Medical editor: Strokina O.A. - therapist, functional diagnostics doctor. September, 2021.
ICD-10 code: I35.0, I06.8, I35.8.
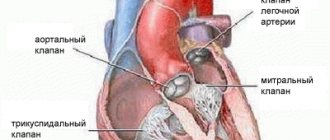
Aortic insufficiency is a malfunction of the aortic valve with the formation of reverse blood flow from the aorta into the cavity of the left ventricle. Symptoms directly depend on the amount of blood entering the ventricle. Diagnosis of pathology is possible only with the help of echocardiographic examination (ultrasound of the heart). Treatment also depends on the degree of deficiency and may involve both conservative and surgical techniques.
Aortic insufficiency is a heart defect that is characterized by the development of regurgitation (backflow of blood) on the aortic valve during the relaxation phase of the heart muscle. As a result, blood from the aorta flows back into the ventricle. There is an overflow of its volume, which in the future may threaten the expansion of the cavity of the left chambers of the heart with the development of heart failure.
During the contraction phase, the left ventricle ejects blood into the aorta, after which the ventricular relaxation phase begins. At this moment, the blood tends to return back. Her path is blocked by 3 leaflets of the aortic valve, which are “sacs”. As they fill with blood, the valves straighten, close with each other and completely close the aortic opening.
On the mitral and tricuspid valves, a small discharge of blood in the opposite direction is normally allowed, and the term “insufficiency” is not used here. In the case of the aortic valve, even minimal regurgitation is a pathology that needs to be monitored.
Causes and risk factors
Aortic valve insufficiency develops due to loose closure of the valves during the relaxation phase of the ventricles, which can develop for a number of reasons:
- idiopathic (unknown cause) dilation of the aorta;
- congenital defects of the aortic valve (usually bicuspid aortic valve);
- sclerosis of the valves (due to atherosclerosis);
- rheumatism;
- infective endocarditis;
- arterial hypertension;
- myxomatous degeneration (disorder of connective tissue development);
- dissection of the ascending aorta;
- Marfan syndrome;
- aortic valve injuries;
- ankylosing spondylitis;
- syphilitic aortitis;
- rheumatoid arthritis.
Most of these causes lead to chronic aortic insufficiency, which can be asymptomatic for a long time. Others, in particular infective endocarditis, aortic dissection, and trauma are often accompanied by a sudden development of severe aortic insufficiency. This leads to serious hemodynamic disturbances. As a result, much less blood reaches vital organs: the brain, kidneys, liver, heart.
Treatment of aortic valve insufficiency
There are two types of treatment for this pathology. Aortic insufficiency is eliminated if treated with surgery, which radically solves the problem. In this case, an artificial valve is implanted. But the positive outcome of such an operation depends on the severity of the changes that have occurred in the myocardium.
Aortic valve insufficiency is treated conservatively; treatment is aimed at reducing the symptoms of this disease, which can be eliminated temporarily. At the same time, the time of onset of heart failure is delayed. The conservative method is aimed at maintaining the functioning of the heart and improving the condition of other organs. In order to prevent cerebral circulatory failure, as well as coronary circulatory failure, it is necessary to maintain a sufficient heart rate. This becomes possible with the use of cardiac glycosides (korglykon, strophanthin and others).
Vitamins, cocarboxylase, and riboxin are also used to maintain nutrition of the heart muscle. If complications occur, their treatment is prescribed.
Types and stages
For aortic regurgitation, doctors use a classification based on the severity of regurgitation (backflow of blood). the degree is determined only by a functional diagnostics doctor based on the results of echocardiography:
- Soft (light);
- Moderate;
- Expressed.
There are many ways to define it. But all of them are possible thanks to Doppler research. All echocardiography devices have this function. It allows you to detect pathological flows inside the heart using an ultrasound sensor. One way or another, this is the most objective assessment of the severity of aortic insufficiency.
Acute and chronic deficiency are also distinguished. This is largely a clinical classification based on symptoms and how quickly they develop.
Symptoms of aortic insufficiency
The rate at which symptoms develop depends on the cause of aortic insufficiency.
Acute form
Acute aortic insufficiency develops abruptly, literally in a few minutes to hours, less often during the day. The cause is often some acute pathology, such as valve injury or aortic dissection. As a result, severe aortic insufficiency develops with large backflow of blood into the left ventricle. It's overflowing with volume. Mitral valve insufficiency develops quickly and blood stagnates in the pulmonary circulation, which can lead to pulmonary edema. If emergency measures are taken, the heart can recover almost completely.
In the acute form, acute heart failure with pulmonary edema and cardiogenic shock develops:
- severe shortness of breath,
- difficulty breathing,
- cough,
- forced position of the patient sitting,
- wheezing in the lungs,
- the appearance of foamy pink sputum,
- decreased blood pressure until loss of consciousness.
Even with intensive drug therapy, death often occurs from ventricular arrhythmias, cardiogenic shock, and pulmonary edema.
Chronic form
Chronic develops slowly. The clinic has not developed for years. A person may not be aware of the pathology and deficiency often becomes an accidental finding. Or the patient comes in with some symptoms, when the heart is greatly changed. Treatment in this case is mainly symptomatic, although in some cases surgical correction is possible.
Chronic aortic insufficiency can be asymptomatic for years. The first symptoms may be lethargy, decreased performance, fainting and presyncope. The clinical picture of heart failure is gradually developing due to volume overload of the left ventricle:
- shortness of breath during exercise, then over time at rest;
- attacks of suffocation;
- pain in the heart area of a pressing, squeezing nature, which goes away after taking nitroglycerin;
- swelling of the lower extremities, and subsequently, in the absence of adequate treatment, fluid appears in the abdominal, pleural and even pericardial cavities;
- heart rhythm disturbances - from atrial fibrillation to ventricular tachycardia. life-threatening.
Modern methods of treatment
The initial stage of the pathology does not require special treatment. The patient must regularly visit a cardiologist (once every 6 months), undergo echocardiography, ECG and other additional diagnostic methods as indicated. A person is recommended to reduce physical activity, and for rheumatism, take antibiotics and avoid staying in conditions of increased dampness.
When the first symptoms develop at the stage of relative compensation, treatment consists of using diuretics, antihypertensive drugs, and taking antibacterial agents to prevent infectious complications. The medicinal method of providing assistance cannot completely eliminate the problem, but only acts on the cause and improves a person’s quality of life.
Types of prostheses and the difference between them
Plastic surgery or replacement of the valve and ascending aorta is recommended at the onset of hemodynamic decompensation. Emergency surgery is also performed if an acute aneurysm develops or if a valve is damaged due to a strong blow to the chest.
Surgical treatment of aortic valve insufficiency is usually performed using artificial and biological implants. The former are created from metals with an intact coating, and the latter are divided into three types:
- xenografts (created from animal tissue);
- homografts (material from another person is used);
- autografts (taken from the person being operated on).
Previously, all operations were performed on an open heart. Transcatheter implantation is currently practiced. This is a minimally invasive technique that involves inserting an artificial valve through an opening in a vessel without making an incision in the chest.
There are several types of prostheses on the market for such an operation:
- Medtronic CoreValve. Introduced transfemorally (through the femoral artery), it consists of a frame and three leaflets, which are made from the pericardium of pigs.
- Placed using transapical access (through the apex of the heart).
- Made from the pericardial sac of a bull, and a stainless steel ring is used as fastening.
After a week's stay in the hospital, the person is discharged under the supervision of his doctor. Sometimes hospital stay is extended to 10 days.
The main rehabilitation consists of properly selected drug support, which will prevent possible complications and speed up the process of returning a person to a normal lifestyle. The treatment protocol in this case includes the following groups of drugs:
- immunosuppressants are necessary to suppress the process of transplant rejection;
- antibiotics prevent infectious complications;
- anticoagulants prevent the formation of blood clots on artificial valves
- antiplatelet agents that thin the blood.
Medical treatment of the patient after surgery will include drugs to treat conditions that caused the defect or aggravated the course of the disease.
Surveys
Examination of a patient always begins with examining and listening to the heart. Already at this stage, the doctor is able to suspect a valve defect by the presence of a heart murmur. It is also possible to decrease diastolic (lower limit) blood pressure and, as a result, increase pulse pressure (the difference between the upper and lower limits of blood pressure). However, such signs of aortic insufficiency are detected only in chronic pathology, when the clinical picture of heart failure described above is already clearly manifested.
Instrumental methods are the only way to detect regurgitation on the aortic valve.
Echocardiography (ultrasound of the heart)
First line diagnostic method. It detects backflow of blood through the aortic valve. The doctor determines the degree of its severity and the possible cause - for example, trauma, vegetations on the valve (accumulations of bacteria on the valves - a sign of infective endocarditis), volumes of the left chambers of the heart, left ventricular ejection fraction and many other morpho-functional indicators.
Magnetic resonance imaging (MRI)
Used only if echocardiography is not available or visualization of the heart and its structures is extremely difficult.
Multislice computed tomography angiography and magnetic resonance imaging angiography (both contrast-enhanced procedures) are used in patients with a bicuspid aortic valve to evaluate the initial aorta to its arch, but only if echocardiographic findings are unsatisfactory.
X-ray of the chest organs
Used to assess the size of the heart and ascending aorta.
Electrocardiogram (ECG)
Allows you to identify rhythm disturbances, conduction disorders in the heart and signs of myocardial hypertrophy.
The methods listed are more than enough to make an accurate diagnosis of aortic insufficiency and begin treatment on time.
Diagnostic tests
Common tests to diagnose aortic valve regurgitation include:
- Echocardiogram.
This test uses sound waves to produce an image of your heart. In echocardiography, sound waves are sent to your heart from a wand-like device (transducer) placed on your chest. Sound waves bounce off your heart and are reflected back through your chest wall and processed electronically to provide video images of your heart. An echocardiogram allows your doctor to take a close look at your aortic valve. A certain type of echocardiography, Doppler echocardiography, may be used. This allows measurements of the volume of blood that flows in the opposite direction through the aortic valve. This volume is expressed in cubic centimeters per beat. - Chest X-ray.
Using a chest X-ray, your doctor can examine the shape and size of your heart to determine whether your left ventricle is enlarged, a possible sign of damage to the aortic valve. - Electrocardiogram (ECG).
In this test, wires (electrodes) are attached to your skin to measure electrical impulses from your heart. The pulses are reflected as waves displayed on a monitor or printed on paper. An ECG can provide information about whether the left ventricle is enlarged, a problem that can occur with aortic valve insufficiency. - Transesophageal echocardiography.
This type of echocardiography allows you to take a closer look at your aortic valve. A “sensor tube” is inserted through your esophagus and goes into your stomach and is closer to your heart. In traditional echocardiography, a device called a transducer moves on your chest to produce the sound waves needed to create a picture of your beating heart. In transesophageal echocardiography, a small probe is attached to the end of a tube and passed through the esophagus. This is done to better visualize the image of your aortic valve and the bleeding through it, since the sensor is closer to the valve itself. - Exercises, tests.
Various types of exercise tests to assess activity tolerance and test your heart's response to exercise (sports). - Cardiac catheterization.
Your doctor may order this procedure if noninvasive tests have not provided enough information to firmly diagnose the type and severity of your heart disease. The doctor threads a thin tube (catheter) through a blood vessel in your arm or groin and into your heart. A contrast agent is injected through a catheter in your heart, making details visible on an X-ray. Cardiac catheterization can show if blood is flowing back from the aorta in the heart into the left ventricle. Some catheters are equipped with special sensors that can measure pressure within the chambers of the heart. Pressure may be increased in the left ventricle with aortic valve insufficiency.
ECG
These tests help doctors diagnose aortic valve regurgitation, determine how severe the problem is, and decide whether your aortic valve needs replacement.
Treatment
Aortic insufficiency is treated by a cardiologist and cardiovascular surgeon.
Drug treatment
Drug treatment is prescribed depending on the cause of aortic insufficiency. It is considered as an option in preparation for surgery or to reduce the symptoms of heart failure and alleviate the condition of patients who have contraindications to surgical treatment.
For rheumatism and infective endocarditis, a course of antibacterial therapy is prescribed. In the first case, penicillin antibiotics (benzathine benzylpenicillin) are used to prevent exacerbation of the disease. For infective endocarditis, amoxicillin, ceftriaxone, gentamicin, and, less commonly, vancomycin are usually prescribed for a long course of 2 weeks. Drugs are prescribed based on the clinic and the resistance of bacteria to them. Can be used as a single drug or in combination.
Treatment of arterial hypertension consists of prescribing ACE inhibitors (perindopril, enalapril, lisinopril) or sartans (valsartan, losartan) and dihydropyridine calcium antagonists (nifedipine, amlodipine).
Beta blockers (bisoprolol, metoprolol, nebivolol) are added to treatment in the case of reduced cardiac ejection fraction as determined by echocardiography.
Surgery
Aortic valve replacement is the only possible method of valve correction.
It is recommended for patients with:
- severe aortic regurgitation and the presence of symptoms regardless of ejection fraction;
- asymptomatic chronic severe aortic regurgitation and ejection fraction less than 50%;
- chronic aortic regurgitation in parallel with coronary artery bypass surgery or surgery on the aorta and other heart valves;
- asymptomatic severe aortic regurgitation with normal ejection fraction. on significant expansion of the left ventricle (EDV - more than 75 mm).
The duration of treatment for patients with aortic insufficiency varies greatly depending on the severity of the condition and the cause of the pathology. After the operation, it is recommended to undergo a course of rehabilitation in a cardiological sanatorium or rehabilitation center. The recovery period is at least 3 months, after which the patient can resume work with the doctor’s permission.
Symptoms
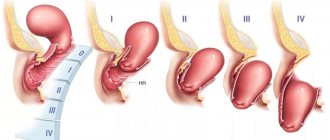
The disease manifests itself differently depending on the degree of neglect of the pathology. For comparison, here is a table of signs of the disease by stage:
| Stage | Degree of regurgitation in % | Complaints | Signs upon examination |
| I. Full compensation | 15 | none | there are no deviations, the appearance of a slight noise at the time of diastole during auscultation |
| II. Aortic insufficiency degree 2 (hidden) | 15-30 | the appearance of unpleasant sensations in the chest after physical activity, pulsation in the head and neck, rapid heartbeat | increased heart rate |
| III. Subcompensation | 50 | pain syndrome like angina pectoris at rest, dizziness, tinnitus, blurred vision, fainting, head shaking, pulsation of the pupils and vessels of the nail bed | enlarged liver, pasty legs, pallor, galloping pulse, weakening of the first and second tones, increased difference between systolic and diastolic pressure |
| IV. Decompensation | from 50 and more | progressive failure, dysfunction of all organs, arrhythmia, severe edema | acrocyanosis, anasarca, hepatosplenomegaly, uneven pulse, visual determination of the cardiac impulse, its displacement to the 7th intercostal space |
The compensatory stage can last a long time without showing itself in any way if the cause is a chronic process.
Complications
Complications of aortic insufficiency develop as its severity increases. At the beginning, normal syncope (fainting) may appear due to insufficient blood supply to the brain. Conduction disorders in the form of blocks of the left bundle branch and atrioventricular conduction of impulses can also often occur in patients with aortic insufficiency.
Coronary insufficiency can accompany aortic insufficiency, but more often in combination with aortic valve stenosis. The patient develops attacks of angina (pain in the heart of a pressing, squeezing nature) and even myocardial infarction.
Heart failure is the most common complication of already severe aortic regurgitation. The patient complains of shortness of breath during physical exertion, asthma attacks, and swelling of the lower extremities.
Sudden death often develops as a result of life-threatening arrhythmias - paroxysmal ventricular tachycardia, ventricular fibrillation. In this case, the person does not even have time to call an ambulance - the arrhythmia develops so quickly.
Forecast
The prognosis for aortic insufficiency is better, the lower the degree of regurgitation and the earlier treatment is started. Preventive examination by a general practitioner, cardiologist, full antibiotic therapy in case of infective endocarditis and rheumatic fever - all this helps to improve the prognosis. It is very important to listen to yourself, your body, so as not to miss the first symptoms (lethargy, decreased performance, fainting, shortness of breath during physical activity).
Usually, with severe clinical heart failure, the prognosis worsens, since irreversible changes occur in the structure of the heart.