Symptoms of a neurogenic bladder
There are several clinical options, determined by different levels of damage, the nature of manifestations, severity, and duration of the disease.
Main symptoms:
- frequent urination, including at night;
- sudden urge to defecate immediately;
- urinary incontinence.
With the hyperactive type, more than 250 ml of urine never accumulates in the bladder, voluntary urination is difficult, and there is practically no urge to urinate. Characteristically, there are symptoms of damage to the autonomic nervous system: sweating, periodic rises in blood pressure.
With the hypoactive type, there is no increase in intravesical pressure even with a large volume of urine. The detrusor does not respond to stretching. When the bladder becomes full, the internal bladder sphincter stretches, causing urine to be released in uncontrollable drops or a sluggish stream.
1. Why bladder dysfunction occurs
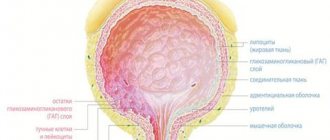
The bladder is one of the few organs whose work is associated with consciousness. The accumulation of urine and the urge to urinate occur with the participation of humoral regulation, but a person is able to control the moment of emptying the bladder. The nervous system sends signals about the need to remove urine from the body, and it also triggers mechanisms that contract the bladder and open the urine exit channels. This is a rather complex process, violations of which lead to a functional pathology called “neurogenic bladder.” The walls of the bladder may become hypotensive or, conversely, become hypertonic. In both cases, control over the process of urination suffers, which causes a lot of inconvenience to the person.
As the bladder fills, signals are sent to the brain to empty it. When a person goes to the toilet, the conscious readiness to urinate is complemented by brain impulses that ensure the contraction of the bladder walls and the removal of urine from the body.
A complex chain of conscious and unconscious mechanisms must work very harmoniously. Otherwise, if at some stage the nerve impulses do not pass through or are distorted, the person experiences difficulty urinating or loses control over this act.
Dysfunction of the neuromuscular structures of the bladder not only brings discomfort to the patient’s life, but can also cause the development of concomitant diseases of the urinary system: pyelonephritis, cystitis, nephrosclerosis and chronic renal failure. Long-term problems with urination create a tense psycho-emotional background, which, combined with disorders of fluid metabolism in the body, provokes arterial hypertension in many patients.
A must read! Help with treatment and hospitalization!
Treatment of neurogenic bladder
The treatment plan is drawn up individually, depending on the cause that caused the syndrome. General principles:
- normalize detrusor tone;
- improve blood supply to the pelvic organs;
- relieve nervous tension;
- relieve irritation of the autonomic nervous system.
Drug therapy, exercise therapy, physiotherapy, and psychotherapy are used.
In some cases, surgery is performed.
Primary appointment (examination, consultation) with a urologist
1850 rub.
Sign up
Complications and consequences
Most congenital diseases of the nervous system in children affect the quality of urination, but neurological symptoms often come first. Complications of impaired urination occur faster than in adults.
- Mental disorders (anxiety, depression, sleep disturbances) that reduce the level of quality of life.
- With inadequate treatment, the disease can lead to serious consequences for the patient’s health - the development of chronic cystitis (inflammation of the bladder), vesicoureteral reflux (reflux of urine from the bladder back into the ureters and kidneys, followed by their atrophy and the development of chronic renal failure), pyelonephritis ( microbial inflammatory kidney damage), etc.
Why is it better to treat a neurogenic bladder at Major Clinic?
The clinic, conveniently located in the center of Moscow, has a urology department equipped with modern diagnostic equipment. Analyzes are done in our own laboratory. Patients are received by highly qualified doctors who are able to quickly and efficiently conduct examinations, prescribe treatment, and perform surgery in the clinic’s operating room. Safe and effective techniques are used, as a result of which all patients go home with recovery and a significant improvement in well-being.
History taking
First, the doctor collects the patient’s medical history, which includes the following information: the nature of urination disorders, the presence of intestinal disorders and general symptoms such as headache, malaise, dry mouth, previous diseases of the nervous system, head and spine injuries, spina bifida.
In addition, the doctor must determine whether the patient has sensory disturbances (feeling of incomplete emptying, pressure or fullness in the lower abdomen, lack of urge to urinate). For an accurate diagnosis, behavioral symptoms should also be taken into account: restriction of fluid intake, control urination, inability to urinate in front of strangers (medical staff).
Diagnostics
Since the disease is multisystem in nature, diagnosis begins with a detailed history. If a neurogenic etiology is suspected, the doctor will recommend keeping a special diary. In it, patients record the frequency and time of urination, and the approximate volume of urine. Accurate documentation allows you to objectively assess the scale of the problem.
In addition, the specialist will prescribe hardware and laboratory diagnostics:
- pelvic radiography;
- excretory urography;
- Ultrasound of the kidneys;
- Ultrasound of the bladder;
- Ultrasound of the ureters;
- bacteriological examination of urine;
- serum creatinine.
Phenomenology of neurogenic urinary disorders
The process of differential diagnosis is complicated by the fact that LUTS are characteristic manifestations of diseases of the bladder, prostate and urethra that may affect a neurological patient. Despite the fact that in the International Statistical Classification of Diseases and Related Health Problems (ICD 10), neuromuscular dysfunction of the bladder (synonymous with “neurogenic bladder”) is identified as an independent disease and has code N31, the obvious statement is that that the symptoms of urinary disorders are just one of the manifestations of a disease of the nervous system. N31 Neuromuscular dysfunction of the bladder, not elsewhere classified: N31.0 Uninhibited bladder; N31.1 Reflex bladder; N31.2 Neurogenic bladder weakness; N31.8 Other neuromuscular dysfunctions of the bladder; N31.9 Neuromuscular dysfunction of the bladder, unspecified. If we assume that neurogenic dysfunctions of urination are an independent disease, then there is no way to explain their pathogenesis. On the contrary, if we assume that LUTS is a neurological symptom, then it is obvious to assume its origin through comparison with the function of the parts of the nervous system that regulate urination. The most acceptable method for analyzing the origin of LUTS is deduction, i.e. a method of thinking in which a particular situation is logically deduced from the general, a conclusion according to the rules of logic. An example of a deductive inference: • parasympathicotonia in Parkinson's disease (PD) is characterized by the presence of three symptoms (overactive bladder (OAB), spastic constipation and hypersalivation); • taking an anticholinergic drug (for example, trospium chloride) relieved all three symptoms; • therefore, OAB was a manifestation of parasympathicotonia. This conclusion reveals the general pathogenetic mechanism of three, at first glance (both the doctor and the patient), unrelated symptoms. The vision of this community allows us to reduce the number of prescriptions for a given patient from three drugs to one - an anticholinergic mechanism of action. The opposite of deductive reasoning is inductive reasoning: • taking an anticholinergic drug (for example, trospium chloride) did not relieve the symptoms of OAB in a patient with PD; • the patient has PD; • therefore, OAB in PD is not associated with parasympathicotonia. This conclusion from the particular to the general casts doubt on a proven fact based on a single observation. As a result, OAB syndrome is not considered neurogenic, and if a patient is diagnosed with benign prostatic hyperplasia (BPH), he undergoes transurethral resection of the gland. The result of such an operation (according to the literature) in 65% of cases is total urinary incontinence. There is an obvious error in reasoning. OAB syndrome in PD can develop against the background of decreased stimulation of dopamine receptors in the bladder. In this case, the patient receiving antiparkinsonian therapy does not even suspect that he has a hidden urinary disorder. It only appears when there is an error in taking medications. The nature of the complaint may indirectly indicate the location of the lesion in the nervous system. Table 1 shows the most common complaints detected when certain areas of the nervous system that regulate the normal act of urination are damaged. As can be seen from the table, damage to individual functionally significant areas of the central nervous system leads to the formation of strictly defined pathological LUTS. A prerequisite for the development of these symptoms is the nature of the nervous system disease (ischemic damage, demyelination, neurodegeneration). The appearance of a combination of symptoms in a patient with the subsequent formation of syndromes of impaired urination indicates a steady progression of the pathological process with the involvement of a large number of new areas of the nervous system (multi-infarct form of dyscirculatory encephalopathy (MIGE), subcortical arteriosclerotic encephalopathy (SAE) or multisystem atrophy (MSA)). In some localizations of damage, similar symptoms may be observed (for example, the need to strain to start and continue urination in the presence of a focus of ischemia in the region of the islet of Reil, trunk or lumbosacral segments of the spinal cord). In this case, it is necessary to compare the “urological symptoms” with neurological signs. The areas of damage given as an example are usually accompanied by a pronounced neurological picture, including disorders of movement, breathing, vision, swallowing, and cognitive impairment. Analysis of known symptoms and the time of their onset makes it possible at the initial appointment to differentiate some diseases with similar neurological symptoms (for example, PD and MSA). Thus, OAB syndrome in PD develops by the 5th–6th year of the disease, while in MSA it develops in the 1st–2nd year. Differences are also noticeable in the composition of symptoms within one syndrome. In PD, OAB syndrome consists of frequent nighttime urination up to 4–5 times in full portions (250–300 ml) and a decrease in daytime urination up to 2–3 times, and MSA is characterized by the presence of imperative, less often orthostatic, urinary incontinence. The frequency of occurrence of symptoms for different diseases also differs. In PD, OAB syndrome is detected in 25% of patients, while in MSA – in 80–100%. The frequency of occurrence of the main syndromes of urination disorders in various diseases of the nervous system is presented in Table 2. As can be seen from the table, urination disorders in various diseases of the nervous system differ not only in frequency of occurrence, but also in qualitative composition. This is due to fundamental differences in the pathogenesis of diseases. When differentiating between vascular and Alzheimer's dementia, the timing of LUTS can be a useful guide. For vascular dementia, OAB syndrome is one of the earliest signs and is combined with the initial manifestations of leukoaraiosis, detected by neuroimaging. While in dementia of the Alzheimer's type, urinary incontinence is extremely rare and indicates the destruction of the core of personality in the later stages of the disease. With vascular dementia, as a rule, the following dynamics of symptoms are noted: frequent daytime urination > nocturia > urge urinary incontinence. The symptoms do not replace, but complement each other. Changes in symptoms are less common. Such a change in the form of urination disorders may indicate the appearance of lesions in the spinal cord following lesions in the brain (for example, in multiple sclerosis (MS)). OAB syndrome can be replaced by detrusor-sphincter dyssynergia or (much less frequently) detrusor hypotension. The cerebral form of MS is replaced by the cerebrospinal form. The presence of a pathological symptom does not always indicate destruction of a certain area of the central nervous system. With demyelinating lesions of the nervous system (vascular or inflammatory origin), the areas that control urination become disconnected. Combinations of symptoms form a syndrome. Syndromes are more stable over time than symptoms, and their formation marks the appearance of persistent functional disorders. Establishing the exact form of urination disorder consists of assessing the severity and combination of symptoms on one side and the characteristics of the contractile activity of the detrusor, smooth urethral sphincter and pelvic floor muscles, identified during a comprehensive urodynamic study. Table 2 presents data on the incidence of various forms of urinary dysfunction in the most common diseases of the nervous system. Below is a description of the clinical picture of the main neurourological syndromes. Overactive bladder (old detrusor hyperreflexia) is a syndrome of predominantly neurogenic origin, including a complex of irritative symptoms (the connection with damage to certain areas of the central nervous system is indicated in parentheses): • increased frequency of urination, pollakiuria (left frontal lobe); • nocturia with frequent daytime urination (multiple brain damage); • nocturia with infrequent daytime urination (paraventricular nucleus of the hypothalamus); • nocturnal polyuria (hypothalamus, vasopressin deficiency); • the presence of an imperative urge to urinate (frontal lobe); • the presence of episodes of urge urinary incontinence (Barrington's nucleus); • the presence of episodes of urinary incontinence with increased abdominal pressure (stress urinary incontinence) (sentinel urinary center, pons); • urinary incontinence caused by the sound of falling water (reorganization of the temporal auditory cortex due to damage to the white matter of the frontal lobes). This symptom complex occurs, as a rule, in diseases of the brain and is represented by two or three symptoms. The presence of 3 or more symptoms in a patient indicates a multifocal lesion. OAB is most often found in vascular diseases of the brain, PD, and less often in MS. Detrusor-sphincter dyssynergia (DSD) is a syndrome of exclusively neurogenic origin, including a complex of irritative and obstructive symptoms (associated with damage to the lower thoracic segments of the spinal cord): • increased frequency of urination, pollakiuria; • the presence of an imperative urge to urinate; • presence of episodes of urge urinary incontinence; • feeling of incomplete emptying of the bladder at the end of urination; • repeated involuntary interruption of the urine stream during urination; • difficulty starting to urinate in the presence of an imperative urge; • a long waiting period from the moment the urge to urinate occurs until it begins. DSD is most common in MS, myelitis, spinal strokes and SCI. The combination of irritative and obstructive complaints leads to maximum discomfort and decreased quality of life. Reduced contractile activity of the detrusor (old detrusor hypotension) is a syndrome represented by obstructive symptoms (the connection with damage to certain areas of the central nervous system is indicated in parentheses): • a feeling of incomplete emptying of the bladder at the end of urination (right frontal lobe); • weak pressure of the urine stream during urination (island of Reille); • the need to strain to start and/or continue urination (island of Reille); • using the Creda maneuver (pressure with the palm over the pubis) to initiate urination (island of Reil); • a long waiting period from the moment the urge to urinate occurs until it begins (cerebellum, less often - the insula of Reil); • lack of urge to urinate (right frontal lobe); • weakening of the feeling of the urge to urinate (right frontal lobe); • a feeling of urge to urinate, as a feeling of pressure or fullness in the lower abdomen (right frontal lobe, more often with damage to the lumbar segments of the spinal cord). This form of urination disorder occurs in various diseases: ischemic cerebral stroke, spinal cord injury, spinal stroke, myelitis. A wide variety of causes causing the development of detrusor hypotension can be explained by analogy with OAB syndrome by a sensory and motor component, especially impaired sensitivity of the bladder and urethra; 8 out of 12 urination reflexes can be reproduced only if the afferent link is preserved. Pseudodyssynergia is a syndrome caused by impaired voluntary control of the pelvic floor muscles. Most often, this syndrome is observed with damage to the cerebellum and its connections with the Barrington nucleus, sometimes with damage to the Onufrovich nucleus. Clinically manifested by obstructive symptoms, such as: • difficulty starting urination in the absence of an imperative urge (cerebellum); • the need to relax the muscles of the perineum to begin urination (cerebellum); • a long waiting period from the moment the urge to urinate occurs until it begins (cerebellum). Pseudodyssynergia is most typical for PD, cerebellar infarctions and MSA. Enuresis. Modern domestic and foreign researchers understand nocturnal enuresis as the phenomenon of involuntary urination during night and daytime sleep. Enuresis is not a monosymptomatic disease, but a complex set of closely related symptoms that make up an entire syndrome. It includes: • involuntary urination during sleep; • sleep disturbance; • change in physical activity during the day; • violation of emotional-volitional behavior; • inadequate attitude towards one's defect; • therapeutic resistance; • spontaneous healing. The peculiarity of involuntary urination is that it occurs in the form of an explosion, paroxysm, accompanied by pronounced motor-vegetative manifestations, which does not occur when urinating while awake. Symptoms of disturbed behavior and changes in the emotional-volitional sphere during the daytime explain the unity of the functioning of brain systems, for example, the limbic-reticular complex, which is involved in the regulation of both sleep processes and emotional behavior during the day. According to modern concepts, enuresis is classified as minimal brain dysfunction. Under certain conditions, when sleep mechanisms “mature”, enuresis as a compensatory mechanism becomes irrelevant and spontaneously disappears. Enuresis acquires particular significance when it appears for the first time (or repeatedly) in adulthood against the background of general well-being. In this case, the patient must exclude nocturnal attacks of epilepsy (epileptic form). In addition to epilepsy, enuresis is rare in MS and Guillain–Barré syndrome, but its mechanisms in this pathology are difficult to explain. There are several other forms of enuresis that are not associated with organic damage to the nervous system: simple, neurotic, neuropathic, endocrinopathic, dysplastic, neurosis-like. At the age of 6 months. urination during daytime sleep disappears in 87% of healthy children. At the age of 1.5 years, more than 70% of children sleep dry all night or get wet occasionally in their sleep (no more than once a week). To date, a universal questionnaire has not been developed that allows at the clinical stage to establish any form of urination disorders in a neurological patient (regardless of the disease), however, questionnaires and scales already accepted in urological practice can be used. These are the Boyarsky scale-system, the Madsen-Iversen system, the American Urological Association symptom index for BPH, the international system of summary symptoms for prostate diseases I-PSS (1995), as well as the LISS scale [Lesley, 2004]. In our practice, we use the questionnaire from the Scientific Center of the Russian Academy of Medical Sciences [Shvarts P.G., 2010]. Rhythm of urination: • normal (5–8), pollakiuria up to____times, nocturia up to____times. Symptoms of sensory disturbance: • the urge to urinate is preserved; • the intensity of the urge to urinate is reduced; • there is no urge to urinate; • the urge to urinate is imperative; • the urge to urinate is accompanied by pain (from 1 to 10 points)_____ ; • the urge to urinate is felt as pressure in the lower abdomen; • the urge to urinate is felt as distension in the lower abdomen; • feeling of incomplete emptying of the bladder in the presence of residual urine; • a feeling of incomplete emptying of the bladder in the absence of residual urine. Symptoms of impaired contractile activity of the detrusor: • satisfactory stream of urine; • sluggish urine stream; • urge urinary incontinence; • the need to strain to initiate urination; • the need to strain to continue urination; • the need to strain to finish urinating. Symptoms of impaired contractile activity of the smooth urethral sphincter: • inability to urinate independently when there is a urge to urinate; • intermittent urination, usually in equal portions; • delayed onset of urination. Symptoms of impaired contractile activity of the pelvic floor muscles: • the need to relax the pelvic floor (perineum) muscles to initiate urination; • the need to tense the pelvic floor (perineum) muscles to complete urination. Behavioral symptoms: • inability to urinate in the presence of strangers (including medical staff); • restriction of drinking regime; • use of hygiene products (pads ______ pcs./day, diapers); • control urination “on the track”. Symptoms of UUI associated with the position of the patient’s body (in space): • inability to accurately get a stream of urine into the toilet (for men); • inability to urinate while lying down; • inability to urinate while standing. A distinctive feature of this questionnaire is an attempt to link the nature of the symptom with the sensory or motor sphere, as well as with the pelvic organ, the dysfunction of which caused the urination disorder. In conclusion, it should be emphasized that the further search for the optimal questionnaire or scale for assessing the SNMP in a neurological patient, in our opinion, should be aimed at indicating the localization and the mechanism of damage to the nervous system. With this approach to the detection of diseases of the central nervous system, a neurourological examination will be as close as possible to its goal.
References 1. Al-Shukri S.H., Kuzmin I.V. Detrusor overactivity and urge urinary incontinence. A manual for doctors. St. Petersburg, 1999. 48 p. 2. Benign prostatic hyperplasia / Ed. Lopatkina N.A. M., 1999. 216 p. 3. Zakhmatov Yu.M. Changes in urodynamics and their role in extra- and intravesical diseases: Abstract of thesis. dis. ...cand. honey. Sci. M., 1978. 22 p. 4. Leites A.L., Shnetser L.Ya., Ogombaev M.A. Neurogenic bladder. Frunze, 1971. 115 p. 5. Mazurenko D.A. Differential diagnosis and treatment of urination disorders in patients with Parkinson's disease: Dis. ...cand. honey. Sci. M., 2005. 105 p. 6. Minatullaev Sh.A. Chronic vascular diseases of the brain and functional disorders of urination: Abstract of thesis. dis. ...cand. honey. Sci. M., 2009. 25 p. 7. Neurogenic dysfunctions of the bladder / Ed. Javadzadeh M.D., Derzhavina V.M. M.: Medicine, 1989. 384 p. 8. Osipov I.B., Smirnova L.P. Neurogenic bladder in children. St. Petersburg: Peter, 2001. 79 p. 9. Pushkar D.Yu. Overactive bladder in women. M.: MEDpress-inform, 2003. 159 p. 10. Multiple sclerosis. Selected issues of theory and practice / Ed. Zavalishina I.A., Golovkina V.I. M., 2000. 625 p. 11. Savchenko N.E., Mokhort V.A. Neurogenic urinary disorders. Minsk: Belarus, 1970. 244 p. 12. Shvarts P.G. Disorders of urination in patients with relapsing-remitting multiple sclerosis: Abstract of thesis. dis. ...cand. honey. Sci. M., 2004. 22 p. 13. Shvarts P.G., Popov S.V. Neurogenic urinary retention. M.: Press Bureau, 2011. 224 p. 14. Shevtsov I.P. Treatment of urinary disorders and their complications in patients with spinal cord injury. L.: Medicine, 1974. 215 p. 15. Abrams PH, Blaivas JG, Stanton SL, Anderson JT Standardization of terminology of lower urinary tract function // Neurourol. Urodyn. 1988. Vol. 7. P. 403–428. 16. Araki I., Kuno S., Assessment of voiding dysfunction in Parkinson's disease by the international prostate symptom score // J. Neurol Neurosurg Psychiatry. 2000. Apr. Vol. 68(4). R. 429–33. 17. Blaivas JG Evaluation of urinary bladder symptoms in multiple sclerosis. In: Poser CM et al. eds. The Diagnosis of Multiple Sclerosis. 1984. NYP pp. 76–93. 18. Bors E., Comarr A. Neurological disturbance of sexual function with special references to 529 patients with spinal cord injury // Urol Surv. 1960. Vol. 10. P. 191–222. 19. Langhorne P. et al. Medical complication after stroke // Stroke. 2000. Vol. 31. N 6. P. 1223–1229. 20. Rushton DN Handbook of neuro-urology. 1994. Marcel Dekker. 404 p.
Causes
The main cause of bladder dysfunction in men is neurogenic factors. When a pathology is detected, diagnostics are carried out primarily based on this indicator. Pathology can be provoked by:
- Parkinson's disease;
- multiple sclerosis;
- serious disturbances in the functioning of the central nervous system;
- traumatic spinal cord injuries;
- traumatic brain injury;
- tumors in the bladder control centers.
Much less frequently, the disorder is caused by other factors, which include:
- age-related changes in the bladder;
- compression of the bladder by tumors of nearby organs;
- insufficient blood supply to the bladder or urethra;
- vascular atherosclerosis.
In order to fully treat the disease, it is mandatory to undergo an examination. After this, having identified the factor that provokes the dysfunction, therapy is carried out, aimed primarily at eliminating the cause of the pathology.
Types of NDMP
There are two main types of neurogenic bladder dysfunction:
- Hyperactive. Occurs at any time, often unexpectedly. A person cannot voluntarily control the process of natural urine excretion. It does not have the ability to accumulate in the bladder, so the urge to go to the toilet occurs very often. The main symptoms of the disorder include:
- release of a small amount of fluid from the body;
- immediate release of urine with a sudden gust;
- hypertonicity of the pelvic floor muscles, in which urine moves backwards through the ureter;
- Unusual postures in a small child (for example, squatting or crossing legs).
- Hypoactive. It is expressed in weak contraction of the muscles of the organs responsible for urination, or its absence, even with a large accumulation of fluid in the bladder. Patients lose the desire to defecate and incontinence occurs. In most cases, the person does not experience relief.
Free consultation on training issues
Our consultants are always ready to tell you about all the details!
Laboratory research
To make a diagnosis, laboratory tests are indicated. Namely, you will need to do a general urine test, which in case of illness will show bacteriuria, persistent pyuria, and albuminuria. In addition, such tests are prescribed. such as a Zimnitsky test, a general blood test, its biochemical study, a urine flora test.
To diagnose pathology, X-ray examination is used:
- plain radiography allows you to determine changes in the size of the contours of the kidneys, a significant enlargement of the bladder, the presence of spina bifida, a developmental abnormality or even the absence of the coccyx;
- urethrocystography is performed to identify false diverticula, narrowing of the urethra, displacement of the bladder to the right;
- excretory urography is used to identify kidney pathologies;
- ascending pyelography.
In addition to the above diagnostic methods, doctors may also prescribe the following procedures:
- Ultrasound of the kidneys and bladder to accurately assess changes in these organs and determine the level of residual urine;
- cystourethroscopy, which involves a thorough examination of the bladder with a cystoscope;
- MRI - necessary to assess the condition of the spinal cord and brain;
- urodynamic study - used to assess the state of a full and empty bladder;
- neurological examination to identify pathologies of the spinal cord and brain.
During the diagnostic process, the doctor will need to differentiate neurogenic bladder from bacterial cystitis, which will require additional examinations. Diseases can be differentiated according to the following criteria: with bacterial cystitis, inflammatory changes are observed in the urine (with a neurogenic bladder), urine culture is positive (negative), cystoscopic examination shows signs of inflammation (no signs of inflammation), the urodynamic picture is normal (there are seven types of disorders) , the effect of anti-inflammatory and antibacterial medications is positive (absent).