Features of dry skin in children
Normally, the body is clean, smooth and soft to the touch. When dry, the skin becomes rough, wrinkled, loses elasticity, peeling appears, and the risk of infection increases, as microcracks easily occur.
Dry skin in a child can develop under the influence of external factors, and can also be a symptom of various diseases. If the skin can be protected or restored from certain adverse effects by proper care, then in the presence of diseases it is necessary to consult a doctor.
Causes of dry skin in newborns
Among the medical problems of dry skin in children, perhaps the first place is occupied by atopic dermatitis. The disease is based on a genetic defect in barrier function, resulting in increased loss of moisture. The disease begins at an early age and is characterized by dryness, itching, and during periods of exacerbation - the appearance of inflammatory foci. If an exacerbation must be eliminated with medications, then in the period between exacerbations, the care recommended by the doctor must be carried out daily. Typically this is the use of emollients.
LIPIKAR BAUME AP+M
Lipid-restoring balm for face and body
Relieves dry skin in children. Instantly soothes atopic skin, reduces itching and irritation, and increases the intervals between outbreaks of excessive dryness.
581 rub. more details
Ichthyosis is another cause of dry skin in newborns. This is a congenital disease, which is accompanied by a violation of keratinization of the upper layer of the epidermis. As a result, fish-like scales can form on the body, hence the name of the disease. This is not a very common disease, it can occur in different ways, from mild manifestations to severe conditions requiring constant therapy.
Diseases of the endocrine system (underfunction of the thyroid gland, diabetes mellitus), helminthic infestation, some diseases of the gastrointestinal tract, deficiency of certain vitamins A and PP are also reasons why a child has dry skin. Regular monitoring of the baby, periodic examinations by a pediatrician, and timely treatment, if required, will allow these causes to be suspected and eliminated in a timely manner.
If a child has dry skin on his body, there are other reasons. In the first month of a baby’s life, physiological dryness of the skin may develop. In utero, the child is in an aquatic environment, and after birth it moves into an air environment, and it takes time for the baby to adapt. The main cause of this condition is the insufficient functioning of the sweat glands, which begin to activate after birth. Physiological dry skin can manifest itself in the form of peeling all over the newborn’s body. Gradually, over the course of a month, this physiological condition disappears. After water procedures, it is enough to moisturize the baby’s skin with a light cream or special milk. For example:
LIPIKAR LAIT
Unscented milk for dry to very dry skin
Nourishes and restores the lipid barrier of the skin. Suitable for small children and babies.
992 rub. more details
But if the skin of a one-year-old baby is excessively dry, this is a reason to consult a doctor to get recommendations for care to avoid the development of complications.
Any inflammatory process, be it a cold or a more severe condition, accompanied by a rise in temperature contributes to the loss of moisture from the body. Dyspeptic symptoms, insufficient drinking, frequent diarrhea or poisoning of the child are accompanied by loss of fluid, and, as a result, dehydration develops. One of the manifestations of this condition will be very dry skin in a child, which can be corrected by moisturizing the face and body with baby light cream or milk.
Only after the age of 6 years does a child’s skin become like that of an adult. And before this age, it is characterized by high permeability and therefore loses natural moisture much easier and faster. It is more vulnerable to injury, and through damage it can become infected, especially in infancy. Therefore, it is important to carefully monitor and care for her every day.
If your baby develops areas of irritation or dryness as a reaction to food, contact with a substance, or after being in the sun, we recommend that you consult a doctor. The causes and treatment are always different, and the wrong medications and creams can lead to serious skin lesions.
Skin of newborns: differential diagnosis of pathological conditions, features of care
I.A. GORLANOV
, Doctor of Medical Sciences, Professor,
L.M.
LEINA , Ph.D.,
I.R.
MILYAVSKAYA , Candidate of Medical Sciences,
St. Petersburg State Pediatric Medical University Issues of caring for the skin of a child in the first years of life remain relevant to this day.
Due to the anatomical and physiological characteristics of children, the protective function of the skin, protecting against adverse external influences, is significantly reduced in them. The influence of various damaging factors, improper use of care products - all this can lead to disruption of the normal condition of the skin. The most common skin lesions in children of the first year of life include diaper (contact) dermatitis, the prevalence of which can be up to 50%. The importance of proper baby skin care as the main element in the prevention of dermatitis is undoubted. Features of the skin of infants and young children
The skin of a newborn baby has its own characteristics, which is associated with its transition at birth from an aquatic intrauterine environment. At birth, the skin is covered with vernix caseosa, which is 80% water, as well as lipids and proteins [1]. “Virginic lubricant” lipids are formed in the epidermis and sebaceous glands. As studies by Marchini G. et al. have shown, the original lubricant contains antibacterial peptides that play a protective role both before birth and in the first days of life [2].
The skin of newborns and infants is soft, velvety, pink. It is much thinner than the skin of an adult. In newborns, the structure of the epidermis at this age differs in a number of features. Their epidermis is much thinner. The basal cells are small in size, and the number of desmosomes at the junctions of cells is also reduced. The stratum spinosum has 2–5 rows of cells. The granular layer is poorly developed and consists of 1–2 rows of cells. Unlike the skin of adults, in infants the shiny layer is practically absent even on the palms and soles. The connection between the cells of the stratum corneum is weak, the horny plates are easily rejected (physiological parakeratosis) [1, 3].
By the time of birth, two layers are distinguished in the dermis, although not very clearly: the upper one is papillary and the lower one is reticular. The border between the epidermis and dermis is smoothed. In newborns and infants, the dermis is thinner than in older children and differs in structure. With the exception of the palms and soles, the papillary layer is not yet fully formed. The skin of newborns is highly hydrophilic. The subcutaneous fatty tissue of newborns and infants also has a number of features. At birth, the mass of subcutaneous fat is 4-5 times greater than in adults. In newborns, brown adipose tissue predominates, which is replaced with white with age. In terms of its chemical composition, subcutaneous fatty tissue also differs from that of adults. It is dominated by saturated fatty acids.
Skin appendages are imperfect at birth. There are 12 times more eccrine sweat glands in newborns than in adults. Their secretory section is represented by 6-12 loops of epithelial tubes, and the excretory duct is located in the dermis and epidermis. Unlike adults, the excretory ducts of the sweat glands in the epidermis of infants are usually straight and not corkscrew-shaped. The result of their immaturity is frequent blockage of the eccrine sweat glands with keratin plugs. With age, the sweat glands become more formed, larger, and the intensity of sweating after 2-3 months. after birth it returns to normal [1].
Newborns are characterized by hyperplasia of the sebaceous glands. Their number per 1 cm of facial skin in newborns is 4–8 times greater than in adults. After 40 weeks During pregnancy, the skin of a mature newborn is almost fully developed anatomically. Its weight is 10−13% of a newborn's body weight, compared to 3% in an adult. Anatomical maturity only partially correlates with functional maturity, and this discrepancy concerns both barrier function and thermoregulation. In a newborn child, the connection between the epidermis and the dermis is weak, while the dermal-epidermal junction plays an important role in the skin’s ability to withstand mechanical stress, therefore, in the neonatal period, injuries associated with detachment of the epidermis from the dermis can occur [2–4].
The characteristics of the skin of newborns and infants contribute to the easy occurrence of skin lesions with a pronounced exudative reaction and generalization of inflammatory processes. Dermatoses that occur at an early age differ significantly from diseases in adults and require specific care and treatment.
Violation of the skin barrier function is manifested by an increase in transepidermal water loss and the risk of percutaneous intoxication from external agents. For example, transdermal absorption occurs directly through the stratum corneum, hair follicles and sweat glands. And in premature babies, the barrier function of the skin is formed by the 4th week. life. The risk of percutaneous absorption in newborns, according to Eichenfield LF, Frieden IJ, Esterly NB, is presented in table [5].
Physiological and pathological conditions unique to the skin of newborns and infants are explained by its structural and functional properties. Features of proliferation and differentiation of epidermal and dermal cells, lipid composition and structure of connective tissue fibers determine the elasticity and velvety of the skin. The abundance of blood vessels and the constantly dilating capillary network give the skin of a newborn a peculiar bright pink color. A large number of functionally labile lymphatic tubules forming “lymphatic lakes” form pastosity and easily occurring edema.
Due to anatomical and physiological characteristics, various manifestations may appear on the skin during the neonatal period, including physiological or borderline conditions that do not require active intervention, as well as severe diseases [6–8].
Physiological conditions include physiological desquamation, erythema of the newborn, telangiectasia, blue (Mongolian) spots, sebaceous ichthyosis (Ichthyosis sebacea), milia.
Borderline changes in the skin of newborns can be considered miliaria and toxic erythema, which may require medical intervention.
Diseases requiring treatment include vesiculopustulosis, pyoderma of various etiologies, limited skin defects (Aplazia cutis), subcutaneous adiponecrosis, diaper dermatitis of varying severity.
Physiological peeling. Peeling of the skin (desquamation of the skin of newborns) is observed 24-36 hours after birth, more often in post-term infants and lasts up to 3 weeks. If desquamation is visible immediately after birth, congenital ichthyosis must be excluded. Bepanten cream can be used as a treatment for physiological peeling.
Erythema of newborns (physiological catarrh of the skin) is characterized by hyperemia of the skin due to dilation of capillaries in response to exposure to an ambient temperature lower than intrauterine. This erythema usually persists for 2-3 days and then decreases until it disappears. Redness of the skin is replaced by more or less pronounced pityriasis-like or lamellar peeling.
Telangiectasias are densely located dilated capillaries of the skin in the form of spots, most often located in the area of intrauterine presentation of the head - in the back of the head or on the forehead, sometimes in the area of the eyebrows and eyelids (nevus of Unna). The spots disappear when pressed and intensify when the child cries. It is believed that this is not a capillary nevus, but a transient vasodilation. Such telangiectasias disappear on their own after 1-1.5 years. No treatment required. According to Kanada KN et al., the incidence of telangiectasias is observed in 83% of newborns [9].
Blue, or Mongolian, spots are found only in representatives of the Mongoloid race and children with dark skin. Usually on the skin of the lumbosacral region, less often on the shoulder blades or buttocks, a bluish-purple spot of irregular shape of various sizes is found. When pressed, the stain does not disappear, the skin in the lesion is not changed. Usually this is a single formation, but there are also multiple ones. Histological examination reveals spindle-shaped melanocytes in the dermis (normally they are not found there). This appears to be the result of incomplete migration of melanocytes into the epidermis from the neural crest. Mongolian spots usually disappear spontaneously by 5-6 years.
Sebaceous ichthyosis (Ichthyosis sebacea) occurs due to increased secretion of quickly drying sebum by the sebaceous glands. The skin of a newborn baby becomes dry, rough to the touch, and acquires a brownish tint. Superficial cracks appear on the surface of the sebaceous crust. After a week, the process ends with abundant pityriasis or lamellar peeling. If a child has embryonic hair (lanugo) preserved on his skin, then when it is glued together with sebaceous secretion, the so-called hair is formed. seta. After the crust is rejected on the 6th–8th day, the skin takes on a normal appearance. The child’s condition with sebaceous ichthyosis is not affected and no treatment is required. Skin care is carried out by holding warm baths followed by lubricating it with lanolin cream or dexpanthenol. Sebaceous ichthyosis is differentiated from congenital.
Milia are small epidermal cysts that develop from the sebaceous glands of the hair vellus. Occurs in more than 50% of mature newborns. Milia appear from the moment of birth and are whitish-yellow papules the size of a pinhead or millet grain (milium). They are usually localized in the forehead, on the nose and cheeks, and in premature babies even on the trunk and limbs. These elements are epidermal retention cysts containing, in addition to thick fat, horny scales. Within 3−4 weeks. milia disappear. No treatment is required [3].
Miliaria is a reaction of the child’s body to overheating, associated with blockage of the sweat glands due to their functional immaturity. Miliaria occurs in approximately 15% of newborns. It is caused by a temporary blockage of the excretory ducts of the eccrine sweat glands. The appearance of prickly heat is promoted by high temperature and humidity of the rooms in which newborns are located. There are crystalline and miliaria rubra. With crystalline miliaria, blockage of the sweat gland ducts occurs at the level of the stratum corneum. Small blisters without an inflammatory component appear on the skin, filled with transparent contents. Bubbles sizes up to 1 mm. With prickly heat, the level of blockage of the sweat gland ducts is deeper. The rashes are represented by small erythematous papules and papulovesicles. The localization of rashes is any, but more often they appear on areas of the skin covered by clothing (torso, axillary and groin areas). With severe hyperhidrosis, prickly heat appears on the face, neck and scalp. Being inherently a physiological condition, prickly heat is often complicated by the addition of a secondary pyococcal infection, resulting in the development of vesiculopustulosis or even abscesses of the sweat glands.
When treating prickly heat, baths with potassium permanganate and drying agents in the form of powders are usually used. Prevention consists of ensuring temperature control, daily bathing, and air baths [1, 3, 6].
Newborn acne (Acne neonatorum) occurs in newborns at 2–3 weeks. life, are more common in boys than in girls. The cause of this condition is not completely clear; their appearance is usually associated with hormonal stimulation of the sebaceous glands by maternal androgens. Acne appears more often and lasts longer in breastfed children. The rashes are usually located on the face in the cheek area, on the forehead and on the nose in the form of small papules and pustules, surrounded by a halo of hyperemia. Less commonly, similar elements appear on the chest and shoulders. Breastfed children get sick. The process on the skin resembles that of teenage acne vulgaris and is associated with postpartum hormonal changes in the mother’s body. Acneiform rashes in newborns can be associated with the saprophyte Malassezia furfur and Malassezia sympodialis and are referred to as neonatal cephalic pustulosis [6, 7, 9, 10].
For single pustular elements, treatment consists of treating the skin with disinfectant 30−40% alcohol solutions of 1−2% salicylic acid, powder containing neomycin and bacitramine, and salicylic-zinc paste. It is possible to use external antifungal agents. The mother is prescribed a dairy-vegetable diet and increased fluid volume. In case of a common form of acne with severe pustulization, antibacterial therapy is prescribed taking into account the sensitivity of the pathogenic flora and specific bacteriophages.
Toxic erythema of newborns is observed in almost half of newborns on the 2nd–5th day of life. It is rare in premature babies. This condition is considered borderline between normal and pathological. Modern research confirms the hypothesis of an excessive reaction of the immune system to the first colonization of the skin by non-pathogenic microorganisms [2, 3]. In addition, it has been established that the mother’s consumption of large amounts of foods that are obligate allergens (chocolate, condensed milk, fish, citrus fruits, etc.) after childbirth can play a role in the formation of toxic erythema. Most often, this condition is considered as the first manifestations of an allergy (as well as dry skin, flushed cheeks, etc.).
In the clinical picture of the disease, limited and generalized forms are distinguished. With limited toxic erythema, single small (miliary and lenticular) spotted and urticarial elements of a bright pink color appear on the skin of the extensor surfaces of the limbs, trunk, and buttocks; a vesicle can be seen in the center of only a few. The child's condition is not affected. In the generalized form, the rash is abundant, polymorphic with a predominance of papulovesicles, urticaria and even pustules, prone to rapid spread and fusion (Fig. 1). The general condition of the child, as a rule, is not disturbed. Eosinophilia is present in the blood in 20% of cases. A generalized form is often treated with antihistamines. Treatment of toxic erythema involves prescribing a hypoallergenic diet to the mother. Externally, vesicular and pustular elements are treated with a 1% solution of brilliant green. The rash usually lasts 2-4 days, with a generalized form up to 7-10.
Limited congenital defects of the skin and subcutaneous tissue (Aplazia cutis) can occur when the amniotic membranes of the fetus are disrupted, at the site of intrauterine healing of hemangiomas, or during an attempted abortion. It is possible that such a disease is preceded by viral or bacterial infections at the beginning of pregnancy or occupational hazards of the mother (radiation, chemical agents, etc.). The frequency of skin aplasia is 1: 5 thousand. Changes on the skin are visible immediately at the birth of the child. More often, defects in the skin, subcutaneous tissue, and sometimes deeper defects are visible on the scalp, as well as on the torso or limbs. The lesions take the form of granulating ulcers or scars of a round or oval shape ranging in size from a few millimeters to 5-6 cm in diameter. Sometimes aplasia cutis is combined with such congenital anomalies as cleft upper lip and hard palate, malformations of the limbs, etc. The differential diagnosis of Aplazia cutis is carried out with a nevus of the sebaceous glands, which can also be seen from birth in the form of a lesion with no yellowish hair protruding above the surface skin. If aplasia is localized in the midline of the skull, it is advisable to conduct an ultrasound examination to exclude encephalocele.
The disease should be differentiated from possible injuries during childbirth, congenital syphilis, and congenital epidermolysis bullosa. Treatment depends on the child's condition. In case of numerous injuries, antibacterial therapy and agents that improve microcirculation and epithelization are prescribed. Ulcerative defects are treated with disinfectant solutions (hydrogen peroxide, furatsilin, chlorhexidine), ointments containing antibiotics, solcoseryl, actovegin. There is no treatment for scars [1, 3].
Subcutaneous adiponecrosis appears in the 1st–2nd week. life and is an essential disease of young adipose tissue with a disorder of lipid metabolism due to the peculiar ratio of fatty acids (the predominance of saturated acids over polyunsaturated ones). Histologically, extensive necrosis of subcutaneous fatty tissue with the presence of reactive inflammation, giant and epithelioid cells is determined. The pathological process occurs at the sites of injury during obstetric manipulations (application of forceps, turning the fetus, resuscitation measures). Large, full-term newborns are usually affected.
Clinically, sharply demarcated nodes or infiltrates appear in the area of the back, shoulders, and buttocks, up to the size of the child’s palm. The skin over the infiltrates is initially cyanotic or violet, then becomes pale. The nodes are usually painless and the general condition of the child is practically not affected. Treatment consists of prescribing thermal procedures (dry warming bandages, Sollux), vasodilators and antioxidant drugs [1].
Diaper dermatitis
One of the most common skin changes is diaper dermatitis (ND), the incidence of which ranges from 35 to 50% [24]. At the same time, premature babies are high-risk patients. PD is more often observed in girls. A greater predisposition to PD was noted in children with increased sensitivity to allergens, which is explained by the frequent development of exudative phenomena and dyspepsia. The disease belongs to the group of region-specific dermatoses, in which an acute inflammatory reaction of the skin occurs in the area covered by diapers. In recent years, thanks to the widespread use of industrial diapers with good hygroscopic properties, the number of diaper dermatitis has decreased. The disease is multifactorial in nature and is initiated by a combination of a number of factors: physical, chemical and biological (interaction of the skin with urine and feces). The main condition for the occurrence of diaper dermatitis is skin occlusion due to the use of diapers. The surface in contact with diapers is excessively moistened, the stratum corneum is loosened, as a result of which the barrier functions of the epidermis are reduced and the skin becomes more sensitive and vulnerable. Such changes contribute to the colonization of yeast-like fungi Candida albicans and gram-positive bacteria, in particular Staphylococcus aureus and streptococci, on the surface of the skin. Enzymes secreted by microorganisms break down uric acid, promote the synthesis of ammonia and create an alkaline skin reaction, which in turn activates the enzymatic activity of feces [11–13].
Most often, contact dermatitis develops in those areas that come into direct contact with the diaper. The buttocks and genitals are most affected. First, spots appear with erythema of varying intensity, then the skin in the affected areas becomes swollen, sometimes peels, and later papular rashes may appear. Children who spend a long time in diapers with poor absorption at night may develop erosions and sometimes even ulcers on the surface of the skin. Diaper dermatitis, a type of simple contact dermatitis, is more typical for children in the first month of life, which is explained by the anatomical and physiological characteristics of the skin (Fig. 2).
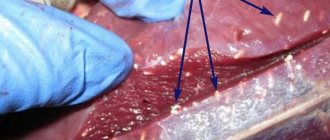
The second most common after simple diaper dermatitis is candidiasis diaper dermatitis. It is represented by different-sized bright, clearly defined erythematous foci of irregular shape, spotted and papular in nature. Characterized by a fairly rapid growth of lesions along the periphery, a tendency to the appearance of fresh rashes in folds and on contacting surfaces. Along the periphery of the lesions one can often see “screenings” of miliary papules and small flaccid superficial pustules, after the opening of which erosions with fragments of epidermis of a regular round shape remain (Fig. 3). There is a tendency to increase the area of eroded surfaces, which have a bizarre shape with clearly defined boundaries of scalloped outlines. The likelihood of secondary candidal infection is very high with any form of diaper dermatitis that lasts more than three days. In infants, candidiasis in the anogenital area is often combined with thrush in the oral cavity, where there is a white cheesy coating and cracks in the corners of the mouth. These patients may also have intestinal candidiasis. The diagnosis is based on clinical data and microscopy - detection of hyphae and pseudomycelium [14, 15].
PD of bacterial etiology is most often caused by b-hemolytic streptococci, and is called papulo-erosive streptodermia. Predisposing factors to the occurrence of this form of dermatitis are the formation of ammonia in wet diapers, excretion of antibiotics in the urine, and washing clothes with synthetic scented detergents. On the skin of the buttocks, the back of the thighs, and in boys, on the scrotum, on an erythematous, somewhat edematous background, miliary and lenticular papules of a pinkish-bluish color appear slightly protruding above the skin, on the surface of which erosions quickly appear.
Prevention and treatment of PD
The key to treating PD is good skin care to prevent irritation and damage to the epidermis. This is achieved by cleansing the skin, protecting it from adverse effects, in particular contact with secretions [25]. Skin care principles
1. It is necessary to change diapers in a timely manner. In particular, the shift should be carried out early in the morning (immediately after the child wakes up), immediately before the baby goes to bed, after each feeding, if the child shows signs of anxiety; in any case, at least every 3-4 hours. 2. Clean and dry the skin regularly and thoroughly, especially in the anus and genital area. Due to the low threshold of irritability, it is advisable to use detergents sparingly. Soap can irritate the skin due to alkaline components, and synthetic detergents (bath bubbles, shampoos) due to the degreasing effect they produce. Therefore, it is necessary to bathe a baby using detergents no more than 2-3 times a week, while washing should be done regularly, and after bowel movements it is mandatory. 3. Air baths should be performed every time you change diapers. 4. To prevent skin contact with secretions (urine and feces), it is advisable to use modern disposable diapers, the inner cellulose layer of which contains a gel-forming material with high moisture-absorbing ability. 5. Applying barrier cream at every diaper change. When erosions occur, treatment with a 1% aqueous solution of aniline dyes (brilliant green or eosin) is necessary.
During PD, the use of creams and ointments is recommended to treat affected areas of the skin. In dermatological practice, for the purpose of healing, improving trophism and tissue regeneration, topical products containing vitamin B5 (pantothenic acid), which is not without reason called the antidermatitis factor, are used. In the body, provitamin pantothenic acid (synonymous with vitamin B5) is an integral part of coenzyme A, which is involved in many enzymatic reactions of aerobic cell metabolism. Firstly, coenzyme A, acting as an intermediate carrier of acyl groups, promotes the formation of acetyl-CoA with subsequent initiation effective oxidative breakdown of carbohydrates and fatty acids, resulting in the formation of ATP. Thus, vitamin B5 is one of the essential components that allows the complex system of cellular bioenergetics and metabolism to function normally. Pantothenic acid stimulates the production of glucocorticoids, which partly explains the effectiveness of vitamin B5 in the treatment of allergies. The most important property of this vitamin is its participation in tissue regeneration and healing of damaged epithelium.
The drugs of choice, which have proven their effectiveness and safety for the prevention and treatment of PD, are the Bepanten line. The active substance of Bepanten is dexpanthenol (synthetic provitamin pantothenic acid - B5). which helps prevent the development or speedy healing of already formed microcracks. The provitamin dexpanthenol, which is part of the drug, is quickly converted into pantothenic acid in skin cells, exerting its therapeutic effect, enhancing the metabolic activity of dermatocytes and stimulating regeneration processes
The drug is available in the form of a 5% ointment, as well as in the form of a 5% cream and a cream with antiseptic properties containing chlorhexidine - Bepanten plus.
In pediatric practice, the form of Bepanten is actively used in the form of an ointment, which, in addition to the active ingredient - dexpanthenol, includes lanolin, almond oil, and liquid paraffin. The main inactive substance of Bepanten, lanolin, is close in lipid composition to the secretions of the sebaceous glands. Being semi-permeable, lanolin provides a pronounced protective effect without interfering with gas exchange. Lanolin also penetrates the stratum corneum of the skin, providing its hydration, and reduces friction, one of the main causes of diaper dermatitis.
Since Bepanten ointment does not stain the skin, does not contain dyes or preservatives, is practically odorless, and the fatty components of the ointment are well absorbed by the skin, it is deservedly popular among both pediatricians and parents. When using Bepanten ointment or cream, it is also necessary to take into account its lack of antibacterial and antiviral effects.
Bepanten ointment should be applied daily in a thin layer to the affected areas of the baby's skin during swaddling until the symptoms of diaper dermatitis disappear. For preventive care, the ointment is applied to the skin of the buttocks and groin area with each diaper change. Bepanten ointment is especially effective for the prevention of PD, prickly heat, and milk scabs on the skin of infants.
It is advisable to use Bepanten cream as a care product for dry, irritable skin, as well as as a preventative for healthy skin.
When identifying skin abrasions, products that also have disinfectant properties are used as a topical agent. Thus, Bepanten Plus cream, which contains 0.5% chlorhexidine, provides, in addition to the regenerative effects of dexpanthenol, antiseptic and disinfectant. An important advantage of the cream for use in pediatric practice is its ability to not cause pain when applied to a wound surface.
The use of Bepanten Plus cream is effective for the treatment of diaper rash accompanied by weeping.
The high clinical effectiveness of Bepanten ointments and creams has been confirmed by a number of clinical studies. [2−3, 19−20]. According to foreign and domestic researchers, when assessing the effectiveness of using Bepanten ointment in the treatment of infected skin lesions in newborns, the following data were obtained in 58% of children - complete disappearance of dermatitis, in 48% - a significant decrease in skin symptoms [21−23].
If candidiasis of the skin is suspected, pastes, creams and ointments from the group of imidazoles (clotrimazole, ketoconazole) are used externally. External therapy for diaper dermatitis of bacterial etiology includes the use of fusidic acid in the form of a cream or paste. Systemic therapy is usually not required [16]. Conclusion
Compliance with hygiene and skin care rules prevents the development of PD and secondary (associated) skin infections in young children. Treatment and observation of children with uncomplicated PD is carried out by pediatric neonatologists or general pediatricians. In the case of a complicated or prolonged course of PD, differential diagnosis requires consultation with a pediatric dermatologist.
Bibliography
1. Zverkova F.A. Skin diseases of young children. St. Petersburg: Sotis, 1994:236. 2. Ivanova N.A., Kostrakina L.N. Experience with the use of bepanten and bepanten plus in the treatment of atopic dermatitis in children. Consilium medicum. Pediatrics 2005;1:39-41. 3. Yatsyk G.V., Akoev Yu.S. Clinical effectiveness of various newborn skin care products based on D-panthenol. Cons. Med. Pediatrics 2004;6(2):41-3. 4. Marchini G, Lindow S, Brismar H, Stabi B, et al. The newborn infant is protected by an innate antimicrobial barrier: peptide antibiotics are present in the skin and vernix caseosa. Br. J of dermat., 2002;147:1127-1134. 5. Peter G. Heger Pediatric Dermatology M., 2013.633. 6. Schmid-Wendtner MH, Korting HC. The pH of the skin surface and its impact on the barrier function. Skin Pharmacol. Physiol., 2006;19(6):296-302. 7. Eichenfield LF, Frieden IJ, Esterly NB. Textbook of neonatal dermatology. 2001. 8. Darmstadt GL, Dinlos JG. Neonatal Skin Care. Pediatric Dermatology 2000;47(4):757-8. 9. Color Textbook of Pediatric Dermatology. William L. Weston, Alfred T. Lane, Joseph G. Morelli. Mosby, fourth edition, 2007:466. 10. Hurwitz. Clinical pediatric dermatology. Fourth edition, Elsevier Saunders, 2011:624. 11. Canada RN, Merin MR, Munden A, Friedlander SF A prospective study of cutaneus findings in newborns in the United States: correlation with race, ethnicity, and gestational status using updated classification and nomenclature. The J. of Pediatr., 2012;161(2):240-5. 12. Zuniga R, Nguyen T Skin conditions: common skin rashes in infants. FP Essent 2013;407:31-41. 13. Marty O. Visscher Recent Advances in Diaper Dermatitis. Etiology and Treatment Pediatr Health., 2009;3(1):81-98. 14. Visscher MO, Chatterjee R, Munson KA, Pickens WL, Hoath SB: Changes in diapered and nondiapered infant skin over the first month of life. Pediatr. Dermatol., 2000;17(1):45-51. 15. Wolf R, Wolf D, Tuzun B, Tuzun Y. Diaper dermatitis. Clin. Dermatol., 2000;18(6):657-660. 16. Scheinfeld N. Diaper dermatitis: a review and brief survey of eruptions of the diaper area. Am. J. of clinical. Dermatol., 2005;6(5):273-81. 17. Marty O. Visscher. Recent Advances in Diaper Dermatitis: Etiology and Treatment. Pediatr. Health. 2009;3(1):81-98. 18. Concannon P, Gisoldi E, Phillips S, Grossman R. Diaper dermatitis: a therapeutic dilemma. Results of a doubleblind placebo controlled trial of miconazole nitrate 0.25%. Pediatric. Dermatology. 2001;18(2):149-55. 19. Ebner F, Heller A, Rippke F, Tausch I. Topical use of dexpanthenol in skin disorders. Am. J. Clin. Dermatol., 2002;3(6):427-433. 20. Tahiliani AG, Beinlich CJ. Pantothenic acid in health and disease. Vitam. Horm., 1991;46:165-228. 21. Gillman T. The dermis. An Introduction to the Biology of the Skin, Philadelphia. 1970. 22. Pulet G. Effect of Bepanten. Realitis Pediatricas. 52, 2000. 23. Revyakina V.A. Modern technologies for skin care in children with atopic dermatitis. Attending Physician 2004;3. 24. Jordan WE, Lawson K, Berg R, Fromxman J. Diaper dermatitis: frequency and severity among a general infant population. Pediatr. Dermatolog., 1986;3:198-207. 25. Liou LW, Janniger CK. Skin care of the normal newborn. Cutis., 1997;59(4):171-174.
External factors that cause dry skin in a child
Dry skin in a one-year-old child may not only be due to medical problems. Improper or excessive care, too frequent bathing, poor nutrition, and climate affect the condition of the dermis. Using very hot water or very hard water when washing will dry out your skin. We recommend paying attention to special mild detergents, monitoring the water temperature when bathing (not higher than 37°C), choosing soft towels and using a moisturizing or nourishing cream after a bath.
Another external cause is dry air and overheating. Thermoregulation processes in babies are poorly developed and continue to develop after birth, so the baby cannot quickly and adequately respond to overheated air or excessive wrapping. This is also due to the fact that the sweat glands after birth do not function sufficiently and have underdeveloped ducts. First of all, the formation of sweat glands ends on the forehead and head, then on the chest and back. The formation of the sweating function occurs over 7 years.
It is recommended to use a humidifier at home, especially in winter when the heating is running (the recommended humidity in the room should be 40-70%) and preference for light clothing that does not allow overheating (sometimes the easiest way to determine may be to feel your back and neck under clothing - they should not being hot or wet, as well as red cheeks in a baby with normal, non-rough skin are signals of overheating).
Another feature is the incomplete formation of melanin in children, a pigment that protects the skin from UVA rays. Therefore, until the age of 6 months, the baby should avoid direct sunlight, and at an older age, do not forget about sun protection. Up to a year, a child can be in the open sun for no more than five minutes a day, and only with a special children's sunscreen. Ultraviolet light dries out the skin and also increases the risk of cancer.
Frost and cold air are another challenge. Under the influence of bad weather in autumn and winter, the development of redness, dryness, peeling and irritation of the skin is possible. What to do to avoid dryness? Use cold cream (or emollient) about 20-30 minutes before leaving the house to prevent chapping of your baby's face and hands.
If your child’s dry skin lasts for a long time, you should first contact your pediatrician to rule out various diseases. If you have a skin rash, you may need to consult a dermatologist. Following your doctor’s recommendations, as well as proper daily care, will help you cope with dryness.
Advantages of the Morozko® children's winter series
All products included in the Morozko® line are hypoallergenic and safe. They were developed by domestic specialists taking into account the characteristics of harsh Russian weather conditions and are designed specifically to protect delicate children's skin from them. These products contain allantoin, chamomile extract, vitamins A, E and F. Natural ingredients carefully care for the baby’s skin, restore its natural strength, softness and elasticity, and restore the protective barrier.
For the care of thin facial skin, which is susceptible to frostbite and chapping in winter, the Rosy Cheeks® cream is intended. It creates a protective film on the surface of the skin that prevents the evaporation of water molecules, which means it will protect the face from the prickly wind and cold. A special children's hygienic lipstick Morozko® based on natural oils and wax has been developed for a child's lips, which effectively nourishes the lips and protects them from the cold wind.
Hand cream Mittens® will protect the skin from the effects of low temperatures, melted snow and ice water, and will also gently soften and soothe irritated and dry skin on a child’s hands, heal pimples and cracks and prevent possible drying out.
Morozko® universal cream is ideal for skin with severe dryness. It is made on the basis of reverse emulsion, has a high fat content and does not freeze even in severe frosts below 20⁰C. In addition, the cream perfectly eliminates dryness and irritation of the skin caused by water and detergents.
1Lukushkina E.F., Baskakova E.Yu. Skin is a barometer of health. Preventive and therapeutic role of emollients // RMZh. 2021. No. 18. pp. 1246-1252.
Rules for caring for dry baby skin
Caring for a child’s skin during the day consists of several stages: washing the face, washing hands, washing intimate areas after each bowel movement, and bathing.
It is permissible to bathe a baby every day, as it not only cleanses the skin, but also calms the child, strengthens him, awakens his appetite, improves tactile and emotional skills, and improves psychological contact with parents. One of the mistakes parents make is bathing their child for a long time in a bath with potassium permanganate. Such bathing dries out the skin and is not advisable to use. Contraindications for water procedures are high body temperature and the presence of purulent-inflammatory diseases or open wounds on the body.
Bathing water should be soft and, if necessary, filtered. The water temperature should also not be high; it is optimal if it is 34-37° C. In order not to damage the protective hydrolipidic layer of the baby’s skin, it is not recommended to use bathing products every day. Pay attention to special products for babies that have delicate formulas and have been tested by pediatricians and dermatologists.
LIPIKAR GEL LAVANT
Soothing shower gel with protective properties
Soothes the skin, thanks to the action of Niacinamide and the lipid-restoring properties of Shea Butter, helps restore the skin's protective barrier. Suitable for cleansing the skin of the face and body, does not irritate the eyes.
719 rub. more details
This gel can also be used to cleanse babies' heads and for daily intimate hygiene when changing diapers. Washing should be as gentle as possible; it is not recommended to use washcloths made of rough materials.
After bathing, dry the body and apply a moisturizer. The towel should not be hard, you should not rub the baby’s skin too much, it is better to gently blot away excess moisture. You can use a terry bathrobe. During the first 3-5 minutes after bathing, while the skin is still damp, it is advisable to apply a moisturizer. You can use Lipikar Lait milk . It has a rich formula based on cold cream - a classic combination of protective lipids, enriched with Shea butter (10%) to restore the lipid barrier. Suitable for very dry skin of children and adults. And niacinamide provides long-lasting comfort to even the driest, most delicate and sensitive skin.
Create a favorable microclimate in the room where the child is. The air should not be dry, the temperature should not be higher than 18-22°C. Monitor the humidity, ideally if it fluctuates in the range of 40-70%. To maintain humidity, you can purchase a humidifier. During the heating season, it is necessary to shield the batteries; you can cover them with a wet towel to evaporate moisture.
Choose clothes made of cotton fabric, it breathes well and absorbs excess sweat well. Give air baths while changing diapers. When walking, do not wrap your baby tightly to avoid sweating.
During the summer, avoid going out in the sun during the hottest hours, from 11 a.m. to 4 p.m., or when the ultraviolet index is above 4 (just check this indicator in the Weather app on your smartphone or almost any website to determine the weather forecast). Be sure to wear a Panama hat or a hat for your child to protect from the sun; on the beach, it is better for your child to wear a closed swimsuit or T-shirt. Do not neglect sunscreens; choose them according to the child’s age. Be sure to reapply the cream every few hours according to your child's skin type and sun exposure that day. When you return home, wash off any remaining sunscreen and apply moisturizing milk to your skin. For mild sunburn or redness of the skin, you can use:
CICAPLAST BAUME B5
Multi-regenerating and healing product for baby skin
Due to its rich, nourishing texture, it protects the skin and creates a barrier that prevents bacteria from reaching the surface. Panthenol in the composition promotes the healing of irritated skin.
654 rub. more details
What to do to prevent your child's skin from drying out
Preventive measures against dry skin:
- regular care;
- drinking regularly;
- balanced diet with sufficient vitamins;
- use of special soft care products tested by pediatricians and dermatologists.
Baby bathing and care products are marked on the packaging: “suitable for the use/care of the skin of infants and children”, “suitable for children” or the like. Plus, as a rule, the production of children's products is subject to higher requirements for the safety of formulas and stricter selection of components included in the formula.
How to make an appointment with a dermatologist
You can make an appointment with a dermatologist at the pediatric department of JSC “Medicine” (academician Roitberg’s clinic) using the form on the main page of the site. It is necessary to enter feedback information in order to agree on a convenient time and date for a visit with the child.
If it is necessary to make an accurate diagnosis, the doctor can additionally refer you for examination to other specialized specialists: an allergist, an immunologist, etc. Contact reception number for questions and appointments with doctors. The clinic has a convenient location in the Central Administrative District near the Mayakovskaya metro station at the address: Moscow, 2nd Tverskoy-Yamskaya lane, building 10. Other stations are within walking distance: Belorusskaya, Chekhovskaya, Novoslobodskaya, Tverskaya " Qualified doctors with extensive experience treat young patients with care and attention.
Take care of the health of your children together with JSC “Medicine” (clinic of academician Roitberg).