Introductory part
Before heart surgery, a person has many questions. Some of them we ask the doctor, and some we cannot even formulate. When we understand what is happening to our body and what we can do to restore health, it is easier for us to endure all procedures.
Acquired heart valve defects
- these are diseases that are based on morphological and/or functional disorders of the valve apparatus (valve leaflets, annulus fibrosus, chordae, papillary muscles), developed as a result of acute or chronic diseases and injuries, disrupting the function of the valves and causing changes in intracardiac hemodynamics.
Valve defects can be congenital or acquired.
Congenital defects occur when the structures of the heart are formed incorrectly during intrauterine development; sometimes they do not make themselves felt until adulthood. Acquired defects arise due to rheumatism, infection, metabolic disorders (when calcium is deposited in the valves), trauma and other reasons.
The main types of heart valve defects:
- mitral stenosis
- mitral valve insufficiency
- mitral valve prolapse
- aortic stenosis
- aortic valve insufficiency
- tricuspid stenosis
- tricupidal insufficiency
The normal functioning of the heart largely depends on the functioning of its valve apparatus.
Obstacles to the passage of blood cause overload, hypertrophy and expansion of the structures above the valve. Obstructed heart function disrupts the nutrition of the hypertrophied myocardium and leads to heart failure.
Etiology and pathogenesis
Etiology of stenosis
and combined rheumatic disease,
insufficiency
- usually rheumatic, rarely septic, atherosclerotic, traumatic, syphilitic.
Stenosis is formed as a result of cicatricial fusion or cicatricial rigidity of the valve leaflets and subvalvular structures; valve insufficiency - due to their destruction, damage or scar deformation.
Failure
valve damage occurs due to destruction or damage to its valve flaps. Valve insufficiency is characterized by incomplete closure of the leaflets and occurs as a result of their wrinkling, shortening, perforation or expansion of the fibrous valve ring, deformation or separation of the chordae and papillary muscles. In some cases, valve insufficiency develops as a result of dysfunction of the valve apparatus, in particular the papillary muscles.
Often stenosis and insufficiency develop on one valve (the so-called combined defect
).
In addition, there are cases when the defects affect two or more valves - this is called combined
heart disease.
Affected valves form an obstacle to the passage of blood - anatomical in case of stenosis, dynamic in case of insufficiency. The latter is that although some of the blood passes through the hole, it returns back in the next phase of the cardiac cycle.
A “parasitic” volume is added to the effective volume, performing a pendulum-like movement on both sides of the affected valve. Significant valvular insufficiency is complicated by relative stenosis (due to increased blood volume). Obstruction to the passage of blood leads to overload, hypertrophy and expansion of the overlying chambers of the heart.
The expansion is more significant with valve insufficiency, when the overlying chamber is stretched by additional blood. With stenosis of the atrioventricular orifice, the filling of the underlying chamber is reduced (left ventricle with mitral stenosis, right ventricle with tricuspid stenosis); There is no hypertrophy or expansion of the ventricle.
With valve insufficiency, the filling of the corresponding ventricle is increased, the ventricle is dilated and hypertrophied. Difficulty in the functioning of the heart due to improper functioning of the valve and degeneration of the hypertrophied myocardium leads to the development of heart failure.
to the top of the page
Pulmonary valve
The pulmonary or pulmonary valve is the next valve through which deoxygenated blood passes. It closes the right ventricle and opens to allow blood to enter the lungs. Pulmonary valve stenosis
causes this valve to thicken over time, narrowing its opening and causing blood to flow more slowly.
Pulmonary valve insufficiency
prevents complete closure, causing blood to flow back into the right ventricle.
A rare disorder of the pulmonary valve called pulmonary atresia
, means that a person is born without this valve.
Anatomy of the heart
A healthy heart is a strong, continuously working organ, about the size of a fist and weighing about half a kilogram.
In addition to maintaining steady, normal blood flow, it quickly adapts and adapts to the body's ever-changing needs.
For example, the heart pumps more blood when it is active and less when it is at rest. During the day, the heart produces an average of 60 to 90 beats per minute - 42 million beats per year!
The heart is a two-way pump that circulates blood throughout the body. It consists of 4 chambers.
A muscular wall called the septum divides the heart into left and right halves. Each half has 2 chambers.
The upper chambers are called atria, the lower chambers are called ventricles. The right atrium receives all the blood returning from the upper and lower parts of the body.
Then, through the tricuspid valve, it sends it to the right ventricle, which in turn pumps blood through the pulmonary valve to the lungs.
In the lungs, the blood is enriched with oxygen and returns to the left atrium, which sends it through the mitral valve to the left ventricle.
The left ventricle pumps blood through the arteries through the aortic valve throughout the body, where it supplies the tissues with oxygen. Oxygen-depleted blood returns through the veins to the right atrium.
Four valves (tricuspid, pulmonary valve, mitral, aortic) act as a door between the chambers, opening in one direction.
These valves help blood move forward and prevent it from flowing in the opposite direction.
The petals of a healthy valve are thin, flexible tissue of perfect shape. They open and close when the heart contracts or relaxes.
Heart valves can become abnormal due to birth defects. They can become damaged or scarred due to rheumatic fever, infection, hereditary factors, age or heart attacks.
The mitral valves are most susceptible to such changes.
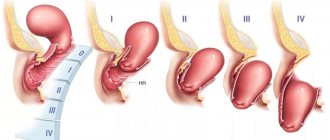
Regardless of the case, the heart valve can become stenotic (narrowed opening) or insufficient (does not close completely).
With valve stenosis, the heart must work harder to pump the required amount of blood through the narrowed opening.
Valve insufficiency causes blood to flow backwards through the valve after it closes. Once again, the heart has to work harder to pump enough blood for the body's needs to make up for the deficiency caused by the backflow of blood.
Both cases - stenosis and failure - force the heart to work harder to pump the required amount of blood. This extra work can weaken the heart, cause it to enlarge, and cause various diseases.
to the top of the page
Tricuspid valve
The tricuspid or tricuspid valve is so named because it has three leaflets. Blood passes through this valve after leaving the right atrium. After passing through the tricuspid valve, the blood enters the right ventricle.
People with a rare condition called tricuspid atresia
, are born without a tricuspid valve, which means that blood cannot flow from the right atrium to the right ventricle.
Tricuspid insufficiency
means the tricuspid valve fails to close completely, while
tricuspid valve stenosis
causes the valve to thicken, narrowing its opening.
Diagnosis of heart valve diseases
After listening to the symptoms you describe and examining your medical record, the doctor will measure your pulse and blood pressure and listen to your heart using a stethoscope.
If your doctor suspects that you have a heart disease, he may ask you to undergo a series of special diagnostic tests that will help make an accurate diagnosis and prescribe the necessary treatment.
One of these research methods is a non-invasive method, i.e. which does not require any internal intervention.
Another type of research is invasive: with the help of instruments inserted into the body, which, as a rule, causes only minor inconvenience to the patient.
Chest X-ray
This test allows the doctor to obtain valuable information about the size of the heart, heart chambers and the condition of the lungs.
Electrocardiogram (ECG)
An electrocardiogram monitors the electrical current passing through the heart and stimulates the chambers to contract. An ECG is especially useful in diagnosing abnormal heart rhythms and rates.
These studies also show muscle enlargement or damage, and the presence of congestion on one side or another of the heart.
Echocardiogram (EchoCG)
This test is carried out using a “small” microphone placed on the surface of the chest, which emits high-frequency sound waves.
Sound waves are reflected back (hence the term "echo") from each layer of the heart wall and valves and then displayed on a monitor screen. The “echo” image from different points allows you to see a cross-section of the heart at the moment of its operation.
During the echo, the speed of blood flow is also recorded, the direction of blood movement is monitored: is the blood moving in the normal forward direction or is there a reverse movement (as in the case of valve insufficiency).
A narrowed (or stenotic) valve causes increased blood flow. The degree of valve stenosis is in many cases accurately determined by the increased blood flow velocity.
This test will not only show how the heart valves work, it will also provide useful and comprehensive information about the size of the heart chambers, as well as the thickness and function of the heart muscle.
Cardiac catheterization and angiogram
These tests are done by inserting a thin, hollow tube (catheter) through a vein or artery in the arm or groin area and into the chambers of the heart, using X-rays.
During catheterization, the pressure in the chambers of the heart is measured and the volume of blood in the bloodstream is determined.
Angiography consists of the injection of a radiopaque contrast agent, which is visible using X-rays and allows you to evaluate the work of the heart in pumping blood, the function of the valve and the patency of the arteries (coronary) that supply blood to the heart muscle.
Despite the fact that similar studies have been routinely carried out before, it is not at all necessary that they are needed in your case if the information obtained by echocardiography is complete and accurate.
In many cases, the only invasive test required before surgery is a coronary angiogram if it is determined that the patency of one or more arteries is impaired.
If there are blockages in the coronary arteries, the doctor will usually perform bypass surgery at the same time as heart valve surgery.
to the top of the page
The structure of the aortic valve, its function
The aortic valve (AV) demarcates the left ventricle and the aorta, preventing backflow of blood during diastole (the relaxation phase of the myocardium). Another name for it - semilunar - reflects the structural features, since the AC is formed by three convex pockets (flaps).
Anatomy
The AC is located in the initial section of the vessel - the aortic bulb, which is projected onto the chest in the center of the sternum, between the cartilages of the third ribs.
The structure of the AK is very complex; the valve consists of:
- three semilunar valves (or valves);
- fibrous ring;
- commissure
Sometimes it is supplemented with sinuses of Valsalva and triangles of Henle. These elements anatomically do not belong to the aorta, but take part in the work of the structure.
The fibrous ring consists of connective tissue bundles formed by collagen and elastic fibers. The element forms the boundary between the ventricle and the aortic bulb, being the attachment point for the valves.
The valves are the main functional part of the AK. In their shape, they resemble pockets that extend from the walls of the aorta, their base attached to the fibrous ring. The free edge of each valve is slightly elongated and contains the Arrantian node at the end.
There are three flaps: right, left and rear. Opposite each are the so-called sinuses (or sinuses) of Valsalva - the entrance gates of the coronary vessels that supply the myocardium of the heart.
Commissures are the contact lines between the edges of the valves when the valves are closed. The normal activity of the heart largely depends on the density of their articulation.
Histology
All valves, including the aortic valve, are formed from the endocardium - the inner lining of the heart, mainly consisting of epithelial cells. However, each structure has its own characteristics:
- The fibrous ring is formed by connective tissue, which gives a certain rigidity and density. The need for such a structure is caused by the large hemodynamic load to which the element is exposed.
- The valves are formed by three layers of connective tissue: fibrous (or aortic), spongy and ventricular. They contain a large amount of collagen and a small amount of elastin. On the outside, each leaflet is covered with a thin endothelial membrane.
- The sinuses of Valsalva have a thinner wall than the aorta. The latter consists of two layers: intima and media. Towards the heart, the amount of collagen decreases and elastin increases.
During embryogenesis, the AC develops from mesenchyme, like all tissues of the left ventricle.
Physiology
The physiological significance of the AC is enormous, since the valve regulates the normal flow of blood from the ventricle into the systemic system, which nourishes the entire body. In addition, adequate closure of the valves takes part in the filling of the coronary arteries.
The valve operates passively, under the influence of blood coming from the heart. The whole process is divided into two stages - periods of opening and closing of the valves.
The discovery phase contains several stages:
- Preparatory. At this moment, the heart is in the phase of isovolumetric (constant chamber size and volume) contraction. At the same time, all valves are closed, and during muscle tension the pressure in the left ventricle quickly increases. In addition, the aortic root expands, causing the valves to begin to open before there is a difference in pressure on both sides.
- Rapid opening begins at the moment when the pressure in the ventricle exceeds the value in the aorta, after which blood rushes out of the heart, pushing through the valves.
- Peak opening coincides with the rapid expulsion phase. At this time, the valves are tightly pressed to the sinuses of Valsalva, the lumen approaches the shape of a circle.
The closing period consists of two phases:
- The sustained opening corresponds to the slow expulsion phase. The pressure begins to equalize, the valves partially move away from the walls, the lumen more closely resembles the shape of a triangle.
- Quick closing. Due to the slow flow of blood, small turbulences form near the walls. Reaching the sinuses, they penetrate the valve pockets and push the valves to the center, thereby closing them.
When the valves slam shut, they emit a sound, which upon auscultation is recorded as the 2nd tone. Additional noise occurs from reverse blood flow during diastole when fluid impinges on the closed valve.
Heart valve surgery
Often heart defects do not manifest themselves for a long time, because the heart adapts to working under overload. In the case where the heart defect is “moderate” and does not lead to serious overload of the heart, in some cases they are limited to observation or drug therapy. But when the defect is severe, it must be treated surgically.
The following operations are performed on heart valves: reconstruction or complete replacement of a damaged valve.
Heart valve reconstruction
Sometimes during surgery it is possible to preserve the valve flaps and only correct their shape. This procedure is called valve repair.
.
Sometimes the shape of the valve can be restored by strengthening its base with threads, or by sewing a special ring to the base, while the valve’s own flaps are preserved. This procedure is called annuloplasty.
, it is possible only for the mitral and tricuspid valves.
Valve reconstruction can largely restore its function. For severe heart valve damage, valve replacement surgery may be the only treatment option. The results of these operations exceed the effect of drug therapy. Today, heart valve surgery can be performed on patients of any age group.
Access for operations on the aortic valve or on several valves simultaneously is made through an incision in the center of the sternum. When performing operations on the mitral valve, it is possible to use the “keyhole technique,” when surgical access is made through a small incision in the projection of the mitral valve: on the side and below the chest.
When it is impossible to save the leaflets of the native valve, or if they are preserved, there is a high probability of the defect returning and repeated surgery, the native valve is excised and implanted in its place
artificial
valve prosthesis
.
The most commonly performed surgeries are mitral valve reconstruction. In this case, the own valve is preserved - this is very important.
, Ross surgery is performed to treat aortic disease.
. The damaged aortic valve is replaced with the patient's own pulmonary valve, which is similar in structure, and an artificial prosthesis is implanted instead of the excised pulmonary valve.
When the aortic valve and aortic wall are damaged, it may be necessary to replace the ascending aorta with a valve-containing aortic graft
(sometimes called a conduit). In this case, not only the aortic valve is replaced, but also the adjacent ascending aorta.
Your attending physician will inform you about the possibility of reconstructive surgery on the heart valve in your case. In some cases, the question of the possibility of valve reconstruction is decided during the operation: if reconstruction is not possible, then an operation is performed to replace the damaged valve.
Aortic valve
The aortic valve is the last valve through which oxygen-rich blood passes before leaving the heart and throughout the body. The valve prevents blood from flowing back into the left ventricle.
Aortic regurgitation
, or
aortic valve regurgitation
, means that the aortic valve does not close completely, allowing blood to pass backwards.
Aortic valve stenosis
means the aortic valve thickens or hardens, narrowing the path through which blood can flow. This delays or prevents normal blood flow to the rest of the body.
Heart valve problems fall into two broad categories:
Conclusion
Defects of the mitral and aortic valves are more common than those of the pulmonary valve. Valvular insufficiency of the left side of the heart usually follows after the left side fails at the stage of decompensation; and then the right side of the heart “breaks.”
Infectious endocarditis is also considered a common cause of pulmonary valve defects. Older people are advised to prevent endocarditis and consult a cardiologist more often for a routine examination.
However, if it is nevertheless diagnosed after a detailed study, then the patient needs to completely reconsider his life.
Prevention of the development of defects
The best prevention of valve dysfunction at all times is to maintain a healthy lifestyle. No vitamin supplements or “golden formulas” of youth will help maintain health if a person smokes from a young age and does not follow a sleep-wake schedule.
The human heart is a very vulnerable organ. Smoking and alcohol cause irreparable harm to him. And another factor for heart health is that humans are designed to move. At any age, he should play sports, but in moderation. Heavy loads for the sake of results are also harmful.
Women during pregnancy should avoid various mutagenic factors and not take medications without consulting their doctor. Many drugs in the prenatal period can lead to pulmonary valve defects.
Isolated stenosis in the pulmonary trunk in the neonatal period
Isolated stenosis, that is, stenosis not associated with other heart diseases, is formed in the intrauterine (neonatal) period of fetal development in the following cases:
- the mother suffered from rubella during pregnancy;
- has diabetes of the 1st or 2nd degree;
- the woman drank alcohol;
- genomic damage;
- substances in the mother’s body such as isotretinoin, used to treat seborrhea, also lead to defects; or hydantoin, a substance used in anti-convulsant medications.
Clinical manifestations of pulmonary valve stenosis in newborns occur in different ways. In mild cases, the defect does not make itself felt and is asymptomatic. And in severe cases, from the first days of life there is a severe lack of blood supply to the tissues and cyanosis.