Risks of infection
- direct contact with the skin of an infected person;
- playing or caring for animals;
- using clothes and shoes of infected people, or personal hygiene items, such as combs, brushes or towels;
- exchanging sick children's toys, especially soft toys;
- touching contaminated surfaces.
Floors in bathrooms, showers, locker rooms, shower stalls, gym mats, and ship decks are at high risk, especially in schools or public swimming pools. In general, any surface that is used by a large number of people can harbor fungi, especially if the surface is wet or damp.
Researchers estimate that at least 20% of people suffer from some form of fungal infection of the skin, hair and nails. There are groups of people who are more likely to get sick than others:
- people living in warm, humid climates;
- athletes (especially swimmers);
- children attending kindergarten;
- people working with animals;
- obese people;
- people with reduced immunity due to illness (HIV infection, organ transplantation, some types of cancer) or taking medications.
Fungal skin infections
Fungal infections of the skin and its appendages have been known since ancient times. Doctors gave skin diseases with different symptoms from others separate designations (for example, favus), not yet knowing that they were caused by fungi. The history of the science of dermatophytes began with the discovery of the favus pathogen Achorion schoenleinii in 1839 by Schonlein JL. Schonlein found fungal mycelium in the skin rashes of a patient whom he had mistakenly diagnosed as having impetigo. In 1841, Grubi D. established the relationship between skin diseases and fungi. He described the clinical picture of microsporia and the morphological features of the fungus that causes this disease. As a result of the use of the special nutrient medium proposed by Sabouraud R. for the cultivation of mushrooms, favorable conditions were created for mycological researchers. Relevant clinical and laboratory studies began to be carried out, and the era of discovery of new types of pathogens began. In the field of medical mycology, significant changes have occurred in various directions: dermatophytes, molds, yeast-like fungi, the pathogenesis of mycotic infections were studied and described in detail, the nature of actinomycosis was determined, the treatment of fungal diseases was improved, etc. Russian scientists also made a significant contribution to the development of medical mycology , among whom the most famous are P. N. Kashkin, A. M. Arievich, N. D. Sheklakov, O. K. Khmelnitsky, A. N. Arabian, Z. G. Stepanishcheva, N. A. Krasilnikov, G. O Suteev, V. M. Leshchenko and many others.
Fungal diseases have long gone beyond the specialty of a dermatologist, but dermatologists-mycologists are still doing a lot of work to combat dermatomycosis, which ranks first in prevalence in all countries.
Superficial mycoses (dermatomycosis) include infections that affect the skin, nails and hair. The main pathogens are dermatophytes, fungi that can absorb keratin. These include fungi of the genera Microsporum, Trichophyton and Epidermophyton, which, depending on the source of infection, are divided into anthropophilic, zoophilic and geophilic. The habitat of zoophilic dermatophytes (Trichophyton mentagrophytes v. gypseum, T. verrucosum, Microsporum canis, etc.) is animals, anthropophilic (Trichophyton rubrum, T. mentagrophytes v. interdigitale, Microsporum ferrugineum, Epidermophyton floccosum, etc.) is human, geophilic species ( Microsporum gypseum) live in the soil. Dermatophytes are highly contagious and can be transmitted to humans from humans, animals or soil, causing disease. The main “spreaders” of infection are anthropophilic species.
Superficial mycoses also include keratomycosis: pityriasis versicolor and piedra, which affect the most superficial areas of the stratum corneum and hair cuticle. The causative agent of pityriasis versicolor and seborrheic dermatitis, the yeast-like fungus Malassezia furfur, lives on the skin of humans and animals and, under favorable conditions, can affect the stratum corneum of the epidermis and the mouth of the follicles. The disease in most cases is not contagious. White and black piedra are usually found in countries with hot and humid climates. The diseases are less contagious. The causative agent of black piedra, Piedraia hortae, is found only on hair. Trichosporon beigelii is widespread in the environment and, in addition to white piedra, can also cause skin and nail lesions.
In addition to true dermatophytes, which infect only the skin and its appendages, superficial mycoses can also be caused by other fungi, isolated from a variety of localizations during systemic mycoses. Candida spp. - the second most common discharge in dermatomycosis and onychomycosis after dermatophytes. Up to 40% of cases of onychomycosis of the hands are caused by Candida. Lesions of yeast-like fungi on the scalp with a clinical picture of seborrheic eczema were noted. Superficial forms of candidiasis also include lesions of the mucous membranes of the oral cavity and genital organs.
In cases of onychomycosis caused by molds, there is still doubt about the ability of these opportunistic pathogens to independently infect nails due to their weak proteinase and keratinase activity. It is known that mold fungi can manifest themselves as a secondary infection, penetrating into tissues already affected by dermatophytes. However, as a result of many years of research, it has been proven that some molds can penetrate into the intercellular nail space using perforating organs. The most common causative agents of mold lesions of the skin and nails are Scopulariopsis brevicaulis, Pyrenochaeta unguis-hominis, Aspergillus spp., Fusarium spp., Alternaria spp., Cladosporium spp. and etc.
There are numerous options for the classification of fungal infections, which to a greater or lesser extent take into account the etiology, pathogenesis, clinical picture and features of the epidemiology of diseases. In domestic dermatology, the classification of N. D. Sheklakov is most often used:
- Keratomycosis (lichen versicolor, piedra, imbricated mycosis).
- Dermatophytosis (athlete's foot, trichophytosis, microsporia, rubromycosis, favus, etc.).
- Candidiasis (superficial candidiasis of the skin and mucous membranes, visceral, etc.).
- Deep mycoses (chromomycosis, sporotrichosis, etc.).
- Pseudomycosis (erythrasma, actinomycosis, nocardiosis, etc.).
However, many countries around the world have adopted a classification of fungal diseases according to the localization of the pathological process:
- Tinea pedis - mycosis of the feet.
- Tinea corporis is a mycosis of the smooth skin of the trunk.
- Tinea cruris - inguinal mycosis.
- Tinea capitis is mycosis of the scalp.
- Tinea unguim - onychomycosis.
- Tinea manum - mycosis of the hands.
- Tinea barbae is mycosis of the face.
This classification is convenient from a practical point of view, but does not take into account the etiological features of dermatophytosis, which can determine the nature of epidemiological measures and treatment features.
Main clinical features of fungal infections
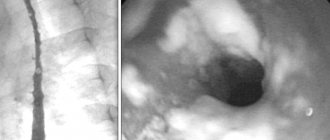
Mycoses of the feet (Fig. 1). The interdigital folds and soles are mainly affected. In the interdigital folds, slight peeling with minor inflammatory phenomena, moderate maceration, cracks, and blisters are observed. On the sole there is thickening of the stratum corneum, flour-like peeling in the skin grooves, small cracks on a slightly hyperemic background. In the dyshidrotic form, numerous blisters form on the skin of the arch and inferolateral surface of the foot, which then merge to form large blisters. In place of the opened blisters, erosions with an uneven edge remain.
Mycosis of smooth skin of the body (Fig. 2). With tinea versicolor, brownish and white spots are usually localized on the skin of the chest, back, neck and shoulders. Scaly lesions have clear boundaries and are not accompanied by inflammatory phenomena.
When the skin is damaged by other pathogenic fungi, clearly demarcated, round, swollen lesions with a raised ridge are formed. The center of the lesion is flattened, with slight peeling. The lesions increase due to peripheral growth.
Mycosis inguinal. Typical localization is the inner thigh, lower abdomen, buttocks. The lesions are clearly defined, scaly, erythematous, with an inflammatory ridge. Over time, the general moderately erythematous background gives way to a brownish one.
Mycosis of the scalp. Most often observed in children. The disease manifests itself as large, round, clearly demarcated, scaly patches of baldness. Inflammatory phenomena are mild. Discolored hair within the lesion is broken off a few millimeters above the skin level (with microsporia) or, breaking off at the skin level, leaves a stump in the form of a black dot (with trichophytosis). Zoophilic pathogens can cause the development of an infiltrative-suppurative form of dermatophytosis: the lesion protrudes above the surrounding skin, is covered with purulent-bloody crusts, and hair falls out.
Onychomycosis. Various types of fungal infection of the nail plates are characterized by loss of transparency, discoloration (whitish, yellowish), thickening, subungual hyperkeratosis, crumbling or destruction down to the nail fold.
Mycosis of the hands. In the squamous form of palm lesions, the disease manifests itself in fine-lamellar mealy peeling in the skin grooves. Cracks may form, accompanied by pain and itching. In the dyshidrotic form, vesicles form, which often cluster and can coalesce to form blisters.
Mycosis of the face. Most often, lesions are localized in the neck, chin and lower lip. The infiltrative-suppurative form of the lesion manifests itself in the formation of large bluish-red nodes with a bumpy surface. Numerous pustules merge to form abscesses. Changed dull hair in the lesion is removed easily and without pain. The superficial version resembles mycosis of smooth skin.
Laboratory diagnostics
Microscopy of clinical material is a quick and simple method for preliminary diagnosis of the disease. In cases where there is no growth of the pathogen in culture, a positive result of direct microscopy can be an undoubted confirmation of a mycotic infection. In scrapings from skin and nails, dermatophytes are usually represented by thin, 2–4 µm in diameter, straight and rarely branched mycelium. Often in the preparation one can find atypical forms of dermatophyte mycelium - chains of round arthrospores (Fig. 3).
M. furfur, when microscopy of skin scales, is revealed in the form of round cells with a diameter of 3–8 μm, collected in clusters, and short curved mycelial hyphae of a characteristic “banana-shaped” shape. In most cases, the diagnosis of lichen versicolor can be established precisely by microscopy of the native specimen, since culture of the material usually does not give results.
Scopulariopsis brevicaulis in nail scales is represented by characteristic cup-shaped spores with a rough shell.
Fungi of the genus Candida form typical budding yeast cells and pseudomycelia (branching chains of long cells).
Identification of other pathogens in native preparations is difficult.
When hair is damaged by dermatophytes, several tissue forms of the fungus are observed: 1) endoectothrix - spores with a diameter of 2–3 microns are “mosaic” located inside and mostly outside the hair, forming a muff on the root (“Adamson’s sheath”). Inside the hair you can also see mycelium, which, with light pressure on the preparation, comes out of the hair in the form of a fringe - “Adamson's brush”. The causative agent is Microsporum spp.; 2) endothrix - spores with a diameter of 4–6 microns are located inside the hair in longitudinal chains, completely filling it. The causative agent is Trichophyton spp. The final identification of fungi is carried out by cultural studies.
For cultural studies of pathological material, Sabouraud's medium with chloramphenicol and gentamicin is used, as well as for the selective isolation of dermatophytes - with cycloheximide (actidione), to inhibit the growth of fast-growing saprophytic fungi.
Dermatophyte genera are distinguished by the presence and morphology of multicellular macroconidia and unicellular microconidia.
Characteristics of the most important pathogenic fungi
Epidermophyton floccosum. Anthropophil. Affects the skin of the groin folds and legs. Colonies grow slowly, grayish-brown, lemon-olive, later white, folded-lumpy in the center. The surface of the colony is leathery or velvety-mealy. By microscopy: in mature cultures there are chains of intercalary chlamydospores. Macroconidia are 4–5-celled, club-shaped, smooth, with rounded ends. Arranged in bunches of 3–5 pieces. Microconidia are absent.
Microsporum canis (Fig. 4). Zooanthropophil. The most common pathogen of microsporia in Russia. Colonies are fast-growing, flat, radiant-hairy. The mycelium is grayish-white, against the background of a brownish-red or orange reverse side, the general hue of the colony is salmon. Under microscopy: it forms a characteristic bamboo-like mycelium, there are combs, short spirals, intercalary chlamydospores. Macroconidia are fusiform, pointed, spinous, multi-chambered (4–12 cells) with a distinct double-circuited shell. Microconidia are pear-shaped and occur inconsistently.
M. gypseum. Geophilic pathogen. It affects the skin and hair primarily of people who cultivate the soil. The colonies are fast-growing, flat, mealy (powdery), later with a small velvety elevation in the center. The color is yellowish-pink. The reverse side is yellow. Under microscopy: numerous macroconidia (4–6 cells) spindle-shaped, wide, blunt-ended, smooth. Microconidia, if present, are numerous and pear-shaped or oval.
Trichophyton rubrum (Fig. 5). Anthropophil. The most common causative agent of dermatomycosis. Affects toenails, hands and skin anywhere on the body.
The colonies are velvety, white, sometimes waxy at the beginning of growth; later they can acquire a pinkish or purple-red color. The reverse side is yellow, red or cherry red. Under microscopy: abundant microconidia of elongated, drop-shaped or pear-shaped are located on the sides of the mycelium. Macroconidia are 5–6-celled, blunt-pointed.
T. mentagrophytes var. interdigitale. Anthropophil. Affects the nail plates and skin of the feet.
Colonies are fast-growing, velvety, white, sometimes pinkish. With age, the colonies of different strains become fluffy or densely powdery. The reverse side is colorless or brownish. Under microscopy: microconidia are round, located on the sides of the mycelium, singly and in clusters. Cigar-shaped, 3–5-celled macroconidia with a rounded end are rare. In mature cultures there are many whorls and spirals, nodular organs and intercalary chlamydospores are formed.
T. mentagrophytes var. gypseum. Zooanthropophil. Affects skin and hair. In terms of frequency of isolation, it ranks second after T. rubrum.
Colonies are fast-growing, flat, granular-powdery, white, cream, yellowish. The reverse side is brownish-red. Under microscopy: microconidia are abundant, round, located on the sides of the mycelium singly and in the form of clusters. Macroconidia are cigar-shaped, 3–8 cells with rounded ends.
Treatment
Therapy for various mycotic lesions of the skin and nails is carried out with antifungal drugs, which can be systemic or applied externally. In practice, both monotherapy and various combinations of antifungal drugs are used. In most cases, treatment should be comprehensive using external antifungal agents, systemic drugs, and symptomatic treatment. Methods and means of topical therapy are mandatory components of the treatment of various mycotic skin lesions. If the fungal process is in the initial stage and there are minor skin lesions, then it can be cured by prescribing only external antifungal drugs. With a widespread or deep mycotic process, as well as in patients with damage to hair and nails, treatment may be difficult.
Antifungal drugs or antimycotics are specific agents used to treat fungal infections of the skin, nails, hair, etc. They may have fungicidal and fungistatic properties. The fungicidal effect of the antifungal agent leads to the death of fungal cells, while the fungistatic effect stops the formation of new fungal cells. Antimycotics are conventionally divided into 5 groups: polyene antibiotics, azole compounds, allylamine drugs, morpholine derivatives and medications without a clear relationship to any specific group.
When prescribing topical therapy, it is important to take into account the nature of the specific effect of the antifungal agent. It is known that griseofulvin preparations are active only against dermatophytes. External products containing polyene antibiotics - against yeast and mold fungi, preparations of selenium, zinc, benzyl benzoate - fungi of the genus Malassezia and the causative agent of erythrasma Corynebacterium minnutissium. Modern antifungal agents of the azole, allylamine, morpholine series, thiocarbamycins and pyridine compounds have a significantly wider spectrum of antifungal activity, as well as anti-inflammatory and antipruritic properties and are well tolerated.
Onychomycosis is the most treatment-resistant disease. The basis for success is an individually selected treatment regimen. When treating, it is necessary to take into account the patient’s age, concomitant diseases, the number of affected nails, and the degree of involvement of the nail plates in the pathological process.
Currently, mycologists have a large arsenal of agents with a wide spectrum of fungicidal action, accumulation in therapeutic concentrations in the nail plate and nail bed. The greatest preference is given to drugs that meet the requirements for therapeutic effectiveness, as well as aesthetics and ease of use.
Treatment of onychomycosis is divided into local, systemic, and combined.
Local treatment allows you to create high concentrations of the drug on the surface of the nail plate. However, the active ingredients of the antimycotic do not always penetrate into the nail bed, where the most viable fungi are located, in effective concentrations.
Local antimycotics: varnishes - Loceryl, Batrafen; creams - Lamisil, Nizoral, Mikospor, Mifungar, Travogen, Ecozax, Exoderil, Pimafucin, sprays - Daktarin, Lamisil, etc. It is necessary to take into account that they are not intended specifically for the treatment of onychomycosis, but they can be used in the treatment of fungal infections of the skin of the feet, interdigital gaps, often combined with onychomycosis.
To treat nails, local antiseptics are also used - alcohol solutions of iodine and dyes.
Multicomponent preparations contain an antimycotic or antiseptic in combination with an anti-inflammatory agent. In the treatment of skin infections accompanying onychomycosis, the following are used: Triderm, Travocort, Mikozolon, Pimafucort, Lorinden S, etc.
Azole, allylamine, morpholine compounds, as well as mixed group drugs are active against a large number of pathogens. Considering that quite often mycoses of the feet are caused by mixed fungal flora, it is preferable to prescribe these drugs, which are broad-spectrum antimycotics. Most of them damage the cytoplasmic membranes of fungal cell walls, suppressing the synthesis of their main components, in particular ergosterol.
Currently, the mycologist has highly effective systemic antimycotics: itraconazole (Sporonox, Orungal), fluconazole (Diflucan, Forkan), terbinafine (Lamisil), the antifungal effect of which is reflected in the table.
One of the important principles of topical therapy for mycotic skin lesions is the alternation of external antifungal drugs, which avoids resistance of dermatomycetes to them.
For squamous-keratotic forms of skin lesions, keratolytic agents are used as part of collodion peels or ointments: Arabian, Arievich, Andriasyan ointment or 5-10% Salicylic ointment. For candidal lesions, use Nystatin, Levorin, Amphotericin ointments, Pimafucin 1-2 times a day for 10-15 days. As a result of treatment, foci of candidal intertrigo, interdigital candidal erosions, and paronychia are resolved.
For acute skin mycoses with a pronounced inflammatory component, treatment begins with the elimination of swelling, hyperemia, exudation, eczematization, and allergic rashes. Lotions and wet-drying dressings with disinfectant and astringent compositions are prescribed: tannin, ethacridine, boric acid, etc. Then 2–5% boron-naphthalan paste, 5% ASD paste, as well as combinations of antifungal and corticosteroid agents in creams are used: Mycozolon, Travocort, Triderm. At the same time, acute inflammatory phenomena are quickly eliminated, which makes it possible to subsequently switch to treatment with fungicidal agents. It is recommended to use external agents with corticosteroids for 7–8 days to avoid activation of the mycotic process.
After acute inflammatory phenomena have subsided or after detachment of the stratum corneum in hyperkeratosis, azole antimycotic drugs can be used: Canesten, Clotrimazole, which are used 1 to 3 times a day, applying a thin layer to the lesions.
External dosage forms of terbinafine have high therapeutic activity: Lamisil (1% spray, cream), Lamisil Dermgel (gel). All forms have pronounced antimycotic and antibacterial properties. The presence of three dosage forms allows the mycologist to use the drug with the greatest benefit. Thus, Lamisil spray is indicated for acute mycoses with hyperemia, swelling, and rashes. The areas irrigated with the spray are covered with a thin film and isolated from the environment. Lamisil spray does not cause irritation and leads to a rapid resolution of mycosis areas: pain, itching, burning disappears, the lesions turn pale and dry out. With the help of Lamisil spray, foci of erythrasma are cured within 5 days. Within 7–10 days, recovery occurs in patients with various forms of lichen versicolor. Lamisil Dermgel, like the spray, is more indicated for acute mycoses, as it has a pronounced cooling effect and is easily applied to the affected areas. For erythematous-squamous and infiltrative manifestations of skin mycoses, the use of Lamisil in the form of a cream is indicated. The gel and cream of this drug are also effective for microsporia, lichen versicolor, candidiasis of large skin folds and periungual ridges. When using Lamisil cream for one week, a concentration of the drug is created in the skin that retains its fungicidal properties for another week after its discontinuation. This circumstance justifies short courses of treatment with Lamisil compared to other local antifungal agents.
Therapy for mycoses of the scalp, as well as in the treatment of smooth skin, is carried out with systemic and external antimycotics. Apply 2–5% tincture of iodine to the foci of mycosis and apply antifungal ointment in the evening. In cases of significant inflammation, combination drugs are used that contain, in addition to antimycotics, corticosteroid hormones. During an infiltrative-suppurative process, remove crusts with 2-3% Salicylic ointment and use disinfectant solutions (Furacilin, potassium permanganate). To increase the effectiveness of treatment, it is recommended to shave the hair on the head every 10 days.
For questions regarding literature, please contact the editor.
I. V. Kurbatova , Candidate of Biological Sciences G. A. Plakhotnaya , Candidate of Medical Sciences
IMPiTM im. E. I. Martsinovsky, MMA named after. I. M. Sechenova, Moscow
. Spectrum of activity of systemic antimycotics
Treatment and prognosis
Treatment of fungal infections (mycoses) takes from several weeks in the case of skin mycoses to months in the case of nail mycoses. Smooth skin (without hair) is usually completely restored after treatment, scarring at the site of hair loss is rare and, as a rule, hair growth is restored. A complete cure for nails affected by fungi is not always possible, and nail restoration can take a long time.
Unfortunately, there is no immunity after a fungal infection, so infection can occur again.
The information contained in this publication should not be used as a substitute for medical care or consultation with a physician.
author of the publication Mikhail Sergeevich Betekhtin, PhD, dermatovenerologist, oncologist, cosmetologist.
Diagnosis of mycoses
A dermatologist makes a preliminary diagnosis during a consultation. The nature of skin lesions during fungal infections often leaves no doubt about the existing pathology. It is possible to accurately and reliably determine the cause of changes in the skin only by studying scrapings taken from the sites of the rash. The resulting material contains pathogens in large quantities.
Staining a smear and examining it under a microscope allows you to identify mycelium threads, which indicate a fungal infection of the skin. Assessment of the morphological structure and properties of the causative agent of the disease makes it possible to determine its exact genus and species, as well as to finally determine which of the fungi caused the disease. All these diagnostic steps are important for choosing effective treatment leading to a quick recovery.
Types of disease
In the vast majority of cases, varieties of mycoses are named by the name of the pathogen: trichophyton causes trichophytosis, microsporum causes microsporia.
They differ primarily in their characteristic affected areas. Classification of mycoses:
| Type of mycosis | Affected area |
| Tinea pedis, athlete's foot | Feet |
| Tinea unguium, onychomycosis | Nails on fingers and toes |
| Tinea corporis | Skin of hands, feet and body |
| Tinea cruris, jock itch | Inguinal folds, armpits |
| Tinea manuum | Skin of the palms and back of the hands |
| Tinea capitis | Scalp |
| Tinea barbae | Scalp hair, including scalp and face |
| Tinea faciei | Skin on the face |
| Tinea versicolor, pityriasis versicolor, sun fungus | All skin |