Home ▸ Articles ▸ Health ▸ Liver
The name “liver” comes from the word “oven”, because. The liver has the highest temperature of all organs of the living body. What is this connected with? Most likely due to the fact that the highest amount of energy production occurs in the liver per unit mass. Up to 20% of the mass of the entire liver cell is occupied by mitochondria, the “power stations of the cell,” which continuously produce ATP, which is distributed throughout the body. All liver tissue consists of lobules. The lobule is the structural and functional unit of the liver. The space between the liver cells is the bile ducts. There is a vein in the center of the lobule, and vessels and nerves pass through the interlobular tissue. The liver as an organ consists of two unequal large lobes: right and left. The right lobe of the liver is much larger than the left, which is why it is so easily palpable in the right hypochondrium. The right and left lobes of the liver are separated from above by the falciform ligament, on which the liver seems to be “suspended”, and below the right and left lobes are separated by a deep transverse groove. In this deep transverse groove there are the so-called gates of the liver; at this point, vessels and nerves enter the liver, and the hepatic ducts that drain bile exit. The small hepatic ducts gradually unite into one common one. The common bile duct includes the duct of the gallbladder, a special reservoir in which bile accumulates. The common bile duct flows into the duodenum, almost in the same place where the pancreatic duct flows into it. The blood circulation of the liver is not similar to the blood circulation of other internal organs. Like all organs, the liver is supplied with arterial blood saturated with oxygen from the hepatic artery. Venous blood, poor in oxygen and rich in carbon dioxide, flows through it and flows into the portal vein. However, in addition to this, which is normal for all circulatory organs, the liver receives a large amount of blood flowing from the entire gastrointestinal tract. Everything that is absorbed in the stomach, duodenum, small and large intestines is collected in the large portal vein and flows into the liver.
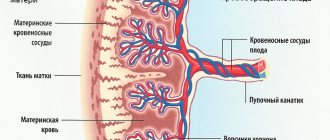
The purpose of the portal vein is not to supply the liver with oxygen and rid it of carbon dioxide, but to pass through the liver all the nutrients (and non-nutrients) that have been absorbed throughout the gastrointestinal tract. First, they pass through the portal vein through the liver, and then in the liver, having undergone certain changes, they are absorbed into the general bloodstream. The portal vein accounts for 80% of the blood received by the liver. The portal vein blood is mixed. It contains both arterial and venous blood flowing from the gastrointestinal tract. Thus, in the liver there are 2 capillary systems: the usual one, between the arteries and veins, and the capillary network of the portal vein, which is sometimes called the “miraculous network”. The normal and capillary miraculous networks are interconnected.
Sympathetic innervation
The liver is innervated by the solar plexus and branches of the vagus nerve (parasympathetic impulses). Through sympathetic fibers, the formation of urea is stimulated and impulses are transmitted through the parasympathetic nerves, increasing bile secretion and promoting the accumulation of glycogen. The liver is sometimes called the largest endocrine gland in the body, but this is not entirely true. The liver also performs endocrine excretory functions and also takes part in digestion. The breakdown products of all nutrients form, to a certain extent, a common metabolic reservoir, which all passes through the liver. From this reservoir, the body synthesizes necessary substances as needed and breaks down unnecessary ones.
Carbohydrate metabolism
Glucose and other monosaccharides entering the liver are converted into glycogen. Glycogen is stored in the liver as a “sugar reserve”. In addition to monosaccharides, lactic acid, products of the breakdown of proteins (amino acids), and fats (triglycerides and fatty acids) are also converted into glycogen. All these substances begin to turn into glycogen if there are not enough carbohydrates in food. As needed, when glucose is consumed, glycogen is converted into glucose here in the liver and enters the blood. The glycogen content in the liver, regardless of food intake, is subject to a certain rhythmic fluctuation during the day. The largest amount of glycogen is contained in the liver at night, the smallest during the day. This is due to active energy consumption during the day and the formation of glucose. Glycogen synthesis from other carbohydrates and breakdown into glucose takes place both in the liver and in the muscles. However, the formation of glycogen from protein and fat is possible only in the liver; this process does not occur in muscles. Pyruvic acid and lactic acid, fatty acids and ketone bodies - what are called fatigue toxins - are utilized mainly in the liver and converted into glucose. In the body of a highly trained athlete, more than 50% of all lactic acid is converted into glucose in the liver. Only in the liver does the “tricarboxylic acid cycle” occur, which is otherwise called the “Krebs cycle” after the English biochemist Krebs, who, by the way, is still alive. He owns classic works on biochemistry, incl. and a modern textbook. Sugar hallostasis is necessary for the normal functioning of all systems and organs. Normally, the amount of carbohydrates in the blood is 80-120 mg% (i.e. mg per 100 ml of blood), and their fluctuations should not exceed 20-30 mg%. A significant decrease in the content of carbohydrates in the blood (hypoglycemia), as well as a persistent increase in their content (hyperglycemia) can lead to serious consequences for the body. During the absorption of sugar from the intestine, the glucose content in the blood of the portal vein can reach 400 mg%. The sugar content in the blood of the hepatic vein and in the peripheral blood increases only slightly and rarely reaches 200 mg%. An increase in blood sugar immediately turns on the “regulators” built into the liver. Glucose is converted, on the one hand, into glycogen, which accelerates, on the other hand, it is used for energy, and if after that there is excess glucose, it turns into fat. Recently, data have appeared on the ability to form an amino acid substitute from glucose, but the process is organic in the body and develops only in the body of highly qualified athletes. When glucose levels decrease (prolonged fasting, large amounts of physical activity), glucogen is broken down in the liver, and if this is not enough, amino acids and fats are converted into sugar, which are then converted into glycogen. The glucose-regulatory function of the liver is supported by the mechanisms of neurohumoral regulation (regulation by the nervous and endocrine systems). Blood sugar levels are increased by adrenaline, glucose, thyroxine, glucocorticoids and diabetogenic factors of the pituitary gland. Under certain conditions, sex hormones have a stabilizing effect on sugar metabolism. Blood sugar levels are lowered by insulin, which first enters the liver through the portal vein system and only from there into the general circulation. Normally, antagonistic endocrine factors are in a state of equilibrium. With hyperglycemia, the secretion of insulin increases, with hypoglycemia - adrenaline. Glucagon, a hormone secreted by the a-cells of the pancreas, has the ability to increase blood sugar. The glucose-static function of the liver can also be subject to direct nervous effects. The central nervous system can cause hyperglycemia both humorally and reflexively. Some experiments indicate that the liver also has a system for autonomous regulation of blood sugar levels.
Anatomy of the liver
The liver consists of four main lobes: the large right lobe, the smaller left lobe, the much smaller caudate lobe, and the posterior inferior surface of the liver. The top of the liver is covered by a thin fibrous membrane - Glisson's capsule.
According to the modern segmental system, which was proposed by Claude Quinot in the 60s of the last century, the liver is divided into eight main segments. With their participation, the right and left lobes are formed. The segments themselves are presented in the form of pyramidal sections of liver tissue, which are characterized by separate blood circulation, innervation, and bile outflow.
The hepatic lobule is the main structural and functional unit of the liver
The liver has two surfaces: the diaphragmatic surface (facies diaphragmatica), adjacent to the lower surface of the diaphragm, and the visceral surface (facies visceralis), facing down and backward. The lower sharp edge of the liver and the posterior blunt edge separate the diaphragmatic and visceral parts of the organ. In some cases, the posterior edges are considered to be the posterior surface of the liver.
The diaphragmatic surface forms several main ligaments. The sagittal plane is divided by the falciform ligament to form the right and left lobes. The free edge of the falciform ligament contains the round ligament (lig. teres hepatis) - this is an overgrown umbilical vein.
The frontal plane forms the coronary ligament, at the edges of which triangular plates are located. They are designated as the left and right triangular ligaments, which provide fixation of the liver to the diaphragm2.
The visceral surface is divided into four lobes by two longitudinal and one transverse grooves. There are right, left, quadrate, and caudate furrows. The transverse groove is called the portal of the liver: the hepatic arteries, portal veins, nerves enter through it, lymphatic vessels and hepatic ducts exit.
The liver receives not only arterial but also venous blood. Between the lobules of the organ there are interlobular veins. The liver is formed by two systems of veins - portal and caval, as well as five tubular systems: bile ducts, arteries, branches of the portal vein, hepatic veins, lymphatic vessels.
Protein metabolism
The role of the liver in protein metabolism is the breakdown and “rearrangement” of amino acids, the formation of chemically neutral urea from ammonia, which is toxic to the body, as well as the synthesis of protein molecules. Amino acids, which are absorbed in the intestine and formed during the breakdown of tissue protein, constitute the body’s “reservoir of amino acids,” which can serve as both a source of energy and a building material for protein synthesis. Isotopic methods have established that in the human body, 80-100 g of protein are broken down and synthesized again. Approximately half of this protein is transformed in the liver. The intensity of protein transformations in the liver can be judged by the fact that liver proteins are renewed in about 7 (!) days. In other organs, this process occurs in at least 17 days. The liver contains the so-called “reserve protein”, which is used for the body’s needs if there is not enough protein in food. During a two-day fast, the liver loses approximately 20% of its protein, while the total protein loss of all other organs is only about 4%. Transformation and synthesis of missing amino acids can only occur in the liver; even if 80% of the liver is removed, a process such as deamination remains. The formation of non-essential amino acids in the liver occurs through the formation of glutamic and aspartic acid, which serve as an intermediate link. An excess amount of a particular amino acid is reduced first to pyruvic acid, and then in the Krebs cycle to water and carbon dioxide with the formation of energy stored in the form of ATP. In the process of desemination of amino acids - the removal of amino groups from them - a large amount of toxic ammonia is formed. The liver converts ammonia into non-toxic urea (urea), which is then excreted from the body by the kidneys. Urea synthesis occurs only in the liver and nowhere else. The synthesis of blood plasma proteins—albumin and globulins—occurs in the liver. If blood loss occurs, then with a healthy liver the content of blood plasma proteins is very quickly restored; while with a diseased liver, such recovery slows down significantly.
Primary liver cancer: diagnosis
All people who are at high risk for developing liver cancer are regularly screened. First of all, doctors look for ultrasound signs
Liver cancer in people suffering from chronic inflammatory processes of the organ have different degrees of cirrhosis. They are advised to perform an ultrasound examination every six months, even in the absence of complaints.
In addition, they are advised to perform laboratory blood tests to determine the tumor marker of primary liver cancer - AFP
(stands for alpha-fetoprotein). With this type of observation, it is possible to identify tumor lesions at an early stage (there are no symptoms or complaints yet), when the cancer can be radically cured. Changes in tests for liver cancer with an increase in AFP typically occur in up to 50-90% of patients. Levels greater than 400 ng/mL may occur in individuals with large tumors or rapidly growing tumors. But a temporary increase in the indicator is possible against the background of cirrhosis or inflammation of hepatocytes. However, high AFP in combination with ultrasound data and MRI of the liver confirms the diagnosis in almost 100% of patients.
Performing a CT
or
MRI with contrast
helps to identify a tumor and clarify its size and location, which is important for drawing up a treatment plan for liver oncology.
If all this data is not enough to make a diagnosis, a percutaneous biopsy
(puncture or aspiration) under ultrasound control. The risk of complications with such diagnostic methods is minimal.
Fat metabolism
The liver can store much more fat than glycogen. The so-called “structural lipid” - structural lipids of the liver - phospholipids and cholesterol make up 10-16% of the dry matter of the liver. This number is fairly constant. In addition to structural lipids, the liver contains inclusions of neutral fat, similar in composition to subcutaneous fat. The content of neutral fat in the liver is subject to significant fluctuations. In general, we can say that the liver has a certain fat reserve, which, if there is a deficiency of neutral fat in the body, can be spent on energy needs. In case of energy deficiency, fatty acids can be well oxidized in the liver with the formation of energy stored in the form of ATP. In principle, fatty acids can be oxidized in any other internal organs, but the percentage will be as follows: 60% liver and 40% all other organs. Bile secreted by the liver into the intestines emulsifies fats, and only as part of such an emulsion can fats be subsequently absorbed in the intestines. Half of the cholesterol in the body is synthesized in the liver and only the other half is of dietary origin. The mechanism of liver oxidation of fatty acids was elucidated at the beginning of this century. It comes down to so-called b-oxidation. Oxidation of fatty acids occurs up to the 2nd carbon atom (b-atom). The result is a shorter fatty acid and acetic acid, which is then converted to acetoacetic acid. Acetoacetic acid is converted to acetone, and the new b-oxidized acid undergoes oxidation with great difficulty. Both acetone and b-oxidized acid are collectively referred to as “ketone bodies.” To break down ketone bodies, you need a fairly large amount of energy, and if there is a deficiency of glucose in the body (fasting, diabetes, prolonged aerobic exercise), a person’s breath may smell like acetone. Biochemists even have this expression: “fats burn in the fire of carbohydrates.” For complete combustion, complete utilization of fats into water and carbon dioxide with the formation of a large amount of ATP, at least a small amount of glucose is required. Otherwise, the process will stall at the stage of formation of ketone bodies, which shift the blood pH to the acidic side, along with lactic acid, taking part in the formation of fatigue. It’s not for nothing that they are called “fatigue toxins.” Fat metabolism in the liver is influenced by hormones such as insulin, ACTH, diabetogenic factor of the pituitary gland, and glucocorticoids. The action of insulin promotes the accumulation of fat in the liver. The action of ACTH, diabetogenic factor, and glucocorticoids is exactly the opposite. One of the most important functions of the liver in fat metabolism is the formation of fat and sugar. Carbohydrates are a direct source of energy, and fats are the most important energy reserves in the body. Therefore, with an excess of carbohydrates and, to a lesser extent, proteins, fat synthesis predominates, and with a lack of carbohydrates, gluconeogenesis (glucose formation) from protein and fat dominates.
Cholesterol metabolism
Cholesterol molecules form the structural framework of all cell membranes without exception. Cell division is simply impossible without sufficient cholesterol. Bile acids are formed from cholesterol, i.e. essentially bile itself. All steroid hormones are formed from cholesterol: glucocorticoids, mineralocorticoids, and all sex hormones. Cholesterol synthesis is therefore genetically determined. Cholesterol can be synthesized in many organs, but it is most intensively synthesized in the liver. By the way, the breakdown of cholesterol also occurs in the liver. Some of the cholesterol is excreted unchanged into the intestinal lumen with bile, but most of the cholesterol - 75% is converted into bile acids. The formation of bile acids is the main pathway of cholesterol catabolism in the liver. For comparison, let's say that only 3% of cholesterol is consumed for all steroid hormones taken together. A person excretes 1-1.5 g of cholesterol per day with bile acids. 1/5 of this amount is excreted from the intestines, and the rest is reabsorbed into the intestines and ends up in the liver.
Liver topography
The liver is attached to the diaphragm, abdominal wall, stomach, and intestines with the help of ligaments. Fills the area of the right hypochondrium, located under the diaphragmatic dome. Rising up to the chest, to a small extent it occupies the left hypochondrium. The two main ligaments that attach the liver to the diaphragm are the falciform and the coronoid. The organ is also supported by the lesser omentum and the inferior vena cava.
Thanks to such topographic characteristics, the liver is subordinate to the movements of the diaphragm; it is easy to feel when inhaling against the background of abdominal breathing. That is why the pathological process from the liver easily passes to the area of the diaphragm: the right pleura and the right lung. Liver prolapse is observed with a significant decrease in body weight, a decrease in intra-abdominal pressure, and with the accumulation of fluid in the pleural cavity.
Vitamins
All fat-soluble vitamins (A, D, E, K, etc.) are absorbed into the intestinal walls only in the presence of bile acids secreted by the liver. Some vitamins (A, B1, P, E, K, PP, etc.) are deposited by the liver. Many of them are involved in chemical reactions occurring in the liver (B1, B2, B5, B12, C, K, etc.). Some vitamins are activated in the liver, undergoing phosphorication there (B1, B2, B6, choline, etc.). Without phosphorus residues, these vitamins are completely inactive and often the normal vitamin balance in the body depends more on the normal state of the liver than on the sufficient intake of one or another vitamin in the body. As we can see, both fat-soluble and water-soluble vitamins can be deposited in the liver; only the time of deposition of fat-soluble vitamins, of course, is disproportionately longer than that of water-soluble vitamins.
Causes and risk factors
The exact causes of liver cancer have not yet been established. Most often, a malignant lesion occurs against the background of a long-term inflammatory process in the liver tissue. Most often, the first signs of liver cancer are detected against the background of cirrhosis. In regions where viral hepatitis is widespread, cases of liver cancer are detected much more often. Thus, approximately 25% of all patients with signs of liver cancer are diagnosed with viral hepatitis C, and approximately 40% are chronic carriers of the hepatitis B virus.
Other risk factors that increase the risk of developing liver cancer include:
- poor nutrition leading to obesity;
- drinking large amounts of alcohol;
- long-term use of drugs that have hepatotoxicity (including steroids, oral contraceptives);
- the influence of external factors - toxins that damage liver cells (vinyl chloride, aflatoxins);
- long history of diabetes mellitus;
- Budd-Chiari syndrome (these are episodes of thrombosis in the hepatic veins);
- hereditary pathologies - Wilson's disease, hemochromatosis, tyrosinemia, glycogenosis, alpha-trypsin deficiency, intestinal polyposis.
In some cases, the causes of liver cancer cannot be determined, and the cases are considered idiopathic.
Hormone exchange
The role of the liver in the metabolism of steroid hormones is not limited to the fact that it synthesizes cholesterol - the basis from which all steroid hormones are then formed. In the liver, all steroid hormones are inactivated, although they are not formed in the liver. The breakdown of steroid hormones in the liver is an enzymatic process. Most steroid hormones are inactivated by combining with glucuronic fatty acid in the liver. When liver function is impaired, the body first of all increases the content of hormones of the adrenal cortex, which are not completely broken down. This is where many different diseases arise. Aldosterone, a mineralocorticoid hormone, accumulates most in the body, the excess of which leads to sodium and water retention in the body. As a result, edema occurs, a rise in blood pressure, etc. In the liver, thyroid hormones, antidiuretic hormone, insulin, and sex hormones are largely inactivated. In some liver diseases, male sex hormones are not destroyed, but turn into female ones. This disorder occurs especially often after methyl alcohol poisoning. The excess of androgens itself, caused by the introduction of a large amount of them from the outside, can lead to increased synthesis of female sex hormones. There is, obviously, a certain threshold for the content of androgens in the body, exceeding which leads to the conversion of androgens into female sex hormones. Although, recently there have been publications that some medications can prevent the conversion of androgens into estrogens in the liver. Such drugs are called blockers. In addition to the above hormones, the liver inactivates neurotransmitters (catecholamines, serotonin, histamine and many other substances). In some cases, even the development of mental illness is caused by the inability of the liver to inactivate certain neurotransmitters.
Clinical manifestations of pathologies
Everyone needs to know what the liver is for, how important it is, and how long it takes to suspect liver dysfunction. During the diagnosis, the patient is interviewed, the size, density, surface of the organ is analyzed, and liver function is assessed.
The gland can be affected by:
- Cirrhosis. The structure of the liver is represented by a pathological proliferation of fibrous (connective) tissue, which replaces functional hepatocytes. Liver dysfunction may be caused by:
- chronic alcoholism;
- hepatitis of viral etiology;
- infection of the gland by helminths, Trichomonas.
- Oncological process – cancer. The reasons for its occurrence are not fully known, however, among the predisposing factors it is worth highlighting:
- cirrhosis;
- viral hepatitis;
- alcoholism;
- contact with carcinogenic substances;
- hereditary predisposition.
- Hemangiomas, or abnormalities of vascular development.
- Cysts (parasitic - echinococcosis, as well as non-parasitic).
As soon as it is noticed that the liver hurts, you should consult a doctor. The specialist will examine the body, especially carefully palpate the area of the right hypochondrium, and prescribe the necessary examinations. Palpation can be carried out on the back or side. In addition, you should pay attention to the main symptoms indicating possible organ dysfunction:
- weakness, feeling of constant fatigue;
- weight loss;
- vomiting, nausea, bloating, indigestion;
- yellowing of mucous membranes and skin;
- causeless increase in temperature;
- itchy skin;
- spider veins;
- a feeling of bitterness in the mouth;
- excessive sweating;
- hypersensitivity to odors;
- change in color of stool and urine.
The listed symptoms are the basis for contacting a gastroenterologist, who, through a full examination, will identify abnormalities in the functioning of the gland and prescribe effective therapy. Only a specialist will be able to figure out what is the cause of liver dysfunction, so you should not self-medicate.
Bile formation
Bile, produced by the liver, as we have already said, takes an active part in the digestion of fats. However, the matter is not limited to just their emulsification. Bile activates the fat-splitting enzyme liposis of pancreatic and intestinal juice. Bile also accelerates the absorption in the intestines of fatty acids, carotene, vitamins P, E, K, cholesterol, amino acids, and calcium salts. Bile stimulates intestinal motility. The liver produces at least 1 liter of bile per day. Bile is a greenish-yellow, slightly alkaline liquid. The main components of bile: bile salts, bile pigments, cholesterol, lecithin, fats, inorganic salts. Hepatic bile contains up to 98% water. In terms of its osmotic pressure, bile is equal to blood plasma. From the liver, bile enters the hepatic duct through the intrahepatic bile ducts, from where it is directly secreted through the cystic duct and enters the gallbladder. Here the concentration of bile occurs due to the absorption of water. The density of gallbladder bile is 1.026-1.095. Some of the substances that make up bile are synthesized directly in the liver. The other part is formed outside the liver and, after a series of metabolic changes, is excreted with bile into the intestine. Thus, bile is formed in two ways. Some of its components are filtered from the blood plasma (water, glucose, creatinine, potassium, sodium, chlorine), others are formed in the liver: bile acids, glucuronides, paired acids, etc. The most important bile acids are cholic and deoxycholic in combination with the amino acids glycine and taurine forms paired bile acids - glycocholic and taurocholic. The human liver produces 10-20 g of bile acids per day. Entering the intestines with bile, bile acids are broken down with the help of enzymes from intestinal bacteria, although most of them are reabsorbed by the intestinal walls and end up back in the liver. Only 2-3 g of bile acids are released with feces, which, as a result of the decomposing action of intestinal bacteria, change their color from green to brown and change their smell. Thus, there is a sort of hepatic-intestinal circulation of bile acids. If it is necessary to increase the excretion of bile acids from the body (for example, in order to remove large amounts of cholesterol from the body), then substances are taken that irreversibly bind bile acids, which do not allow bile acids to be absorbed in the intestines and remove them from the body along with feces. The most effective in this regard are special ion exchange resins (for example, cholestyramine), which, when taken orally, are capable of binding a very large amount of bile and, accordingly, bile acids in the intestine. Previously, activated carbon was used for this purpose.
They still use it now. Fiber in vegetables and fruits, but even more so, pectin substances, have the ability to absorb bile acids and remove them from the body. The largest amount of pectin substances is found in berries and fruits, from which jelly can be made without the use of gelatin. First of all, these are red currants, then, according to their gelling ability, they are followed by black currants, gooseberries, and apples. It is noteworthy that baked apples contain several times more pectin than fresh ones. Fresh apples contain protopectins, which turn into pectins when apples are baked. Baked apples are an indispensable attribute of all diets when you need to remove a large amount of bile from the body (atherosclerosis, liver disease, some poisoning, etc.). Bile acids, among other things, can be formed from cholesterol. When eating meat food, the amount of bile acids increases, and when fasting, it decreases. Thanks to bile acids and their salts, bile performs its functions in the process of digestion and absorption. Bile pigments (the main one is bilirubin) do not take part in digestion. Their secretion by the liver is a purely excretory process. Bilirubin is formed from hemoglobin of destroyed red blood cells in the spleen and special liver cells (Kupffer cells). It’s not for nothing that the spleen is called the graveyard of red blood cells. With regard to bilirubin, the main task of the liver is its excretion, not its formation, although a considerable part of it is formed in the liver. It is interesting that the breakdown of hemoglobin to bilirubin is carried out with the participation of vitamin C. Between hemoglobin and bilirubin there are many intermediate products that can be mutually converted into each other. Some of them are excreted in urine, and some in feces. The formation of bile is regulated by the central nervous system through various reflex influences. Bile secretion occurs continuously, increasing during meals. Irritation of the splanchnic nerve leads to a decrease in bile production, and irritation of the vagus nerve and histamines increase bile production. Biliary excretion, i.e. The entry of bile into the intestines occurs periodically as a result of contraction of the gallbladder, depending on food intake and its composition.
Preparation
Ultrasound of the liver and abdominal organs requires preparation from both adults and children.
This scan should be performed on an empty stomach with a 6-hour fast. It is better to stop drinking 2 hours before the examination. If your body is prone to excessive gas formation and flatulence, you need to adhere to a special diet 2-3 days before the procedure, excluding flour and legume products, carbonated and alcoholic drinks. In the case where an ultrasound of the liver is planned to be performed on a child, the small patient should also be prepared. The first and rather difficult stage will be to limit food intake before the study. The minimum abstinence time for children is 3 hours (drinking is also excluded). Such preparation for a child can be difficult and is carried out only if the children tolerate restrictions on food and drinks relatively calmly. If such abstinence is difficult to achieve, you should stick to your regular eating schedule. Author: Telegina Natalya Dmitrievna
Therapist with 25 years of experience
Excretory (excretory) function
The excretory function of the liver is very closely related to bile formation, since substances excreted by the liver are excreted through bile and, if only for this reason, they automatically become an integral part of bile. Such substances include the thyroid hormones already described above, steroid compounds, cholesterol, copper and other trace elements, vitamins, porphyrin compounds (pigments), etc.
Substances excreted almost exclusively with bile are divided into two groups:
- Substances bound to proteins in the blood plasma (for example, hormones).
- Substances insoluble in water (cholesterol, steroid compounds).
One of the features of the excretory function of bile is that it is capable of introducing substances from the body that cannot be removed from the body in any other way. There are few free compounds in the blood. Most of the same hormones are tightly bound to transport proteins in the blood and, being firmly bound to the proteins, cannot overcome the kidney filter. Such substances are excreted from the body along with bile. Another large group of substances that cannot be excreted in urine are substances that are insoluble in water. The role of the liver in this case is that it combines these substances with glucuronic acid and thus converts them into a water-soluble state, after which they are freely excreted through the kidneys. There are other mechanisms that allow the liver to remove water-insoluble compounds from the body.
Neutralizing function
The liver plays a protective role not only by neutralizing and removing toxic compounds, but even by microbes that get into it, which it destroys. Special liver cells (Kupffer cells), like amoebas, capture foreign bacteria and digest them. In the process of evolution, the liver has become an ideal organ for neutralizing toxic substances. If it cannot turn a toxic substance completely non-toxic, it makes it less toxic. We already know that toxic ammonia is converted into non-toxic urea (urea) in the liver. Most often, the liver neutralizes toxic compounds by forming paired compounds with them with glucuranic and sulfuric acid, glycine, taurine, cysteine, etc. This is how highly toxic phenols are neutralized, steroids and other substances are neutralized. A major role in neutralization is played by oxidative and reduction processes, acetylation, methylation (which is why vitamins containing free methyl radicals-CH3 are so useful for the liver), hydrolysis, etc. For the liver to perform its detoxification function, sufficient energy supply is necessary, and for this, in in turn, it requires a sufficient glycogen content and the presence of a sufficient amount of ATP.
Blood clotting
The liver synthesizes substances necessary for blood clotting, components of the prothrombin complex (factors II, VII, IX, X), the synthesis of which requires vitamin K. The liver also produces fibranogen (a protein necessary for blood clotting), factors V, XI, XII , XIII. Strange as it may seem at first glance, the liver synthesizes elements of the anticoagulant system - heparin (a substance that prevents blood clotting), antithrombin (a substance that prevents the formation of blood clots), and antiplasmin. In embryos (fetuses), the liver also serves as a hematopoietic organ where red blood cells are formed. With the birth of a person, these functions are taken over by the bone marrow.
Types of primary liver cancer
There are several classification options for primary liver cancer. There are various types of tumors, which differ in course and prognosis. Experts identify several of the most typical types of primary liver cancer (the tumor is formed from the cells of the organ).
Hepatocellular cancer
is the most common tumor (carcinoma) that occurs in the liver area.
As the name suggests, these tumors form in hepatocytes, which form the basis of liver tissue. The course of hepatocellular cancer is possible in two clinical forms - diffuse
(when a large part of the liver is affected) or
nodular
(one focus is formed - a node or several areas).
A more favorable variant of this cancer is possible - fibrolamellar carcinoma
, with it there are possibilities for more active treatment.
Cholangiocarcinoma
is a malignant tumor that originates in the area of the bile ducts.
Cholangiohepatoma
is a mixed type of tumor in which cancer cells originate both in the area of hepatocytes and in the area of epithelial cells in the bile ducts.
Variants of tumors such as angiosarcomas, mesodermal formations
are lesions that grow from lymphatic capillaries, blood vessels or connective tissue cells.
Possible hepatoblastoma
cystadenocarcinoma
is also identified . It occurs as a result of the degeneration of a benign tumor.
Redistribution of blood in the body
The liver, in addition to all its other functions, performs quite well as a blood depot in the body. In this regard, it can affect the blood circulation of the entire body. All intrahepatic arteries and veins have sphincters, which can change blood flow in the liver over a very wide range. On average, blood flow in the liver is 23 ml/kx/min. Normally, almost 75 small vessels of the liver are excluded from the general circulation by sphincters. With an increase in total blood pressure, liver vessels dilate and hepatic blood flow increases several times. On the contrary, a drop in blood pressure leads to vasoconstriction in the liver and hepatic blood flow is reduced. Changes in body position are also accompanied by changes in hepatic blood flow. For example, in a standing position, liver blood flow is 40% lower than in a lying position. Norepinephrine and sympathetic increase vascular resistance in the liver, which reduces the amount of blood flowing through the liver. The vagus nerve, on the other hand, reduces vascular resistance in the liver, which increases the amount of blood flowing through the liver. The liver is very sensitive to lack of oxygen. Under conditions of hypoxia (lack of oxygen in tissues), vasodilator substances are formed in the liver, reducing the sensitivity of capillaries to adrenaline and increasing hepatic blood flow. With prolonged aerobic work (running, swimming, rowing, etc.), the increase in hepatic blood flow can reach such an extent that the liver greatly increases in volume and begins to put pressure on its outer capsule, richly supplied with nerve endings. The result is pain in the liver, familiar to every runner, and indeed to all those who engage in aerobic sports.
How is liver ultrasound performed?
The ultrasound procedure in medical institutions is carried out in a separate, specially equipped room, where the ultrasound machine itself is located with a monitor, keyboard and sensors and a couch for the patient. The patient will not have to undress completely during an ultrasound of the liver and abdominal organs. It will be enough to expose the abdominal area and lie down on a couch covered with a disposable sheet. The doctor will then indicate the position in which the examination will be performed. He will ask you to lie down either on your back or on your left side. After the patient has taken the desired position, the diagnostician applies a special gel to the sensor and the area of study for tighter contact and smooth sliding and begins to move it sequentially in different directions. During the ultrasound procedure, the diagnostician will give instructions to the patient for clearer visualization. He may ask the subject to inhale as hard as possible and hold his breath, exhale forcefully, or breathe normally. Different breathing intensities will help the doctor collect more information about the abdominal organs and the features of their anatomical structure. After the diagnostician has made all the necessary measurements, the liver examination is considered complete. The subject can slowly get up, remove the gel from the abdominal area with a disposable towel and get dressed.
Age-related changes
The functional capabilities of the human liver are highest in early childhood and decrease very slowly with age. The liver weight of a newborn child averages 130-135 g. The liver weight reaches its maximum between the ages of 30-40 years, and then gradually decreases, especially between 70-80 years, and in men the liver weight drops more than in women. The regenerative abilities of the liver decrease somewhat in old age. At a young age, after removal of the liver by 70% (wounds, injuries, etc.), the liver restores the lost tissue by 113% (in excess) after a few weeks. Such a high ability to regenerate is not inherent in any other organ and is even used to treat severe chronic liver diseases. So, for example, in some patients with liver cirrhosis, it is partially removed and it grows back, but new, healthy tissue grows. With age, the liver no longer recovers completely. In old people, it grows only 91% (which, in principle, is also a lot). The synthesis of albumins and globulins decreases in old age. Albumin synthesis mainly decreases. However, this does not lead to any disturbances in tissue nutrition or a drop in oncotic blood pressure, because With old age, the intensity of breakdown and consumption of proteins in plasma by other tissues decreases. Thus, even in old age, the liver meets the body’s needs for the synthesis of plasma proteins. The ability of the liver to store glycogen also varies at different age periods. Glycogen capacity reaches its maximum by three months of age, remains for life and only slightly decreases in old age. Fat metabolism in the liver reaches its normal level also at a very early age and decreases only slightly in old age. At different stages of the body’s development, the liver produces different amounts of bile, but always covers the body’s needs. The composition of bile changes somewhat throughout life. So, if a newborn child’s liver bile contains bile acids of about 11 mEq/L, then by the age of four this amount decreases almost 3 times, and by the age of 12 it increases again and reaches approximately 8 mEq/L. The rate of emptying of the gallbladder, according to some data, is the lowest in young people, and in children and the elderly it is much higher. In general, according to all its indicators, the liver is a low-aging organ. It serves a person well throughout his life.
Author: Bulanov Yu.B.
General information
The liver is one of the most important organs of the human body, which is a glandular formation. How much does a human liver weigh? Its mass reaches one and a half kilograms, thanks to which it performs many vital functions, which we will talk about a little later.
The gland is located in the right hypochondrium, so it is here that the organ is palpated to assess its size, density and outline.
Now we will more accurately describe where the liver is located. The location of the liver in a person depends to some extent on his age. So, in an adult it is located in the right hypochondrium, and slightly extends beyond the border of the midline of the abdomen. In children, the gland occupies most of the abdominal cavity.
The upper border of the liver is at the level of the cartilage of the 5th rib, when assessed along the midclavicular line. Moving along the liver to the left side, we reach the xiphoid process of the sternum, then we head to the cartilage of the 6th rib. The lower border runs along the edge of the costal arch. The gland touches the diaphragm from above, the abdominal wall from the front, and the spinal column, aorta and esophagus from the back. To the left of the gland are organs such as the stomach and duodenum.
The location of the human liver is mesoperitoneal. It is customary to speak of such an arrangement when the organ is not surrounded on all sides by the peritoneum. The physiological structure of the liver does not have compactions, deformations, or additional neoplasms. It is represented by a homogeneous fabric with a small grain size. The edges of the organ are even and the surface is smooth.
The gland has bile ducts and blood vessels. The liver contains hepatocytes (liver cells), which ensure the functioning of the organ and the body as a whole.