A person with a vagina will face a number of problems related to its health throughout his life. And vaginal dryness is the most common of all. We women know how uncomfortable this can be to live with and deal with constantly. What's even more unfortunate is the fact that it can cause even more problems if left untreated. Don't know what to do with a dry vagina? Here are the three main causes of dry vagina in girls, why it happens and how to deal with it...
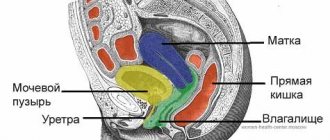
Your vagina is a smart and rational organ! In addition to its self-cleaning and self-regulating mechanism, it has walls coated with moisture for protection and lubrication during sexual intercourse. Many factors can cause this mucous membrane to become thinner or less hydrated. Both can lead to vaginal dryness and burning, characterized by intense discomfort down between the legs.
Signs of dry vaginal skin
Itching and burning in intimate places
If the bikini area is itchy, this in any case indicates a violation of its natural environment: the cause may be an allergic reaction, inflammation, external irritants, or, what is most often the cause, a failure of the acid-base balance.
Expert opinion
The normal level of vaginal acidity in a woman of reproductive age is 3.8-4.5: that is, it is acidic. However, it must be taken into account that the pH balance is not a constant value; it depends both on internal metabolic processes, including hormone levels, and on external factors, such as the type and material of underwear, the intimate hygiene product used, etc.
Obstetrician-gynecologist of the highest category Oksana Anatolyevna Gartleb
Why does itching and dryness occur in the intimate area?
A decrease in vaginal secretion leads to vulnerability of the mucous membranes, which means the formation of microcracks and wounds that cause itching.
Of course, these signs can indicate not only dry skin in the intimate area, but also hundreds of other delicate troubles, even an infectious disease. However, if traditional therapy does not help get rid of discomfort, try paying attention to intimate skin care. For example, the GINOCOMFORT Moisturizing washing gel fights the external manifestations of vaginal dryness. It contains hyaluronic and lactic acids, which restore the natural pH balance and normal moisture of the female genital organs.
Frequent urination
This symptom is especially common in women aged 55+, when the pelvic floor muscles lose their elasticity, which can lead to mild incontinence and a more frequent urge to urinate. Dryness in the intimate area aggravates changes in the female body during the climatic period, often complementing urination with symptoms reminiscent of acute cystitis: burning after emptying the bladder, pain, persistent irritation.
Pain from dry skin in the intimate area
Discomfort when wearing tight things
Tight clothes, especially rough seams on them that touch the perineum, can really irritate the already vulnerable dry skin of the intimate area, so women with vaginal dryness often find it difficult to spend the whole day in trousers. In addition to the mechanical impact, clothing that fits tightly to the intimate organs, especially made from artificial materials, disrupts natural air circulation. As in a room without long-term ventilation, harmful microorganisms begin to linger and multiply with greater comfort in microcracks. If you regularly feel that tight clothes are pressing on your delicate areas, you most likely have dry skin.
Expert opinion
The best option for daily wear are panty models such as slips, culottes, tangas, shorts, with a gusset made of natural material (ideally cotton). At the same time, it is advisable to abandon thongs and thongs.
Obstetrician-gynecologist of the highest category Oksana Anatolyevna Gartleb
Dryness and burning in the intimate area when wearing trousers
Pain and slight bleeding during intercourse
According to Doctor of Medical Sciences, obstetrician-gynecologist Rimma Antonova, the reason for refusal of sex among women over 45 years of age in most cases is not their personal desire, but pain and severe discomfort during sexual intercourse[2]. Hormonal changes and replacement of the slightly acidic environment of the vagina with a more alkaline one does not allow a woman to enjoy intimacy with her partner, giving a burning sensation. Often, a decrease in the volume of natural secretions leads to microtraumas of the mucous membrane of the vaginal walls, which causes mild local bleeding. However, the joy of sexual intercourse can also be experienced during menopause: it is enough to use GINOCOMFORT intimate gel lubricant during sex. The product contains hyaluronic acid, which helps replenish the lack of natural vaginal secretions and moisturizes the vaginal walls.
However, the joy of sexual intercourse can also be experienced during menopause: it is enough to combine the washing gel GINOCOMFORT Moisturizing and moisturizing gel, which can be used as a lubricant. The composition of GINOCOMFORT products is as close as possible to the natural microflora of the vagina, and the natural antiseptics in the composition will accelerate the healing of small cracks and abrasions.
Painful sensations due to dryness in the intimate area
Pain and general discomfort
Dry skin, due to its high irritability, can cause discomfort throughout the day, for example, if you sat for a long time or, on the contrary, walked for several hours in tight underwear. Vaginal dryness is often accompanied by a not very pleasant, pungent odor of discharge, which is quickly absorbed into the underwear and reduces its freshness. Trying to take care of themselves, women suffering from this delicate problem begin to wash themselves more often using aggressive detergents, but this only increases dryness. In this case, of course, it is important to take a shower regularly, but it is better to use the washing gel no more than 1-2 times a day, and the rest of the time, use hypoallergenic panty liners or, in extreme cases, wash with clean water without additional products. It is also important to exclude infections or inflammation in the acute stage in the intimate area.
Dryness and discomfort in the intimate area in women
Reducing the volume of secretions
Vaginal discharge is natural for a woman at any age and reproductive status; normally it is 2-4 ml. If its quantity has decreased or you do not notice it at all, this is a reason to consult an obstetrician-gynecologist - temporary comfort can result in irritation and pain caused by dryness of the vaginal mucosa.
Types of pathology
Doctors divide the anomaly into types for reasons. In this case, the outpatient card indicates: “vaginal dryness against the background...”. Gynecologists also determine the degree of reduction in natural lubrication, however, such a classification is conditional and depends on many additional factors: the time of the test, the food taken before the examination and test.
The main classification for pathology is by age. For patients over 50 years of age with vaginal dryness, the term vulvovaginal atrophy is provided. An anomaly means structural destruction, wrinkling of the mucous membrane. It is also associated with low estradiol levels.
Causes of itching and dryness in the intimate area
Decrease in estrogen levels
The key reason for dryness in the intimate area, which doctors diagnose, is hormonal disorders associated with changes in reproductive status or the onset of menopause. During these periods, the level of female hormones estrogen decreases, which leads to a decrease in discharge and dryness of the vaginal mucosa.
Recent genital surgery
Any surgical intervention, even if it is cosmetic in nature, affects the vaginal microflora, especially if the obstetrician-gynecologist prescribes antibiotics. During the period after surgery, a woman may experience dryness and irritation in the intimate area, but if she is healthy, within a week the comfortable sensations will return and the skin will be restored.
Why is there dryness in the intimate area after surgery?
To speed up rehabilitation, especially if you are prone to dryness, itching and irritation in the intimate area, obstetricians and gynecologists recommend washing yourself daily with intimate hygiene gel with natural ingredients. GYNOCOMFORT Moisturizing washing gel is excellent for daily use in the postoperative period, as it contains the equivalent of lactic acid, which restores the natural microflora of the vagina and acts as a barrier to external microorganisms and infections. Created by specialists from the pharmaceutical company VERTEX, the gel is safe for use and has all the necessary documents and certificates.
Women's health disorders
Dryness and burning in the intimate area are frequent accompaniments of infections and inflammations of the external or internal genital organs. Some of these diseases, for example, candidiasis, can be easily treated at home, while other diseases, such as salpingitis, vulvovaginitis (inflammation of the vaginal mucosa), etc. require consultation and treatment with obstetricians and gynecologists. In addition to inflammatory processes, dryness of the intimate mucosa can be a consequence of hormonal imbalance - in this case, you need to get tested, and an obstetrician-gynecologist will prescribe individual hormone replacement therapy.
Age-related hormonal changes
Doctors are well aware of the diagnosis “atrophic vaginitis” (Vaginitis). During menopause and after the onset of menopause (Climax), the production of estrogen is reduced, causing the vaginal epithelium to become thinner and the vaginal folds to become smoother. This leads to periodic bleeding, dryness and prolonged healing of inflammatory processes. [3]
Dry skin in intimate areas during menopause
Properly selected treatment restores the natural hormonal balance of the vagina, and the effect of treatment can be consolidated by daily use of the GINOCOMFORT Moisturizing washing gel. The AQUAXYL complex in its composition maintains optimal moisture in the mucous membranes of the intimate organs, and sodium lactate helps to resist the proliferation of pathogenic bacteria.
Consequences of radiation therapy [4]
If a woman is undergoing radiation therapy, she may experience burning, dryness, and vulnerability of the genital mucosa. These symptoms are temporary, but despite this, you should definitely tell your doctor about them. In addition, during the period after radiation therapy, you must definitely consult with an obstetrician-gynecologist about intimate cosmetics: during the recovery period, unwanted reactions to the active components contained in hygiene products are possible.
Dry burning in the intimate area after radiation therapy
Using inappropriate cosmetics for intimate care
This is not the first time we have said that a hypoallergenic detergent for dryness in the intimate area with lactic acid and natural extracts in its composition is the basis of women’s health and daily maintenance of intimate organs clean.
It is very important to use cosmetics with a low content of aggressive chemical ingredients so as not to disturb the natural acid-base balance of the vagina and not provoke allergies or irritation.
If you feel discomfort from using your cosmetic product, and your skin has become dry or sensitive, try first to choose a suitable intimate gel. You may need to visit your doctor to determine which component is causing the adverse reaction.
Proper care of the intimate area is important
Approaching menstruation
Some women note that 2-3 days before the start of menstruation, burning and itching is felt in the intimate area. This may be due to changes in hormonal levels. Discomfort can be corrected by using GINOCOMFORT Moisturizing intimate gel with mallow, as well as by keeping the intimate area clean and wearing loose underwear made of natural fibers. The named product underwent clinical studies conducted at the Department of Dermatovenereology with the clinic of the St. Petersburg State Medical University under the leadership of Ignatovsky A.V. and Sokolovsky E.V. Testing of the gel showed that it is well tolerated by women, does not cause allergic reactions, and also has pronounced moisturizing properties.
Side effect of contraception
If, after sexual intercourse using a condom, you regularly feel the familiar symptoms of burning, itching, dry skin and mucous membrane in the vestibule area, you may have an allergic reaction to latex.
In some cases, allergies may arise from the use of low-quality lubricants or sex accessories made from questionable materials.
If irritation occurs, you should visit a doctor to clarify the diagnosis and eliminate dryness and discomfort from the genital tract.
As you can see, the causes of dryness and burning in the intimate area in women are varied, and this unpleasant symptom can occur in almost everyone. However, according to gynecologists, most often pregnant women and women who have recently given birth, as well as women during menstruation, complain of dryness and burning in the vagina. Why are these cases so frequent, and how are unpleasant sensations related to what is happening in the female body?
Dry mucous membranes in the intimate area due to contraception
Video
After the examination, 15 ml of blood is drawn. To isolate the plasma and separate it from the red blood cells, a tube of blood is placed in a centrifuge. The resulting plasma is a gel, which is injected around the circumference into the vaginal walls.
Expert comment:
“I always perform the PRP procedure around the entire vaginal mucosa.
To increase vaginal sensitivity and orgasm intensity, I pay special attention to working on three areas rich in nerve endings. This is the well-known zone G, and the little-known zones A and K.”
Vladislava Gladysheva, plastic surgeon, specialist in aesthetic gynecology.
For 2-3 days after therapy, it is necessary to limit physical activity and avoid baths, saunas and swimming pools.
Dryness in the intimate area during pregnancy
Dryness and burning in the intimate area in pregnant women is a consequence of hormonal changes in the body and changes in the microflora in the genital tract. The genital tract of a pregnant woman becomes more vulnerable to microbes and fungi, and therefore inflammation and irritation are possible. The discomfort is aggravated by the fact that not all traditional antibacterial and anti-inflammatory drugs are not approved for use by pregnant women, so many women are afraid of harming the child and do not seek treatment. However, such patience can harm the expectant mother herself: behind the itching, burning and other symptoms, inflammation, as well as infections of the genital tract and internal organs, can be hidden.
Dryness in the intimate area during pregnancy
Irritation can be caused by the use of panty liners with fragrances, climatic factors, and stress.
To establish the exact cause of dry skin in the intimate area during pregnancy, it is important to notify an obstetrician-gynecologist about this in order to carry out a diagnosis and draw up a treatment plan. It is important not to forget about the rules of daily intimate hygiene: regular toileting of the genitals with the GINOCOMFORT Moisturizing washing gel will relieve irritation and return the pregnant woman the opportunity to enjoy waiting for the baby, and not think about the causes of discomfort.
Dry mucous membranes in the intimate area after childbirth
The postpartum period lasts 42 days, but in various cases the recovery process may take longer. At this time, changes occur not only in the genitals: contraction of the uterus, formation of the cervix, reduction in the size of the vagina and swelling of the external genitalia. At the stage of postpartum changes in the body, dry skin and mucous membranes in intimate places and accompanying irritation are common, which is completely unnecessary for a woman during such a pleasant and troublesome period. The reasons, in addition to temporary changes in hormonal levels, can be pathogenic microorganisms and poor healing of microtraumas in the birth canal due to reduced immunity.
After childbirth, dryness in the intimate area: why does it occur?
Dryness can also be caused by disturbances in the natural microflora and the use of hormonal drugs.
The good news for a woman who has become a mother is that her hormonal levels are restored after the end of lactation, so the discomfort will not haunt her for long. To speed up the healing process of microcracks and other postpartum injuries to the genital organs, as well as restore the feeling of moisture in the genital tract, you can regularly shower with GINOCOMFORT Moisturizing washing gel, which, in addition, can be used as a lubricant during sexual intercourse. A comfortable level of moisture in the intimate areas and following the recommendations of gynecologists is the key to a quick recovery after childbirth.
Diagnosis, examination
If you experience vaginal dryness, you should immediately consult a doctor. Qualified gynecologists receive appointments at the CELT multidisciplinary clinic; their appointment schedule can be viewed on a separate page of the website. The doctor will conduct a visual examination
, will order
tests to identify potential infections and
other diseases.
It is also necessary to perform a cytological smear, or Papanicolaou test
, - a test for the presence/absence of precancerous or cancer cells in the cervix and vagina.
Dryness in the intimate area during menopause
We have already talked about atrophic vaginitis - a common disease that accompanies menopause in 80% of cases. The older a woman gets, the more often she turns to a gynecologist with complaints of decreased vaginal secretion, burning, itching and vaginal dryness[5].
The key reason for this disease is a decrease in the production of estrogens, which are responsible for maintaining optimal levels of hydration and acid-base balance in the intimate area.
Due to the dryness of the mucous membrane, the vagina loses its elasticity and becomes susceptible to injury and inflammation caused by associated infection. In addition, atrophy of the appearance of the genital organs: the skin and vaginal mucosa is a common cause of pain and a feeling of dryness during intimacy and a decrease in sexual activity in general. Depending on the progression and aggravation of delicate symptoms, obstetricians-gynecologists develop an individual treatment plan, most often including a course of hormonal medications and the selection of suitable intimate cosmetics for daily use.
Dryness in the intimate area during menopause
Treatment of dryness in the intimate area
If vaginal dryness is not caused by hormonal imbalance, obstetricians-gynecologists recommend, first of all, switching to specialized moisturizing intimate gels for delicate care of the intimate area, for example, GYNOCOMFORT with mallow. If, however, its moisture content is not enough, you can use water-, oil- or silicone-based lubricants; they compensate for its lack.
Among the more modern methods of treating dryness in the intimate area, in addition to hormone replacement therapy, there is biorevitalization, injections of hyaluronic acid and plasma therapy.
This allows you to restore the elasticity of structures, increase immunity, slowing down withering, which allows you to maintain the delicate area in a comfortable state.
Among the more serious methods of treating dryness in the intimate area, in addition to hormone replacement therapy, laser intimate plastic surgery can be distinguished. The duration of the procedure is 20-40 minutes. Due to the effect of laser beams on the vaginal walls, tone is restored and moisture is restored. After surgery, it is important to exclude sexual contact and active sports for 5-7 days. Another option is biorevitalization or hyaluronic acid injections. Hyaluronic acid molecules retain moisture in the skin, slowing down its evaporation, which helps maintain the delicate vaginal area in a comfortable condition.
Treatment of dryness in the intimate area: what is effective?
What to do when you are already undergoing treatment, but dry skin in the intimate area still bothers you? To accompany the prescribed therapy, obstetricians and gynecologists advise adjusting your diet: drinking at least 1.5 liters of water (as the main source of moisture) per day, monitoring the presence of animal fats in your diet and avoiding spicy, smoked and overly salty foods.
And of course, never self-medicate: folk remedies and quick-acting medications can relieve the symptoms of dryness, but they will not be able to eliminate the causes of your discomfort.
Proper care for dry skin in the intimate area
- Use only specialized hypoallergenic gels for dry and sensitive skin with lactic acid and natural ingredients. Proper intimate care is extremely beneficial for women of any age.
Proper intimate care is the key to good health!
- Give preference to underwear made from natural fabrics that does not restrict movement and does not cause discomfort during the day.
- Avoid douching and using rough sponges and washcloths in the bikini area. Dry skin around the vagina does not tolerate aggressive environments: daily showering with an intimate gel applied with your hands or a soft sponge is quite enough for complete care.
- If you use daily hygiene products, do not forget to change them every 3-4 hours and better avoid scented pads.
- Be examined by an obstetrician-gynecologist 1-2 times a year, and if you experience frequent irritation and other symptoms of vaginal dryness, do not delay your visit to the doctor and visit him as soon as possible.
Intimate care for women - basic rules
- During sexual intercourse, use a moisturizing lubricant. Remember that if you are protecting yourself with condoms, it is prohibited to use oil- and silicone-based lubricants.
Moisturized skin of the intimate area not only prevents discomfort, but also resists pathogenic microbes and has better elasticity and resistance to microtrauma.
Sources:
- Hormonal status and vaginal microbiocenosis. Dobrokhotova Yu. E., Zatikyan N. G. // Obstetrics, gynecology, reproduction. - 2008. - 2 (2). pp. 7-9.
- Hormonal correction of resident microflora of the vagina and cervix in women with chronic cervicitis. Dolgushin I.I., Dolgushina V.F., Chernykh S.L. // Journal. Microbiology. - 2001. - 4: pp. 100-104.
- Vaginal microbiocenosis and its disorders (etiology, pathogenesis, clinical picture, laboratory diagnostics). Clinical laboratory diagnostics. Nazarova E.K., Gimmelfarb E.I., Sozaeva L.G. // 2003. - 2: pp. 25-32.
- https://www.passion.ru/health/zhenskoe-zdorove/sukhost-vlagalisha-prichiny-i-lechenie.htm
- https://www.aif.ru/health/life/ne_day_sebe_zasohnut_kak_lechit_atroficheskiy_vaginit
- https://www.vidal.ru/encyclopedia/gynecology/atrficheskiy-vaginit
- https://abromed.ru/diseases/cancer/cervical/radiotherapy
- https://bc-clinic.ru/gynecology/suhost_vlagalisha.php
Popular questions
Good evening!
Terrible dryness in the intimate area. There was a burning sensation and painful red spots appeared. Will one of the tools presented on the site help? Hello! In your case, Ginocomfort gel with mallow extract is suitable. Its use will have a mild moisturizing, reparative, anti-inflammatory effect. The gel is introduced into the genital tract using an applicator. The duration of use is not limited.
Hello! The intimate area is dry and itchy, there is a discharge similar to thrush, but in December the symptoms were the same. I went to the doctor, had a smear test, everything was fine. While I was waiting for the result, I put on Livarol suppositories. Everything seemed to have passed, but a couple of days ago it all started again! What could it be?
Hello! I recommend conducting a more detailed examination - culture for nonspecific microflora and smear for cytology. I would also like to draw your attention to the fact that after anti-inflammatory therapy with suppositories there was no stage of restoration of microflora in the genital tract. At this stage, before receiving the test results, you can use Gynocomfort gel with tea tree oil, 1 dose 1 time per day for 7 days. This will not only relieve the manifestations of inflammation, but will also restore the balance of the pH of the vaginal environment and the number of lactoflora in the genital tract.
I am 69 years old. I am concerned about vaginal irritation and dryness. I was treated once with Triozhinal suppositories. The result was positive for 1.5 years. Now this problem has arisen again. But now these candles cause a strong burning sensation. Today I am flying to the sea, and I am afraid that I will not be able to swim, since the salt water is making the problem worse. Please advise what I can do. Thank you! Hello! During the postmenopausal period, inflammatory processes develop in the genital tract against the background of atrophic changes in the mucosa caused by hormone deficiency. Its layers become thinner, elasticity decreases, and the number of lactobacilli decreases. In this situation, a study is required: a smear for flora, oncocytology. The first step is to prescribe drugs with anti-inflammatory activity, and the second step is to moisturize, restore microflora, and, in the absence of contraindications, local hormone-containing suppositories. A feature of treatment in this age group is continuous maintenance therapy. At this stage, before receiving the results of the study, you can use Ginocomfort gel with mallow extract, which will have anti-inflammatory and moisturizing effects. The gel is applied in 1 dose 1 time per day for 10-14 days.
I am 42 years old, I have a problem, dryness in the intimate area, inside and out. How should I treat this?
Hello!
You need to conduct an examination - a smear on the flora to exclude the inflammatory process, which led to dry mucous membranes. At this stage, I recommend using Ginocomfort gel with mallow extract. This will moisturize the mucous membranes of the external genitalia and vagina. The gel is used 1 dose daily for up to 14 days. Injected using an applicator. For an accurate diagnosis, contact a specialist
Diagnostics
It is important for the gynecologist not only to determine the degree of dryness and other symptoms, but also to find out the causes of the anomaly. The doctor listens to the patient’s complaints, finds out her lifestyle, the quality of the menstrual cycle and other nuances. On the examination chair he conducts a detailed examination.
To determine the anomaly, the gynecologist prescribes colposcopy, during which he uses a colposcope: assesses the condition of the mucous membrane, its color, thickness, and integrity. Next, he moves on to specific tests that determine pH, glycogen levels and other parameters. Immediately take a smear for microflora and cytology. Colpocytological examination helps to determine the degree of maturity of the squamous epithelium.
A blood test for hormones and other laboratory tests of biological substances are required.