the saphenous veins, and forced positioning of the patient. - Radiography
. In case of pathologies of the OGK, an overview photograph must be taken, and optionally a targeted one. It is possible to detect rib fractures, hemo- and pneumothorax, pneumomediastinum. For facial injuries, radiographs of the orbit, nasal bones, and zygomatic bone are taken. Sometimes an X-ray of the skull is required to rule out fractures of the brain. - CT scan
. CT of the OGK is performed to clarify the nature of the damage, identify atelectasis, pneumo- and hemothorax, and other pathologies, and is performed natively or with contrast. Patients may also have a CT scan of the lungs or a CT scan of the mediastinum. To detail the changes detected on X-rays of the facial bones, CT scans of the orbit and other studies may be prescribed. - Magnetic resonance imaging
. MRI of the lungs is informative in distinguishing between inflammatory and non-inflammatory lesions, studying lung tissue, vascular structures, the lymphatic system and fluid accumulations. Performed at the final stage of the examination as part of differential diagnosis and planning of thoracic interventions. - Endoscopic methods
. Suspicion of esophageal perforation is an indication for esophagoscopy. Tracheobronchoscopy is performed for tracheal perforation, bronchial fistulas, and other pathologies. In some cases, thoracoscopy is necessary to clarify the diagnosis and carry out treatment measures. - Other techniques
. Scintigraphy is recommended for assessing capillary blood flow and pulmonary ventilation; it is used for atelectasis, pneumonia, and obstructive pathologies. Pleural puncture allows you to determine the nature and amount of exudate in pleurisy, hemothorax and hydrothorax.
Subcutaneous emphysema on x-ray
Symptoms of subcutaneous pneumothorax - how to recognize air under the skin?
Patients with pneumothorax complain of the sensation of air bubbles under the skin. Feeling of severe discomfort in the neck and chest. Additionally there may be:
- breathing problems,
- difficulty swallowing and speaking
- change in voice timbre,
- feeling of fullness in the neck.
Patients complain of sore throat, wheezing, or neck pain. The tissue around the pneumothorax may be slightly swollen. On examination, a squeaking sound of the skin when touched is characteristic of subcutaneous pneumothorax.
About
Mediastinal emphysema, or pneumomediastinum, is a pathological condition consisting of air infiltration of mediastinal tissue [4].
It is believed that spontaneous mediastinal emphysema (SEM) is a rare, independent disease characterized by a benign course and occurring without specific causes; it affects mainly young men [9, 19, 23, 36].
The first mention of SES dates back to 1617, when the midwife of the Queen of France, Louise Bourgeois, in her memoirs described the sudden swelling of her neck during childbirth [12]. This pathological condition was first described by Rene Laennec in 1819 in his treatise “On Listening with a Stethoscope” [24]. SES as an independent disease was first reported by Louis Hamman [5, 10, 19, 23, 25] in 1939. He described rough crepitus, synchronous with heartbeats, which is auscultated along the left edge of the sternum in the third to sixth intercostal spaces, not excluding and other areas in a sitting position. This clinical symptom is called Hamman's symptom.
The pathophysiology of this disease, based on experiments on laboratory animals, was described in 1944 by M. Macklin and S. Macklin [5, 10, 23, 25]. In an experiment on animals, they showed that SES occurs as a result of a sharp decrease in the pressure gradient between the alveoli and the interstitial tissue of the lungs, which leads to rupture of the alveoli. The described mechanism, in combination with pathological changes in the alveolar-capillary membrane and/or interstitial tissue of the lungs, can lead to a breakthrough of the alveoli into the interstitial space [31]. Breakthrough of the alveoli into the pulmonary interstitium leads to the accumulation of air in it, which spreads along the pressure gradient, perivascular and peribronchial, centripetally to the hilum of the lungs, and then into the mediastinum (Macklin effect) [20]. This occurs because the pressure in the mediastinum is lower than in the periphery of the lungs. Most authors agree that the disease occurs as a result of rupture of the terminal alveoli located at the root of the segment (lobe) of the lung and adjacent to the loose tissue surrounding the vessels and bronchi [5, 16, 23]. Once in the mediastinum, the air can spread to the cellular spaces of the neck, soft tissues of the chest, into the cavity of the cardiac membrane, and even (depending on the amount) into the retroperitoneal cellular space [8].
The frequency of SES in hospitalized patients varies, according to various sources, from 1:3578 [16] to 1:44,511[25].
There are different trigger mechanisms or factors that contribute to the occurrence of SES. I. Macia et al. [25] consider it advisable to divide these factors into: predisposing - bad habits and/or diseases in history that create conditions favorable for the development of the disease, and provoking - conditions that immediately precede the onset of SES.
Many authors include pulmonary diseases such as bronchial asthma [5, 9, 16, 19, 25, 29], inflammatory diseases of the upper respiratory tract [5, 19], idiopathic fibrosing pulmonary diseases [9], chronic obstructive pulmonary diseases as predisposing factors. [9]. Of the diseases listed above, according to publications in the world literature, only bronchial asthma is considered as a predisposing factor in the development of SES by almost all authors [5, 9, 16, 19, 25, 29, 35, 36]. J. Chapdelaine et al. [11] established a history of this disease in almost 50% of patients, A. Newcomb and C. Clarke [29] - in 39% of patients with SES. It should be noted that in the world literature, authors rarely associate the development of SES with bullous pulmonary emphysema. A.G. Vysotsky [2] described 4 cases of pneumomediastinum as a complication of local bullous emphysema. I.I. Platov and V.S. Moiseev [4] believe that the development of SES is associated with the same reasons that lead to the development of spontaneous pneumothorax, namely bullous disease, cystic lung formations of congenital origin, and respiratory inflammatory diseases.
Some authors believe that smoking is a predisposing factor in the development of the disease [9, 25]. J. Macia et al. [25] compared the number of smokers with SES with the number of smokers among the population of Catalonia (Spain), which was 34.1 and 37.5%, respectively. I. Abolnik et al. [6] noted that the number of smokers among patients with SES differed slightly from those in the general population.
Many provoking factors have been described that can directly cause the development of the disease. It is worth highlighting the Valsalva maneuver, intense coughing, sneezing, severe vomiting, hysterical screaming, childbirth, defecation, physical activity, bronchospasm, spirometry, playing wind instruments, blowing up balloons, using inhaled drugs [1, 5, 9, 10, 18 , 23, 25, 26, 28, 32].
In a report by M. Caceres et al. [9] the dominant among the provoking factors was vomiting, which preceded the onset of the disease in 36% of cases; the second most common factor was an attack of bronchial asthma; this condition was observed in 21% of patients. Cough is also one of the common trigger factors, and according to various sources, it precedes SES in 7.3% [25] and in 40% of cases [28]. The occurrence of SES due to diabetic ketoacidosis [36], chemotherapy [34], and Hodgkin's disease [21] has also been described.
However, it is not always possible to identify predisposing and/or provoking factors; SES often occurs at rest [9].
The variety of symptoms in the clinical manifestation of SES has been reported by many authors [25, 36]. The most common triad of clinical symptoms is chest pain (which is the most common and constant symptom), difficulty breathing, and puffiness of the neck [1, 5, 15, 16, 19, 25, 29, 35, 36]. I. Abolnik et al. [6] noted the presence of chest pain in 88% of patients with SES, I. Macia et al. [25] - in 85%, M. Gerazounis et al. [16] - in 72.7%, G. Koullias et al. [23] - in 66.6%, M. Caceres et al. [9] - in 54% of patients. The patient may also complain of pain in the throat, back, shoulder, lower back, weakness, dysphagia, odynophagia, rhinophonia, and change in voice timbre. Some authors include cough as a symptom of the disease, although it is also a factor provoking the occurrence of SES [23]. M. Caceres et al. and G. Koullias et al. identified cough as one of the symptoms of the disease; it was noted in 41 and 32% of SES’s own observations and was, respectively, the second and third most common symptom after chest pain [9, 23].
Of the clinical symptoms of the disease identified during physical examination, subcutaneous emphysema of the soft tissues of the neck and/or chest is most often noted [1, 2, 5, 7, 16, 25, 36]. Depending on the amount of air entering the mediastinal tissue, soft tissue emphysema can spread to the face and lower chest, but this is rare [5]. In a report by I. Macia et al. [25] in 95% of patients with SES, subcutaneous emphysema of soft tissues was determined by palpation, in 66% of patients - in the neck, and in 29% of patients - in the chest wall. J. Jougon et al. [19] stated the presence of this symptom in 100% of patients with SES. M. Gerazounis et al. [16] described the presence of rhinophony (nasal tone) in 5 patients, which was noted together with emphysema of the soft tissues of the neck and developed as a result of dissection of the tissues of the retropharyngeal cellular space with air. This symptom is quite rare, but there are observations in which it serves as the first manifestation of SES and the main clinical symptom of the disease [17].
Hamman's symptom cannot be called specific for SES, since, according to Yu.V. Haleva [5], such crepitus can be heard in left-sided pneumothorax without mediastinal emphysema, as well as in bullous emphysema of the lingular segments, pneumoperitoneum with a high diaphragm, and gastric dilatation. The prevalence of Hamman's symptom in patients with SES, according to various sources, varies from 0 to 56% [6, 9, 10, 15, 23, 25, 29, 36].
With pneumomediastinum, patients may also experience a decrease in cardiac dullness and deafness of heart sounds during auscultation. I. Abolnik et al. [6] in 2 patients with SES the presence of paradoxical pulsus was noted. Most patients may have one or more symptoms, but sometimes objective examination fails to identify any symptoms [5].
The main methods for diagnosing SES are chest x-ray in frontal and lateral projections, breast CT and x-ray contrast examination of the esophagus.
A. Yellin et al. [36] indicated the need to perform radiography (as a routine method of primary diagnosis) in all young patients with chest pain of unknown origin and difficulty breathing. According to many authors, this research method turned out to be informative in the vast majority of patients with SES [6, 16, 23, 36], while they emphasize the need to perform the study in two projections - frontal and lateral, because with a small accumulation of gas in the mediastinum during survey X-ray of the chest in a direct projection may not reveal pneumomediastinum [23, 25].
When pneumomediastinum occurs, x-rays reveal clear bands or gas bubbles surrounding the mediastinal organs, elevating the mediastinal pleura and often extending to the neck and/or chest wall [14].
S. Bejvan and J. Godwin [8] report that with AP radiography, free gas in the mediastinum is often detected along the left contour of the heart and covers the inner surface of the mediastinal pleura, creating a clearly visible pleural line lateral to the pulmonary trunk and aortic arch. On radiographs in the lateral projection, free gas forms lines of clearing along the contours of the ascending aorta, the aortic arch and its branches, the pulmonary arteries and the trachea with the main bronchi [8]. Gas is also localized along the line of attachment of the diaphragm to the sternum, along the thymus gland and brachiocephalic veins [13].
Polypositional radiography is the main and very effective research method for this disease, but if there is gas infiltration of the soft tissues of the chest wall, then its information content is reduced to almost zero. In such situations, as well as in case of suspicion in relation to diseases with a similar clinical picture and if it is necessary to establish the cause of the disease, if the X-ray method is insufficient, it is advisable to perform a breast CT scan [30]. T. Kaneki et al. [20] noted that in 30% of patients with SES, radiography failed to detect pneumomediastinum; the final diagnosis was made by chest CT. G. Koullias et al. [23] performed CT after an initial X-ray examination in all 25 patients, although they considered X-ray the “gold standard” for diagnosing SES, since both of these diagnostic methods turned out to be informative regarding pneumomediastinum in 100% of cases. CT is undoubtedly the most effective method for diagnosing pneumomediastinum [20], since with its help the presence of gas in the mediastinum is easily detected and its anatomical localization is well determined in cross sections. However, it should be noted that in terms of ease of implementation and radiation exposure to the patient, this method is inferior to radiography; we should also not forget about the economic aspect. A. Newcomb and C. Clarke [29] believe that if pneumomediastinum is determined using radiography and there is no suspicion of the presence of any serious disease as the cause of this pathological condition, then we can limit ourselves to only this diagnostic method.
In some cases of SES reported in the world literature, X-ray contrast examination of the esophagus was performed. This additional diagnostic method was used in situations where it was necessary to exclude the presence of such a dangerous condition as esophageal rupture. A water-soluble contrast agent and/or barium sulfate suspension is used [15, 16, 19, 36]. D. Weissberg [35] used this research method to exclude esophageal rupture if the occurrence of SES was preceded by vomiting.
Additional research methods for this disease include esophagoscopy, bronchoscopy and electrocardiography. These methods are auxiliary and are used to confirm the diagnosis of SES in doubtful situations.
Differential diagnosis of SES is carried out with diseases of the cardiovascular (acute coronary syndrome, pericarditis), respiratory (spontaneous pneumothorax, pulmonary embolism, perforation of the tracheobroncheal tree) and digestive (spontaneous rupture of the esophagus) systems [32].
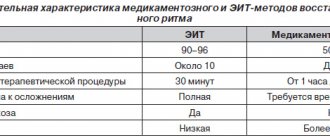
According to foreign authors [15, 25, 29, 35, 36], the optimal period of inpatient observation and treatment of patients with SES ranges from 2 to 5 days.
SES responds well to conservative treatment, which includes bed rest, analgesia and oxygen therapy [6, 9, 15, 23, 29]. In this case, a fairly rapid regression of symptoms is observed and in most cases complete resolution of pneumomediastinum occurs by the 8th day [29, 36]. Usually, soon after the alveoli break into the pulmonary interstitium, they collapse, as the pressure in them decreases and the flow of air stops [19]. G. Koullias et al. [23] all patients received antibacterial prophylaxis for mediastinitis. They used third-generation cephalosporins with the addition of clindamycin to therapy for suspected esophageal perforation and when the disease was accompanied by fever and leukocytosis. Very rarely, emphysema of the tissue of the neck, chest and abdominal walls, and face progresses and tense pneumomediastinum develops. In this case, the mediastinum, according to Sauerbruch, “swells up like a ball”, the thin-walled main veins of the mediastinum are compressed with a drop in cardiac activity, respiratory failure and possible death [3]. In such situations, an upper mediastinotomy according to Tiegel is indicated with tunnelization of the pretracheal fat to the level of the tracheal bifurcation with drainage of the mediastinum and subsequent aspiration, which ensures decompression of the mediastinum [4]. J. Moore et al. [27] in infants with tense mediastinal emphysema, mediastinal drainage was performed through a subxiphoid approach. For decompression of soft tissues and the mediastinum in this complication, some authors propose suprasternal puncture of the mediastinum and sternotomy [33], puncture of the supraclavicular areas [6] and tracheostomy [22]. If, despite these measures, an increase in tense mediastinal emphysema is observed, an urgent transpleural wide mediastinotomy is required [4].
Isolated observations of relapse of SES have been described [16, 25]. A. Yellin et al. were the first to describe relapse of the disease in the literature. [36], they observed patients for 52 months after discharge from the hospital; the recurrence of mediastinal emphysema in one patient occurred 14 months after the first episode without predisposing causes.
Thus, spontaneous mediastinal emphysema is a disease that most often affects young men of working age. Its occurrence requires differential diagnosis with a number of serious pathological conditions. In rare situations, tension mediastinal emphysema can lead to hemodynamic and respiratory compromise.
Treatment of pneumothorax - how to get rid of air bubbles?
Subcutaneous emphysema is suspected in patients with a characteristic history (eg, chest trauma, medical procedures) and typical cracking of the subcutaneous tissue. In addition, the diagnosis is made after an x-ray, which shows the presence of air under the skin. Patients are often accompanied by radiographic evidence of pneumothorax, mediastinal pneumonia, or esophageal perforation.
The course of pneumothorax is usually mild. In most cases, treatment for subcutaneous pneumothorax is not necessary, and the residual air is absorbed spontaneously over time. If the volume of air under the skin is large and results in a massive pneumothorax causing severe discomfort to the patient, the doctor may decide to drain it.
If the cause of pneumothorax is perforation of the esophagus or rupture and damage to the airway, prompt surgical intervention is required. Patients with subcutaneous emphysema should rest and take pain medications if necessary.
Vorobyova Marina
Neurologist of the highest qualification category (work experience 14 years), doctor of neurofunctional diagnostics (work experience 12 years); author of scientific publications on vertebroneurology; participant of scientific conferences on neurology and functional diagnostics of all-Russian and international significance.
How to treat bullae in the lungs
The patient needs to quit smoking and quit working in harmful production activities, otherwise all therapeutic measures will be meaningless. In uncomplicated cases and in the early stages of emphysema (or bullous disease), treatment is conservative and combined. Therapy is prescribed by a pulmonologist and may include:
- Medicines (diuretics, bronchodilators, hormonal drugs);
- A special course of exercise therapy and breathing exercises;
- Regular oxygen therapy using an oxygen concentrator.
- Regular diagnostic measures (CT of the lungs, spirometry, consultation with a pulmonologist).
The positive aspect is that complete and lifelong cessation of smoking in most patients stops the development of bullous emphysema, and the use of oxygen therapy in seriously ill patients can prolong life by 5-10 years.
Surgical treatment of bullae (endoscopic “suturing”) may be indicated for recurrent pneumothorax against the background of growing cavities. The patient undergoes bullectomy and pleurodesis operations. However, the absolute success of such treatment cannot be guaranteed.