Unpleasant sensations in the genital area that a woman feels are subjective and can have various manifestations. Discomfort in the vagina can be understood as itching, burning, unusual discharge from the genital tract, rashes, and unpleasant odor. To determine the causes of such symptoms, a gynecological examination, laboratory and instrumental studies are necessary.
Etiology of vaginal discomfort
The relevance of the problem of vitamin B9 deficiency is due to its extreme importance for normal human life. The functions of folic acid include the following:
Gynecological diseases can cause discomfort:
- vaginal candidiasis (thrush);
- bacterial infections (vaginitis, vulvovaginitis, colpitis);
- STIs (herpes, chlamydia, ureaplasmosis, mycoplasmosis, trichomoniasis, condylomas); involutional changes associated with menopause (kraurosis of the vulva, atrophy of the vaginal lining, etc.).
Discomfort in the vagina can be caused by diseases not related to the reproductive system, including:
- diabetes;
- intestinal dysbiosis;
- cystitis;
- diseases of the kidneys, liver, thyroid gland;
- allergy;
- infection with helminths and protozoa, etc.
Physiological factors that can cause discomfort in the vagina include physical and emotional stress, hypothermia/overheating, taking certain medications, weak immunity, pregnancy, and poor nutrition. As well as non-compliance with personal hygiene rules, individual intolerance to the composition of intimate hygiene products, allergies to latex and intimate lubricants, wearing low-quality underwear.
Infections
Pathogenic microbes, viruses and fungi constantly attack a woman’s body. Insufficient or improper genital hygiene, frequent changes of sexual partners, constant wearing of thongs - all this can contribute to the appearance of infection in the vagina.
Many women don't even realize that washing from back to front contributes to the development of a bacterial infection. During this process, E. coli enters the vagina from the rectum. As a result, these bacteria cause inflammation and stabbing pain in the intimate area.
The same thing happens with thongs. A thin strip at the back, fitting the buttocks, transfers harmful microorganisms from the rectum to the vagina. That is why lovers of such underwear often feel a slight tingling sensation in the crotch.
Frequent change of partners is one of the main reasons for the appearance of infection in the mucous membrane of the female genital organs. Men who do not pay enough attention to intimate hygiene are carriers of pathogenic microbes. These harmful microorganisms, entering the vaginal mucosa, cause inflammation, pain and itching.
How does vaginal discomfort manifest?
Signs of diseases are:
- itching in the labia minora and labia majora;
- discharge with an unusual color and odor;
- rashes on the labia;
- feeling of dryness in the vagina;
- feeling of a foreign object;
- increased urge to urinate;
- painful intercourse;
- swelling and redness of the external genitalia.
Why pain occurs during intimacy: the main reasons
The appearance of strong discomfort during sex prevents a woman from enjoying the process and can lead to a number of health problems. Only a specialist can establish a reliable diagnosis based on the clinical picture, examination and diagnostic results. Below is a list of the main reasons that can cause pain during intimacy.
Vaginal dryness
Lack of sufficient vaginal moisture can be caused by short foreplay or its complete absence. Hormonal imbalance or taking medications can negatively affect the condition of the mucous membrane. Such medications include psychotropic and sedative drugs, and incorrectly selected oral contraceptives. And also vaginal dryness is often observed in women during menopause and after childbirth due to a decrease in the production of female sex hormones (estrogens)
In such situations, you should pay more attention to foreplay and additionally use special intimate gels or lubricants.
ENDOMETRIOSIS
Endometriosis is a pathology in which cells of the endometrium (the inner layer of the uterine wall) grow outside of it. During the menstrual cycle, endometriotic lesions undergo the same changes as the uterine mucosa (bloody discharge during menstruation and pain before it). The disease can cause intense pain during urination and sex in the lower abdomen. It can be diagnosed using an ultrasound of the pelvic organs. Treatment is prescribed individually depending on the patient’s age and clinical picture.
SEXUALLY TRANSMITTED INFECTIONS (STIs)
Pain during intimacy in women can be caused by pathogenic microorganisms. Most often, this symptom is observed with gonorrhea, chlamydia and genital herpes. In addition to pain, the patient may experience a strong burning sensation in the external genital area, unusual discharge (bloody, purulent) and deterioration in overall health.
Contraception (condoms) can protect you from contracting STIs. If you suspect a sexually transmitted infection, it is important to immediately undergo appropriate tests. Without timely treatment, the pathogenic microorganism can spread to other organs and lead to negative consequences that reduce a woman’s quality of life.
PROBLEMS OF PSYCHOLOGICAL CHARACTER
A strong fear of sexual intercourse can lead to uncontrolled tension of the pelvic floor muscles during the process. This creates a barrier to internal penetration. As a rule, such feelings arise before the first intimacy with a new sexual partner. For some girls, fear is due to more serious reasons, for example, sexual violence and harassment. Because of this, the body cannot relax and sex causes nothing but discomfort.
Another psychological problem is low self-esteem. If a girl is unsure of herself and could not accept her body, painful sensations may appear during sex. You should try to relax as much as possible and drive away the feeling of awkwardness. If you cannot solve the problem yourself, it is important to seek help from a specialist. Sessions with an experienced psychologist will help you cope with feelings of fear and anxiety.
ATROPHY OF THE MUSCLES OF THE VAGINA
Vaginal atrophy is the thinning and inflammation of its walls due to a decrease in estrogen levels. As a rule, it appears after menopause, but can develop during breastfeeding, against the background of radiation therapy and chemotherapy for cancer. Most women who suffer from vaginal atrophy experience severe discomfort during sexual intercourse, which leads to decreased interest in sex. In addition, other symptoms that may bother you:
- burning sensation during urination;
- slight bleeding after sexual intercourse;
- vaginal discharge.
Vaginal atrophy, which is caused by menopause, can manifest itself 4-6 years before its onset. However, changes in the vagina may not occur for several years after the onset of menopause. Regular sex life allows you to keep tissues healthy.
INJURIES AND SURGICAL INTERVENTIONS
Injuries from an accident or surgical intervention can lead to painful sensations during sexual intercourse. After any planned operation, the doctor informs the patient about the rules of the rehabilitation period. In most cases, one of these rules is sexual rest. If it is not followed, both pain and bleeding may occur.
Girls who have undergone surgical dissection during childbirth often experience pain during intimacy. This is due to the fact that the wound has not yet fully healed. The pain goes away on its own after 2-3 months.
COLPITIS AND VULVOVAGINITIS
Acute pain during sex can be caused by an infectious and inflammatory process of the vulva and vagina. As a rule, discomfort occurs at the very beginning of intimacy, when attempting to insert the penis. This is directly related to irritation and swelling of the mucous membrane of the external genitalia.
Other symptoms indicating the presence of colpitis and vulvovaginitis include profuse vaginal discharge with a characteristic odor, itching and burning. As a rule, treatment requires taking a course of antibiotics and antifungal agents (prescribed on an individual basis).
BENIGN AND MALIGNANT NEOPLOGMS (TUMORS AND CYSTS) OF THE OVARIES OR CERVIX.
Ovarian tumors and cysts can occur in girls of different age categories. Cysts are often diagnosed; they are benign neoplasms filled with fluid. With small sizes, the symptoms may not bother you, however, in most cases, girls experience:
- bleeding (not associated with menstruation);
- disturbances in the duration and intensity of menstruation;
- painful sensations in the lower abdomen during physical activity.
In addition, if there are tumors in the ovaries, girls may experience aching and nagging pain both during and after sex. In addition, with sudden insertions of the penis, complications may develop - torsion of the leg or rupture of the cyst. This is accompanied by the appearance of sharp pain in the lower abdomen, pale skin and a feeling of nausea; it is important to immediately call an ambulance. in
Pain during sexual intercourse also appears in the presence of malignant neoplasms of the cervix. It is especially pronounced in the second and third stages. After sex, spotting often appears.
INFLAMMATION OF THE BLADDER (CYSTITIS)
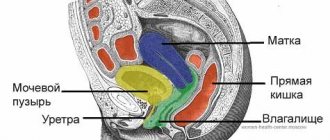
Cystitis is a common pathology characterized by frequent urge to urinate and pain during it. Also, inflammation of the bladder is accompanied by pain during sexual intercourse. This is directly related to the immediate location of the bladder and the uterine wall. Due to their close contact, the woman experiences pain. Cystitis can be infectious or non-infectious. If, based on the results of the analysis, it is determined that there is no pathogenic microflora in the urine, we are talking about interstitial cystitis.
This pathology is a chronic inflammation of the bladder for no apparent reason. Painful sexual intercourse is its main symptom. To eliminate it, doctors often prescribe oral medications and resort to cystoscopy with stretching of the bladder wall.
Diagnosis for vaginal discomfort
With similar symptoms, women turn to a gynecologist. The doctor collects anamnesis and clarifies the nature of the discomfort. Next, he conducts a gynecological examination, takes smears for analysis of microflora, bacteriological culture, cytology (the cellular composition of the epithelium of the vagina and cervix is studied).
To clarify the causes of discomfort in the vagina, clinical and biochemical blood tests may be prescribed (to identify signs of an inflammatory process), colposcopy (visual examination of the inner surface of the genital tract using a colposcope), biopsy (sampling of material from a pathological lesion for histological and cytological analysis). During the diagnosis, attention is also paid to changes in the acidity and composition of the vaginal microflora.
How is a gynecologist examined?
At the Alan Clinic medical center, gynecological examinations are performed in comfortable conditions, using disposable sterile instruments. The initial appointment takes 40 minutes.
The initial examination by a gynecologist includes a standard gynecological examination, including:
- conversation with a doctor
- smear of vaginal discharge to determine the degree of purity
Depending on the clinical symptoms and complaints, the gynecologist may prescribe additional examination methods.
- scraping from the cervix for oncocytology
- Ultrasound of the pelvic organs
- extended colposcopy
- study for tumor markers CA-125, CA-15-3
Treatment of diseases causing discomfort in the vagina
The procedure for eliminating unpleasant symptoms depends on the type of disease that was identified during diagnosis. If discomfort in the vagina is associated with physiological reasons, then the influence of the provoking factor must be eliminated. If discomfort accompanies menstruation or pregnancy, you must wait until it is over.
- antibacterial;
- antifungal;
- antihistamines;
- hormonal;
- anti-inflammatory, etc.
In most cases, conservative treatment methods are sufficient to eliminate the problem.
30 working days
Gut microbiome
12000 ₽
More details
Other factors
Neuralgia
If the pelvic nerves are cold or inflamed for another reason, the pain may be felt in the hips and legs. With neuralgia of the pelvic nerves, a woman experiences discomfort from friction, especially when in an uncomfortable position.
Cystitis
Aching, sharp pain in the lower third of the abdomen - this is how inflammation in the bladder area manifests itself. During coitus, discomfort in the vagina and abdomen may intensify.
Venous blood stasis
Due to blood thickening due to an imbalance of vitamins, microelements, hormonal imbalances, and a sedentary lifestyle, a nagging pain in the lower abdomen may occur. Sex with venous stagnation of blood can be uncomfortable, and, even if there is no pain, it is much less likely to lead to orgasm - due to impaired blood circulation.
Psychological reasons
Lack of self-confidence, negative experiences in past relationships, fear of coitus, reluctance to have sexual intercourse with this partner - these and other factors affect the quality of sex and its possibility in general. The psychological state affects the amount of lubricant released and can lead to involuntary contraction of the vaginal muscles. Even in the absence of muscle spasms and with sufficient lubrication, sex can feel traumatic and uncomfortable.
Preventing vaginal discomfort
In order to maintain women's health, you should follow the recommendations:
- eat right;
- to live an active lifestyle;
- carefully choose personal hygiene products;
- avoid hypothermia and overheating;
- try to avoid emotional and physical overload;
- wear underwear made from natural fabrics;
- avoid unprotected sex;
- undergo regular medical examinations and promptly treat gynecological diseases.
In medical genetics, you can perform an examination of the female reproductive system.
Postpartum problems
Childbirth is a lot of stress for a woman’s body. If the expectant mother has not prepared the vaginal muscles for the upcoming birth, a tear of the uterosacral ligaments may occur. As a result, severe tingling may occur in the area of the perineum.
Often, after severe physical stress during childbirth, a woman experiences inflammation of the uterine cavity - endometritis. In some cases, endometritis is accompanied by an inflammatory process in the appendages - salpingo-oophoritis. Such diseases can also cause discomfort and sometimes pain in the perineum.
These ailments arise due to:
- insufficient processing of medical instruments used during childbirth;
- improper performance of intimate postpartum hygiene;
- hypothermia.
Doctors sometimes perform an episiotomy on a woman during childbirth. So, these are the names of the special incisions necessary to remove a large child. In this case, special sterile instruments are used. If the devices were processed incorrectly, the woman develops inflammation in the appendages or uterus. Because of this, pain and irritation in the vagina often occur.
After childbirth, a woman should carefully monitor her intimate hygiene. To prevent inflammation of the appendages or uterine cavity, doctors recommend that women after childbirth treat the vagina with hydrogen peroxide, brilliant green or other antiseptic solution.
In the first days after birth, attend special physiotherapy procedures and wash yourself with warm water and a solution of potassium permanganate.
A new mother should avoid hypothermia. That is why, immediately after giving birth, a woman should beware of drafts, walking barefoot on linoleum and other potentially dangerous “cold procedures”.
Neoplasms
Sometimes women may develop a cyst on the ovary. This neoplasm often occurs as a result of blockage of the gland that synthesizes lubricant. In this case, surgery is performed.
In some cases, polyps appear in the uterus; the reasons for this phenomenon may be different, but most often this is facilitated by a violation of the hormonal system. Doctors include the development of adnexitis and endometritis, as well as abortion, as predisposing factors.
The main cause of polyps in the uterus is the synthesis of large amounts of estrogen, which stimulates the enlargement of the endometrium. As a result, growths appear, which are called polyps.
Such pathologies are often accompanied by pain, bleeding, bleeding, and infertility. Treatment is expected to be surgical.
Sources
- Hou C., Zheng J., Li Z., Qi X., Tian Y., Zhang M., Zhang J., Huang X. Printing 3D vagina tissue analogues with vagina decellularized extracellular matrix bioink. // Int J Biol Macromol - 2021 - Vol180 - NNULL - p.177-186; PMID:33737175
- Tchuenkam LW., Mbonda AN., Tochie JN., Mbem-Ngos PP., Noah-Ndzie HG., Bang GA. Transvaginal strangulated bowel evisceration through uterine perforation due to unsafe abortion: a case report and literature review. // BMC Womens Health - 2021 - Vol21 - N1 - p.98; PMID:33663467
- Park SY., Lee ES., Lee SR., Kim SH., Chae HD. Vaginal Microbiome Is Associated With Vulvodynia, Vulvar Pain Syndrome: A Case-Control Study. // Sex Med - 2021 - Vol9 - N2 - p.100314; PMID:33652201
- Aldrich ER., Pauls RN. Benign Cysts of the Vulva and Vagina: A Comprehensive Review for the Gynecologic Surgeon. // Obstet Gynecol Surv - 2021 - Vol76 - N2 - p.101-107; PMID:33625519
- Wang J., Wang L. The therapeutic effect of dehydroepiandrosterone (DHEA) on vulvovaginal atrophy. // Pharmacol Res - 2021 - Vol166 - NNULL - p.105509; PMID:33610719
- Pokhrel D., Bhattarai S., Emgård M., von Schickfus M., Forsberg BC., Biermann O. Acceptability and feasibility of using vaginal menstrual cups among schoolgirls in rural Nepal: a qualitative pilot study. // Reprod Health - 2021 - Vol18 - N1 - p.20; PMID:33487171
- Elbaz M., Qadiry RE., Fouraiji K., Jalal H., Elhoudzi J. Yolk sac tumor of vagina: a rare cause of vaginal bleeding in adolescents—a case report. // Pan Afr Med J - 2021 - Vol37 - NNULL - p.169; PMID:33425202
- Kamal E.M., Lakhdar A., Baidada A. Management of a transverse vaginal septum complicated with hematocolpos in an adolescent girl: Case report. // Int J Surg Case Rep - 2021 - Vol77 - NNULL - p.748-752; PMID:33395888
- Wang J., Yang Z., Li W. Deciphering the Role of Human Gastrointestinal Microbiota in the Pathogenesis of Vaginal Infection and Cervical Cancer. // J Environ Pathol Toxicol Oncol - 2020 - Vol39 - N4 - p.365-373; PMID:33389908
- Mat E., Kale A., Yıldız G., Başol G., Gündogdu EC. Alternative method for the diagnosis of acid cases of unknown cause: Transvaginal natural orifice transluminal endoscopic surgery. // J Obstet Gynaecol Res - 2021 - Vol47 - N2 - p.645-652; PMID:33197989
Expert opinion
The diagnosis of colpitis “gets younger” every year. The reason is not only the early onset of sexual activity in girls, but also the modern fashion for underwear. A patient comes to see a doctor with characteristic complaints, and we immediately pay attention to her clothing. Beautiful, lacy synthetic underwear, fashionable thongs do not allow air to pass through and cause a local increase in temperature. This is an ideal environment for bacteria to multiply. If constant wearing of such underwear is accompanied by insufficient intimate hygiene, the girl is almost guaranteed to get bacterial colpitis. You can wear thongs and lace, but only for a short time and on special occasions. The rest of the time, you should take care of your health and choose cotton underwear that will not rub the perineum and will not cause overheating.
Anomalies of the vaginal structure
Under the influence of negative factors, the structure of the genital organs may undergo changes. The walls of the vagina may become thinner or thicker, and they may droop, especially during labor complications. In this case, drug treatment with the use of hormones is carried out, sometimes surgery may be required.
As a woman ages, certain changes occur in her body. Sex hormones are synthesized in insufficient quantities, which can cause the development of kraurosis of the vulva, when the vaginal mucous epithelium atrophies. In this case, a stabbing pain may also appear.
Etiology of colpitis
Normal vaginal microflora includes dozens of types of microorganisms that can live and reproduce in this environment without causing disease. This is a flexible biocenosis that can quickly adapt to changes and suppress the excessive development of opportunistic microbes - such processes are called colonization resistance.
Under the influence of various external and internal factors, the balance of vaginal microflora can be disrupted. The number of lactobacilli decreases, which, in turn, leads to a change in the acidity of the environment and creates favorable conditions for the development of pathogens. Inflammation occurs.
The main infectious agent may be staphylococcus, Escherichia coli, streptococcus, fusobacteria, non-spore-forming anaerobes, peptostreptococci or other bacteria. But in recent years, vaginitis has been characterized by a mixed etiology, when inflammation is caused by the activity of several types of microbes. This significantly complicates treatment, increases the risk of relapse of the disease, and contributes to the transition of acute colpitis to chronic.
Inflammatory processes in the genital organs
Most often, pain occurs due to the development of infection and various female diseases. This is due to the fact that the tissues and mucous epithelium of the vagina are quite thin, so they can change. The most common diseases that cause pain include:
- Colpitis. The pathology is manifested by inflammation of the vaginal mucous epithelium due to infections, tissue changes due to age, and damage. In this case, the woman experiences stabbing pain in the vagina, the causes of which will be accurately determined by a doctor, as well as swelling of the area, and unpleasant discharge with purulent contents. Sometimes the discharge may be mixed with blood. When diagnosing colpitis, maintenance therapy is carried out aimed at restoring microflora and increasing the body's defenses. The doctor often prescribes douching with antiseptic drugs.
- Bartholinitis. This pathology is an inflammation of the gland that synthesizes lubricant. Pain occurs in the perineal area, discharge mixed with pus, and swelling of the mucous epithelium may appear. Women may experience a rise in body temperature, chills and fever. Without treatment, an abscess begins. Treatment should be carried out with the use of antibacterial drugs, analgesics and antiseptics.
- Vaginitis has similar symptoms to colpitis.
Popular questions
Hello!
After intercourse, there was discomfort, then I saw that there was blood, it turned out that there was an ulcer on the vaginal mucosa and it was bleeding. I treated it for a few days and everything went away. Two weeks later, heavy bleeding appeared from the wound, what could it be? Hello! I recommend that you see a specialist and be examined for infections on the surface of the wound - a PCR test for genital herpes, blood for syphilis. If STIs are excluded, to prevent injuries to the mucous membranes of the genital tract, you can use Ginocomfort gel with mallow extract. This will not only have the effect of additional hydration, but will also prevent injury to the mucous membranes.
Good afternoon, I often experience discomfort during sexual intercourse and, in principle... Lubricant is not released or it simply dries on the outside to the point of pain. I bought a gel with mallow, used it twice so far, but both times after administration, after some time it curls up inside, white flakes and a little water come out... Is this a normal effect or should I stop? Thank you
Hello! The appearance of such manifestations when using Gynocomfort gel with mallow is a variant of the norm. If the use of the gel eliminates the moisture deficiency, then you can use it in the future.
Hello. I have a little problem during sex. My boyfriend has a large penis for me and during sex there is a burning sensation, I begin to feel dryness towards the middle or towards the end of the process. This is my first boyfriend. Tell me, what is the problem and is it worth going to the doctor?
Hello! Try to eliminate this problem by using additional moisturizing agents - lubricants. Ginocomfort gel with mallow extract is suitable for this purpose. It contains not only moisturizing components, but also regenerating and anti-inflammatory substances. The gel is administered in 1 dose before contact in the genital tract, and can also be applied topically to the mucous membranes of the vaginal vestibule. The duration and frequency of use is not limited.
Good afternoon, during sex, sometimes with a condom, sometimes without, I feel a burning sensation in the vagina, what do you recommend?
Hello!
Most often, such sensations appear due to insufficient hydration in the genital tract, so use an additional lubricant before contact. For this purpose, the use of Ginocomfort gel with mallow extract is suitable. A distinctive feature from other similar products is that it contains components. having an anti-inflammatory, regenerating effect in case of microtrauma of the mucous membranes. The gel is introduced into the genital tract using an applicator immediately before contact. For an accurate diagnosis, contact a specialist
Therapeutic measures
Pain in the vagina is not treated, treatment is carried out for the underlying disease that caused the appearance of such a syndrome. The treatment regimen is prescribed in each specific case based on the disease, age and individual characteristics of the patient’s body. In some cases, the doctor prescribes antibacterial drugs, antiseptic douching solutions, and hormonal agents. In other cases, surgery may be required.
Doctors strongly recommend not to self-medicate, as this can only worsen the problem. It is unacceptable to use heating pads or prescribe medications on your own. Treatment should only be carried out by a doctor. When the first unpleasant symptoms appear, you need to go to the clinic. Otherwise, complications may arise. Thus, in the absence of therapy, bartholinitis can provoke the appearance of cysts, and endometriosis can cause a cancerous tumor.
Treatment
How to cure inflammation of the female genital area?
Treatment should be carried out under the full supervision of the attending physician and include several stages (parallel implementation of these therapeutic measures is possible):
- Elimination of unpleasant symptoms of the disease.
- Comprehensive treatment of the causes of the disease.
- Treatment of the sexual partner (if necessary).
- Strengthening the immune system.
- Treatment of other diseases of the female genital area (if necessary).
- Adjustment of the patient’s lifestyle and nutrition.
- Development of an individual prevention program.
- Monitoring the patient's condition after treatment.
Complex treatment may include the use of the following methods:
- Drug treatment
. Prescribed in accordance with test results. - Local treatment
. Sanitation of the vagina followed by application of a tampon with a medicinal drug, incl. Ultrasonic sanitation with the Gineton apparatus. - Radio wave treatment
. Non-contact incision of soft tissues using high-frequency radio waves (3.8-4.0 MHz) with the Surgitron device. - Physiotherapy
. Modern Androgyn and Mustang equipment is used, which are successfully used in the complex treatment of inflammatory diseases, hormonal disorders, as well as recovery in the postoperative period. - Pharmacopuncture
. Introduction to acupuncture points of medicinal substances that are indicated for various diseases (inflammatory, hormonal disorders, etc.). - Ozone therapy
. Intravaginal and intravenous administration of drugs enriched with ozone contributes to the development of a powerful antioxidant effect, which can successfully cure inflammatory diseases, improve the immune system and reactive capabilities of the body. - Hirudotherapy
. Widely used in the treatment of diseases such as endometriosis of the uterus and ovaries, inflammatory diseases, hormonal dysfunctions, infertility, etc.
Symptoms and signs
The nature of the pain may vary. The pain can feel like needle pricks and sometimes gets worse over time. Severe pain causes discomfort and forces you to change your body position. There may be a feeling of the presence of a foreign body and heaviness in the groin area. Also, discomfort may be accompanied by other symptoms:
- Pathological discharge. They may have an unpleasant odor and a yellow, brown or green tint.
- Heaviness in the abdominal area.
- Weakness and increased fatigue.
- Increase in body temperature.
- Development of bleeding.
If any of the signs appear, it is recommended to get a free consultation with a gynecologist by phone, or it is best to go to a medical facility in person.
Gynecologist's advice on pain during sex, video
is not responsible for the accuracy of the information presented in this video clip.
Source - Live Healthy! Sources:
- ORGANIC AND PSYCHOSOMATIC DYSPAREUNIA (COMPARATIVE ANALYSIS). Fedorova A.I. // Russian family doctor. – 2006. Series “Original Scientific Research”. – pp. 21-25.
- INTERDISCIPLINARY APPROACH TO THE THERAPY OF DYSPAREUNIA. Fedorova A.I. // Journal of Obstetrics and Women’s Diseases 2006. – No. 4. – P. 101-104.
- Functional female sexopathology. Zdravomyslov V.I., Anisimova Z.I., Libikh S.S. // Alma-Ata: Kazakhstan. - 1985. - P. 272.
- Clinical and physiological basis of psychosomatic relationships. Gubachev Yu.M., Stabrovsky E.M. // L.: Medicine. - 1981. - P. 214.
- Differentiated pathogenetic approach to the treatment of dyspareunia. Fedorova A.I. // Russian family doctor.— 2005.— No. 2.— P. 22–27.
- https://ru.wikipedia.org/wiki/%D0%91%D0%BE%D0%BB%D0%B5%D0%B7%D0%BD%D0%B5%D0%BD%D0%BD%D1 %8B%D0%B9_%D0…