Anatomy
Short review
The vagina is an elastic but muscular canal that is approximately 9-10 centimeters in length. The upper part of it connects to the cervix, which opens into the uterus, and the lower part opens to the outside of the body (in virgins, the entrance to the vagina is normally covered by the hymen). It lies between the urethra (which connects to the bladder) and the rectum. During sexual intercourse, the vagina lengthens, dilates, and fills with blood, preparing itself to better accommodate the penis. In addition, the vagina serves as an outlet for cervical mucus, menstrual blood and other secretions. During childbirth, the baby is pushed out of the uterus and out of the body through the vaginal canal by contraction of the muscles of the perineum and pelvis.
Vaginal walls
The thickness of the vaginal walls is 3-4 mm. They consist of several layers:
- External (adventitial membrane), represented by connective tissue with elastic and muscle fibers.
- Middle layer (smooth muscles, together with the muscles of the perineum, creates and maintains the so-called “vaginal tone”). The muscle fiber bundles are located predominantly in the longitudinal direction. In the upper part they connect to form the muscles of the uterus, and from the bottom they are directly woven into the muscle fibers located in the perineum.
- The inner layer (mucosa), consisting of stratified squamous epithelium, forms transverse folds, which, if necessary, allow this organ to stretch to the desired volume.
The walls of the vagina, together with the cervix, are constantly wet. The fact is that they are lined with secreting glands that produce the so-called cervical mucus. It prevents the proliferation of pathogenic bacteria and their penetration deep into the organs of the reproductive system. The volume of this secretion is small and practically imperceptible. When a woman begins to notice the appearance of uncharacteristic vaginal discharge (with an unpleasant odor, itching, discomfort), this is a good reason to go to the gynecologist and get tested!
What functions does the vagina have?
- Sexual - participation in the process of fertilization. The main function of the vagina is to participate in the process of conceiving children: seminal fluid flowing from the man’s penis during intimacy enters the vagina, from where sperm penetrate the uterus through the tubes. First, sperm accumulates in the posterior, deepest, vaginal vault, which borders the cervix.
- Barrier - protects the internal genital organs from germs. The vagina has an important ability, in particular, to cleanse itself or regulate the stability of its flora. This process is regulated by female hormones - estrogen and progesterone, secreted by the ovaries. Under the influence of estrogen, cells in the vaginal mucosa synthesize glycogen, a substance that is then converted into lactic acid. The process of producing lactic acid from glycogen occurs with the participation of lactic acid bacteria (Doderlein bacillus), while the normal vaginal environment maintains an acidic environment (pH in the range of 3.8 to 4.5).
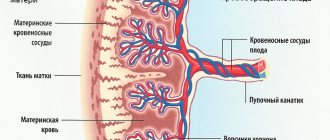
- Participation in childbirth is part of the birth canal during natural childbirth. The vagina, together with the cervix, forms the birth canal through which the baby leaves the uterus. During pregnancy, vaginal tissue changes under the influence of hormones, its walls become more elastic and can stretch enough to smoothly bring the fetus into the world.
- Excretory - releases vaginal and menstrual secretions into the environment. A healthy woman's vagina produces up to 2 ml of excretion per day, but the amount of fluid can vary depending on the phase of the menstrual cycle.
Structural features
Throughout your life, your vagina may look and feel different. To keep your vagina healthy, it is important to understand its anatomy and functioning, as well as what happens there at different times in a girl's life.
- The size of a woman's vagina in an aroused state changes, as does the size of a man's penis before and during an erection. During sexual arousal, the cervix moves deeper, making the vagina longer and more spacious in structure;
- The walls of the vagina are very elastic formations, which in a sexually mature female are quite stretchable; in an unexcited state, friction causes discomfort in a woman;
- In a non-excited state, the depth of the vagina in most women is 8-11 cm, the diameter is no more than 3.0 cm. In the excited state, the depth reaches 15-18 cm, the diameter of the vagina is up to 6-7 cm. In some women, after appropriate preparation, the structure of the vagina changes - its depth can reach 23 - 25 cm, diameter - 10 cm or more.;
- In medicine there is a term “vaginal accommodation”. It means that with constant sexual contact with the same man, the woman’s vaginal dimensions adjust to the parameters of his penis;
- In 85-90% of cases, the size of a woman's vagina is directly proportional to its height. In short patients, the vaginal size is smaller than in tall representatives of the fair sex. However, there are frequent exceptions to this rule;
- Throughout life, the length and volume of the vagina can change. This usually occurs due to events such as childbirth and abortion, as well as hormonal imbalances, significant physical activity and age;
- The inner walls of the vagina, contrary to popular belief, have very low sensitivity. Less than 15% of women are able to feel a touch to its walls. Therefore, many therapeutic and diagnostic procedures in a gynecologist’s office do not cause significant discomfort. But it can hurt for completely different reasons (see here).
Vagina from 0 to 18+
In newborn girls, the length of this body is only 3 cm. Its walls fit tightly to each other. All this is due to the fact that the pelvic muscles of little girls are still very weak. Over about 1 year of life, the length of the vagina increases by about 1 cm. Only by 8-10 years can the so-called folding, which is characteristic of any female vagina, be detected in this organ. It is thanks to it that the size of the organ changes during childbirth, as well as during sexual intercourse. The greatest increase in the size of the vagina in a virgin begins at about 10 years old, and by 12-13 years it reaches an average of 7-8 cm.
Microflora of the vagina of girls
Immediately after a girl is born, her vagina is sterile. Only 3-4 hours after birth are lactobacilli, bifidobacteria and other microorganisms found there. At about 9-10 years of age, the puberty phase begins in girls. Starting from this period, girls begin to experience mucous discharge. They are usually clear, odorless and non-disturbing. The composition of the microflora also changes: in 60% of cases, lactobacilli are detected, the vaginal environment becomes acidic, the pH is 4 - 4.5. From adolescence (16 years +), the vaginal microflora in teenage girls becomes the same as in adult women.
How does the vagina change with the onset of puberty?
With the onset of puberty (18+), this organ becomes longer and wider. Thus, the body prepares to perform the main function of the reproductive system - reproduction. If we talk about what features a virgin’s vagina has, then its structure has, perhaps, the only feature - the hymen. It is this mucous septum that protects the internal genital organs from the external ones and prevents the penetration of pathogenic microorganisms into them. During the first sexual intercourse, this formation ruptures, which is often accompanied by a small amount of blood. If we talk about what the entrance to a virgin’s vagina looks like, then, as a rule, it is smaller than that of women who regularly have sex.
Vagina at 20 - 30 years old
Your years from approximately 18 to 30 are some of the best years of your vagina's life, mainly due to the peak of the sex hormones estrogen, progesterone and testosterone. Estrogen is responsible for keeping your vagina well moisturized and lubricated, the walls elastic, and the internal environment optimal in terms of acid-base balance.
During this age period, a woman’s vagina cleanses itself. Hormonal changes during the menstrual cycle affect the amount and composition of discharge that is constantly produced by this intimate area. Unless you have symptoms such as pain during sex, private itching, foul-smelling discharge or burning, your vagina does not require any maintenance other than daily external washing with mild soap and water.
Vagina from 30 to 40 years
One of the most noticeable vaginal changes in women after age 30 is a decrease in pelvic floor strength. Because the pelvic muscles support the bladder, uterus, and bowels, a variety of problems like urinary incontinence (especially when you sneeze, cough, or laugh), and even prolapse (when the uterus, bladder, or bowel slips out of place) can occur when the muscles The pelvic floor loses its strength with age. Vaginal birth may worsen these symptoms.
After previous childbirth, your vagina may lose some of its elasticity and stretch more than usual. Over time, most vaginas usually return to almost their prenatal size. Kegel exercises and special exercise machines can help strengthen the pelvic floor muscles and restore vaginal tone. To maintain health, regular medical examinations with a gynecologist are recommended.
Vagina from 40 to 50
Thanks to perimenopause (that period of time between about 43 and 47 years of age, just before your menstrual bleeding stops), your vagina goes through significant changes.
Levels of the hormone estrogen decrease, the vaginal walls become thinner and drier, the labia minora may become stretched, and the labia majora may become flabby and wrinkled. Irregular menstrual cycles, vaginal dryness, and hot flashes may occur. And although menopause may be looming ahead, some women give birth during this decade. Essentially, your 40s may mark the end of both your fertility and the end of your ability to conceive. This is known as vaginal atrophy and is accompanied by the following symptoms:
• vaginal burning • vaginal redness • painful sex • vaginal discharge • vaginal itching • burning during urination • shortening of the vaginal canal • increased risk of STDs
Regular intimate life, mostly with orgasms, helps slow the progression of vaginal atrophy by increasing blood flow to the vagina and keeping it elastic. In the absence of more or less regular sex, a good option for preventing blood stagnation in the internal genital organs would be a special therapeutic and preventive massage of the pelvic organs. Vaginal moisturizers or the use of estrogen cream may also help combat vaginal dryness. If you prefer the natural route, olive oil and coconut oil can help keep your vagina hydrated.
Pubic hair may thin or turn gray by the end of your fourth decade.
Questions and answers about the vagina
1. Does the vagina inherently smell bad? Odors may change depending on the day of the menstrual cycle, under the influence of medications or eating habits. Eating garlic, onions, broccoli, asparagus, white cabbage, spices, red meat, and blue cheese adds unique nuances to the vaginal aroma. But in any case, a healthy vagina does not smell like rotten fish or milk that went sour a few days ago.
2. Is discharge normal? They are a natural phenomenon for the female body. Consist of cervical mucus and vaginal secretions. Their intensity, character and consistency depend on the phase of the cycle. Normally, they can be transparent, whitish, watery, viscous... If vaginal discharge acquires a cheesy consistency, smells unpleasant, turns yellowish, grayish or greenish, or has blood in it, this is a good reason to immediately go for a consultation with a gynecologist and get tested.
3. Are expensive lingerie the key to vaginal health? The best choice for maintaining vaginal health is underwear that contains cotton. It allows air to pass through well and absorbs moisture, which reduces the risk of dysbacteriosis and fungal infections.
4. Does the vagina need “scented soap” and periodic “cleaning”? The female vagina is a self-cleaning system that does not require additional hygiene procedures such as douching, lathering with intimate gels or wiping with antibacterial wipes. Such activities disrupt the unique balance of beneficial microflora and create the preconditions for the proliferation of pathogenic microbes.
5. The more sex, the wider the vagina and vice versa? The size of your vagina does not depend on the number of sexual acts in your life. After a long break, a feeling of “tightness” in the vagina may arise from loss of the habit of intercourse or inability to relax.
6. Will the vagina necessarily tear during childbirth? Up to 80 percent of vaginal births involve tearing or require an incision. If there is a risk of rupture of the vaginal opening and to facilitate passage of the fetal head, obstetricians prefer to make an incision (called an episiotomy). It is indicated when, for example, the baby is positioned feet first or labor should go faster. But don't be scared! Your vagina is elastic and, thanks to its abundant blood supply, actually heals faster than other parts of the body.
7. What is point “A” in “that” place? The anterior vestibule, or “A spot,” is a small area of the vagina that is located deeper along the front wall of the vagina than the G spot. According to some overseas research, stimulating your A spot is an easy way to create more lubrication in the vagina. Moreover, 15 percent of study participants achieved orgasm within 10 to 15 minutes of A-spot stimulation.
Vaginal sizes: truth and myths
(excerpt from the “Intimate Book”) Questions about the vagina are of interest to many people, primarily regarding the correspondence of the penis to the size of the vagina. I have repeatedly heard complaints from women who experience discomfort and pain during sexual intercourse that their vagina is obviously too small and not adapted to accept the male sexual organ. This complaint simultaneously became a justification for refusing sexual relations to one’s partners.
Often, having fallen into the hands of a female doctor, such women become hostages of endless diagnostic studies and treatments, which not only harm the female body, but ultimately kill her sexual attraction to men, and also in many cases leads to the collapse of a marriage, official or civil.
What is the mystery of the vagina if it can attract a man no less than cars, cigarettes and other male hobbies?
For information, the vagina (vagina) is a kind of muscular canal, stretchable and elastic, connecting the external genitalia and the uterus. The size of the vagina is individual for each woman, but on average the depth of the vagina is 7-12 cm (not in a state of arousal). Smaller sizes can only occur with malformations of the genital organs or after operations when the vagina was sutured. Thus, a normal vagina can accommodate normal penises. What if the penis size is more than 12 cm? Then you need to take into account the fact that the vagina is elastic, which means it expands and stretches during sexual intercourse, adapting to the erect penis.
We will talk a little more about the size of the vagina using data from the Vagina Institute. Let me remind you that measurements of the external genitalia and vagina of women have been carried out (and are still being carried out) since 1995 and almost 900,000 women took part in the research.
In a non-excited (relaxed) state, the vaginal size is 7-9 cm in 78.34% of women. In an excited state, the size of the vagina increases to 13-19 cm, and in 86.96% of women it is 15-16 cm. Remember these numbers so that you can later compare them with the size of the penis, especially in a state of excitement.
With childbirth, especially rapid, large children, the size of the vagina, its elasticity, may change, and sensitivity during sexual intercourse may decrease. As studies show, the size of the vagina changes slightly only in a relaxed state - by the age of 60 its length increases by 1-2 cm, but in a state of arousal it remains almost unchanged.
The smallest vaginal sizes are in Australian and New Zealand women (15.9 cm when aroused), and the largest are in African women (17.03 cm when aroused). By country, Zambia, Tonga and Bermuda lead the way. Japanese women have the smallest size of an unexcited vagina.
There is a lot of talk among men about the fact that before pregnancy and childbirth, the vagina is smaller and “tighter.” To what extent is this true and not some speculation of men? The study showed that in single women, the vaginal size is 8.21 cm in a relaxed state and 16.3 cm in a state of arousal. In married women, many of whom have had pregnancies and childbirths, the vaginal dimensions are as follows: 8.52 cm in a state of relaxation and 16.55 cm in a state of arousal. Thus, the difference is only 2-3 mm, which is very insignificant.
The problem is most likely not in the size of the vagina, but in the fact that after childbirth the relief of the vaginal walls is slightly smoothed out. In addition, married women, having experience of sexual intercourse and childbirth, are able to relax better during intercourse and do not tighten the muscles of the vagina, as young women who have no experience of sexual activity often do. Most often, if you use certain sex positions and techniques, the sensations and pleasure you receive, including orgasm, do not change after childbirth. In addition, there are certain exercises to strengthen the muscles of the pelvis and perineum to improve the quality of sexual life. In extreme cases, you can resort to vaginal plastic surgery - surgical treatment of prolapse and prolapse of the vaginal walls.
The vaginal size of straight men and bisexuals is the same, but that of lesbians is slightly smaller, which is due to the fact that this category of women has fewer cases of pregnancy and childbirth.
It turns out that the size of an aroused vagina is directly proportional to a woman’s height. Therefore, we can safely say that the taller a woman is, the longer her vagina is when aroused. The dependence of vaginal sizes (average sizes) on height is shown in the table:
| Height (cm) | Relaxed vaginal size (cm) | Vaginal size in aroused state (cm) |
| Up to 139 | 8.0 | 13.97 |
| 140—149 | 8.08 | 14.88 |
| 150—159 | 8.28 | 15.55 |
| 160—169 | 8.4 | 16.57 |
| 170—179 | 8.33 | 16.77 |
| 180—189 | 8.31 | 19.46 |
| Above 190 | 8.0 | 20.73 |
From the above data it is clear that every additional 10 cm of growth “adds” approximately 1 cm to the size of the vagina in a state of arousal.
The structure of the vagina is such that its mucous membrane does not have special sensory nerve receptors, due to which a woman can feel pain and itching. Such symptoms appear only when the skin of the vaginal vestibule (vulva) is irritated by secretions, mechanical irritants (penis, instruments, fingers, vibrator, etc.) or chemical irritants (soap, washing powder, medicinal solutions, etc.). However, a woman may complain of pain and itching “inside”.
Pain may occur with strong contraction (spasm) of the muscles of the vagina and perineum. More than 60% of women have experienced or are experiencing pain during sexual intercourse, but in the vast majority of cases, pain occurs due to women’s inexperience in sexual relations, poor arousal and relaxation during sexual intercourse, and very rarely due to vaginal infections and inflammatory processes of the reproductive system . Painful sensations are often associated with a negative mental attitude (fear, reluctance) towards sexual intercourse, and muscle contractions are controlled by the woman’s consciousness. Therefore, most often such women need the help of a psychotherapist, sexologist, or psychiatrist.
If you are interested in women's health issues, read my articles and books on this topic (1000 questions and answers on gynecology (2017), Preparing for pregnancy (2012), Desk aid for pregnant women (2011), etc.).
To be continued…
Share link:
- Click to share on WhatsApp (Opens in new window)
- Click to share on Telegram (Opens in new window)
- Click here to share content on Facebook. (Opens in a new window)
- Click to share on Twitter (Opens in new window)
- Click to share on Skype (Opens in new window)
- Send this to a friend (Opens in new window)
- Click to print (Opens in new window)
By
Vaginal health
The female vagina is an amazing organ in every sense. It plays a role in sexual pleasure and is capable of giving birth to life. However, as you age, your vagina will change too. Having an aging vagina doesn't have to be a negative experience. Some women come to love their vaginas more than ever as they get older. For example, at 45-50+ you can feel more free during sex, due to the absence of the risk of unwanted pregnancy. And because with age comes wisdom, you may also feel more comfortable in your own skin and with your vagina.
During the period of age changes
You can't prevent every effect of aging on your vagina, but you can support it with some loving care and proper care and keep it as healthy as possible. Vaginal health can be maintained by following simple recommendations:
- undergoing regular gynecological examinations, including cervical screening,
- in situations of potential risk, we practice only “safe” sex,
- We regularly perform Kegel exercises at any age,
- We do not use douches, scented vaginal deodorants or vaginal cleansers.
What's good for a healthy vagina?
Follow these tips to reduce your risk of disease and maintain your vaginal health:
- Avoid unnecessary douching. The vagina naturally cleans itself. Douching can disrupt the natural balance of bacteria and fungi, which leads to the development of dysbiosis and vaginal infection.
- Avoid scented soaps and hygiene products. Perfumes in scented hygiene products such as soaps, pads and wipes can irritate the skin in the intimate area and disrupt the pH balance in the vagina. Choose products without strong odors.
- Be sexually responsible. Always use barrier protection (condom) with new partners and get tested for STIs regularly.
- Learn about Kegel exercises. They help strengthen the pelvic floor muscles, which can help reduce the risk of vaginal prolapse and pelvic floor weakness, as well as improve the sensation of intimacy.
- Get the Gardasil HPV vaccine. Ask your doctor about vaccination against viruses that can be sexually transmitted.
- Have regular medical examinations with a gynecologist. See your doctor for regular smear tests, screening for cervical cancer and HPV types.
Diseases of the vulva and vagina
Causes
- HPV. The main cause of the risk of vulvar dysplasia is determined by the human papilloma virus. HPV is one of the most widespread viruses, and more than 30 types pose a threat to women's health. Medical research has established that the greatest danger is posed by anogenital carcinogenic HPV-16 and HPV-18, which are responsible for the growth and appearance of genital warts - one of the distinctive symptoms of vulvar dysplasia (atypical hyperplasia).
- Inflammatory processes. Advanced inflammation of the genitals and vagina, characterizing colpitis, vulvitis or bartholinitis, are possible harbingers of vulvar dysplasia.
- Age indicators and associated factors. The presence of pathology of the vulvar epithelium can also be provoked by neuroendocrine changes and an imbalance of metabolic processes due to age-related changes. Along with menopausal hormonal imbalances, some associated factors contribute to the occurrence of dysplasia. These include weakened immunity, smoking, premature sexual relations, chaotic sexual intercourse and sexually transmitted infections.
The presence of these items in the patient’s medical history means that she is potentially at risk for the occurrence of vulvar dysplasia and is the basis for urgent contact with specialists in order to conduct a comprehensive diagnosis.
Diagnostics
- Inspection. The patient's examination begins with a visit to the gynecological office for an examination, which can be supplemented by extended colposcopy and the use of the Schiller test. Due to the different reactions of healthy and damaged epithelium to iodine, the Schiller test allows us to identify pathological changes in the epithelium. Iodine-negative tissues require mandatory cytological examination and biopsy, based on the results of which a final diagnosis is made.
- HPV test. Papillomavirus is one of the main factors inducing atypical hyperplasia, which necessitates HPV analysis if this pathology is suspected. HPV testing is carried out using the PCR screening method, which allows not only to establish the presence of human papillomavirus in the patient’s biomaterial, but also to accurately determine its type due to the unique DNA of each infectious agent. PCR screening is an effective research method even for indolent infections.
- Cytological examination, biopsy, histology. If atypical vulvar hyperplasia is suspected, a cytological examination of epithelial cells is prescribed, the results of which make it possible to judge the specificity and severity of cellular atypia, as well as the signs of malignant neoplasms. If the diagnosis is confirmed, in order to exclude a cancer threat, a biopsy with the histology of the selected material is required, the results of which make it possible to differentiate atypical vulvar hyperplasia from benign lesions of the vulva and oncological diseases.
A comprehensive examination with the involvement of specialists from different fields of medicine (in addition to a gynecologist and oncologist, it is advisable to involve a venereologist and a dermatologist in the examination) makes it possible to carry out the most comprehensive diagnosis and select effective methods to combat the disease that are tailored to the patient’s needs.
Sign up
Treatment of vulvar dysplasia
Vulvar dysplasia should be combated within the walls of the appropriate institution with the involvement of specialists of the necessary profile. Professional intervention will help avoid cancer complications and save life. Thanks to the availability of the latest equipment and an established team of professionals, the medical center offers a whole range of services for diagnosing and effectively treating vulvar dysplasia. The presence of an operating room and a day hospital provide access to various treatment methods, including surgery.
The key to curing vulvar dysplasia will be an individually oriented course. Get comprehensive advice from leading medical experts on women's health issues. Timely consultation, comprehensive diagnosis and effective treatment are the key to your recovery and well-being in the future.
Taking into account the age category, severity of atypia, contraindications and concomitant infections, there are various options for combating the disease:
- Conservative treatment. It involves the use of sedatives, hormonal therapy, desensitizing drugs, restoratives, as well as adherence to a certain diet. Focused on controlling the psychological state, leveling out local manifestations and achieving possible remission. A positive test for HPV requires additional antiviral and immunocorrective prescriptions.
- Surgical intervention. Severe pathology predetermines surgical intervention. An alternative may be the use of liquid nitrogen, radio waves, or laser removal of small lesions, but these options are only possible in the initial stages of the disease and are aimed at patients who have not reached menopause. In case of severe atypia, relapse or large-scale lesions and a clear risk of cancer, it is recommended to perform a superficial vulvectomy - a surgical operation to excise the upper layer of skin followed by plastic surgery.
- Organ-sparing methods. In the treatment of vulvar dysplasia complicated by HPV infection, photodynamic therapy can be used. The PDT method involves the use of light-sensitive substances that accumulate in the cells of tissue affected by the pathological process. Exposure to light with certain characteristics causes a chemical reaction, resulting in the death of atypical cells.
After surgical treatment, patients are subject to observation at the dispensary. Cytological control is required. It is recommended to abstain from sexual activity, refuse to use sanitary tampons and douches, and limit exercise.
Prevention and prognosis of vulvar dysplasia
Prognosis of vulvar dysplasia is related to the severity of the disease and the period of development of the disease, the presence of concomitant factors, age indicators and individual characteristics of the patient. In the absence of proper treatment, atypical hyperplasia can progress to oncological pathology. And a mild degree of dysplasia, when detected in the early stages and following the recommendations for appropriate treatment, successfully regresses.
The sooner a visit to a gynecologist follows and the more comprehensive the diagnosis, the more likely a successful recovery. Due to the possibility of relapse, patients with a similar diagnosis are recommended to undergo mandatory monitoring by their attending physician, and in particularly severe cases, additional monitoring by an oncologist.
It is possible to reduce the risk of disease and relapse through a healthy lifestyle, which includes good nutrition and giving up bad habits. Special attention should be paid to barrier contraceptives and sexual activity. A prerequisite for recovery and monitoring a woman’s health condition is further regular visits to the gynecologist.