Pharmacological action of the substance tolterodine
The substance tolterodine, which is part of various drugs, is an antagonist of m-cholinergic receptors, which are localized in the salivary glands and bladder, and has anticholinergic and antispasmodic effects.
The active 5-hydroxymethyl derivative of tolterodine is highly specific for muscarinic receptors, has no effect on other receptors and, unlike salivary gland receptors, has selectivity for bladder receptors.
According to the instructions, tolterodine, which is part of antispasmodic drugs, not only reduces bladder activity, but also reduces detrusor pressure and salivation, helps to weaken and disappear urinary incontinence and increases the interval between urinations.
Tolterodine in the treatment of overactive bladder
The epidemiology, pathogenesis, clinical manifestations, methods of diagnosis and treatment of overactive bladder are considered. Using tolterodine as an example, the possibility of using anticholinergic drugs in the treatment of overactive bladder is considered. It is noted that tolterodine has comparable efficacy to other anticholinergic drugs, but causes fewer side effects due to its high organ specificity.
According to the definition of the International Continence Society, overactive bladder syndrome is understood as urgent (imperative, imperative) urination (in combination with or without urgent urinary incontinence), usually frequent (more than eight times a day) and accompanied by nocturia (urination during the period from falling asleep to waking up) [1].
Epidemiological studies have shown that overactive bladder is one of the ten most common diseases, ahead of diabetes mellitus, gastric and duodenal ulcers. In addition, every year there is a steady increase in the number of patients with overactive bladder.
The significance of this disease is determined not only by its high prevalence, but also by the sharp deterioration in the quality of life of patients. Despite the benign nature of the disease, symptoms of overactive bladder have a negative impact on the emotional and psychological state, social and work activity and, in this regard, on the economic situation of patients [2, 3].
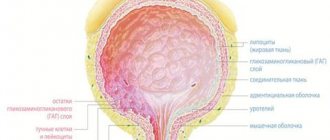
An overactive bladder is a consequence of detrusor overactivity (a violation of its adaptive ability) of a neurogenic (due to neurological diseases) or idiopathic (unknown cause of involuntary contractions) nature. Normally, when the bladder is filled, the pressure in its lumen, regardless of the volume of incoming urine, remains low (
The cause of disruption of the adaptive ability of the detrusor can be myogenic disorders in the detrusor due to age-related changes or bladder outlet obstruction, as well as various neurological diseases and injuries leading to disruption of control over the storage capacity of the bladder by the central nervous system.
In approximately 30% of cases, there is an overactive bladder without detrusor overactivity [4]. The pathogenesis of the development of urgency and frequency of urination in patients with an overactive bladder without detrusor overactivity remains unknown to date.
Overactive bladder is a diagnosis of exclusion, so diagnosing this disease involves a series of measures aimed at consistently excluding well-known urological and other diseases that can cause urgent and frequent urination. In addition to collecting anamnesis, assessing complaints and physical examination, a method such as keeping a urination diary is used. In it, the patient records the frequency of urination, urgency and episodes of urgent urinary incontinence, as well as the volume of urine excreted during each urination for 72 hours. The results of a general urine test and, in some cases, urine culture for sterility are assessed, and an ultrasound scan of the bladder is performed to detect the presence of tumors, stones and residual urine. The diagnosis of “overactive bladder” is established in the presence of urgency or urgency urinary incontinence and more than eight urinations per day, as well as the absence of lower urinary tract infection and pathological findings according to ultrasound examination.
Treatment of patients with bladder storage dysfunction is aimed primarily at restoring lost control of the detrusor storage capacity. Initial treatments for overactive bladder patients include biofeedback, behavioral therapy, and anticholinergic medications.
In most cases, drug therapy is carried out. The main group of drugs used to treat overactive bladder are anticholinergic drugs (M-anticholinergics, anticholinergics). These drugs block M-cholinergic receptors, differing in the degree of organ specificity and selectivity for different subtypes of these receptors. Blockade of postsynaptic (M2, M3) detrusor muscarinic cholinergic receptors reduces or prevents the action of acetylcholine, reducing detrusor overactivity and increasing bladder capacity. Clinically, this is manifested by a decrease in the urgency and frequency of urination.
It is necessary to understand that all anticholinergic drugs cause side effects associated with blocking M-cholinergic receptors in other organs and tissues. For example, dry mouth, a major side effect of anticholinergic drugs, is caused by blockade of muscarinic receptors in the salivary glands. Other systemic side effects of anticholinergic drugs that block muscarinic cholinergic receptors in various organs include impaired vision clarity, decreased tone of smooth muscle organs and associated inhibition of intestinal motility and constipation, tachycardia, in some cases central effects (drowsiness, dizziness), etc. The above side effects necessitate the use of anticholinergics with a good safety profile.
Oxybutynin hydrochloride has long been considered the primary anticholinergic drug for the treatment of bladder storage disorders (maximum 5–10 mg two to three times daily). In recent years, new drugs have been proposed for the treatment of patients with bladder storage disorders, such as trospium chloride (15 mg two to three times daily), tolterodine tartrate (2 mg twice daily) and solifenacin succinate (5–10 mg once a day).
Tolterodine tartrate is one of the most commonly used medications to treat overactive bladder. It must be emphasized that tolterodine tartrate was the first uroselective drug specifically developed for the treatment of urgency and frequency of urination.
Tolterodine is a mixed antagonist of M2- and M3-cholinergic receptors, which has a distinct organ specificity of action in relation to the detrusor. The affinity of tolterodine for the salivary glands is eight times lower than that of oxybutynin, which is in some way a comparator drug for other anticholinergic drugs. This explains the lower incidence of side effects with tolterodine compared with oxybutynin. Unlike oxybutynin, which has pronounced selectivity for M1 and M3 receptors, tolterodine demonstrates almost identical sensitivity to different subtypes of muscarinic receptors.
After oral administration, tolterodine is rapidly absorbed from the gastrointestinal tract. The maximum concentration in the blood serum is achieved after one to three hours. The maximum concentration increases in proportion to the dose of tolterodine in the range from 1 to 4 mg. The absolute bioavailability of tolterodine is 65% in poor metabolizers (those lacking CYP2D6) and 17% in increased metabolizers (most patients).
Food does not affect exposure to unbound tolterodine and the active 5-hydroxymethyl metabolite in advanced metabolizers, although tolterodine levels increase when the drug is taken with food. An equilibrium state is achieved after two days of continuous use.
Tolterodine is primarily metabolized in the liver by the polymorphic enzyme CYP2D6 to form a pharmacologically active 5-hydroxymethyl metabolite. In persons with reduced metabolism (CYP2D6 deficiency), tolterodine undergoes dealkylation by CYP3A isoenzymes to form an inactive metabolite. Tolterodine and the 5-hydroxymethyl metabolite bind predominantly to orosomucoid, with unbound fractions accounting for 37 and 36%, respectively.
The half-life is two to four hours. Approximately 77% of the administered dose is excreted in the urine and 17% in the feces, with less than 1% unchanged and about 4% as the active metabolite.
The safety, tolerability and clinical effect of the drug do not depend on the phenotype. The relative low lipophilicity of tolterodine limits its penetration of the blood-brain barrier and ensures low levels of associated side effects [5].
The effectiveness of tolterodine in reducing urinary frequency and episodes of urge incontinence in patients with both idiopathic and neurogenic detrusor overactivity has been confirmed by several randomized placebo-controlled studies [6, 7]. It is international clinical trials using tolterodine that are the most extensive both in terms of the number of patients and the composition of the participating countries. Tolterodine significantly improves the condition of patients, stopping the clinical manifestations of detrusor overactivity and improving urodynamic parameters.
One of the first clinical studies involved 293 patients with symptoms of overactive bladder due to urodynamically proven detrusor overactivity. Patients were divided into three groups and received tolterodine 2 mg twice daily, oxybutynin 5 mg three times daily, and placebo, respectively. After 12 weeks of treatment, urinary frequency decreased by 21% in the tolterodine group, 19.5% in the oxybutynin group, and 10.5% in the placebo group. The number of episodes of urge urinary incontinence decreased by 78, 71 and 19%, respectively. It was significant that tolterodine had a much better safety profile compared to oxybutynin [7].
R. Millard et al. studied the effectiveness of 1 and 2 mg of tolterodine in patients with idiopathic detrusor overactivity and detrusor hyperreflexia compared with placebo. After 12 weeks of treatment, the average number of urinations within 24 hours statistically significantly decreased from 11.2 to 9.0, and the number of episodes of urge urinary incontinence - from 3.6 to 1.8. Similar efficacy was obtained even with 1 mg of tolterodine. Severe dry mouth was noted in only 2.1 and 2.0% of patients receiving 2 and 1 mg of tolterodine. The authors rightly note that with the use of tolterodine, there is a clinically significant improvement in overactive bladder symptoms with a good safety profile [8].
It should be noted that tolterodine was the first to open up new possibilities in the treatment of irritative symptoms of the lower urinary tract in men with benign prostatic hyperplasia. For a long time, it was considered potentially dangerous to prescribe anticholinergic drugs to patients with bladder outlet obstruction due to benign prostatic hyperplasia due to the risk of urinary retention. At the same time, the presence of severe irritative symptoms in patients with benign prostatic hyperplasia that cannot be treated with alpha-blockers and herbal medications has allowed a number of researchers to evaluate the possibility and effectiveness of using anticholinergic drugs in this particular group of patients.
Thus, tolterodine was prescribed to men with benign prostatic hyperplasia and lower urinary tract symptoms in whom alpha-blocker monotherapy was ineffective. The results exceeded all expectations. It turned out that the combination of an alpha-blocker and tolterodine relieved both storage symptoms and bladder emptying symptoms [9]. This prompted further research. They demonstrated that the combined use of an alpha-blocker and tolterodine was significantly more effective in reducing the frequency of urge incontinence and daytime or diurnal frequency of urination in men with benign prostatic hyperplasia compared with the control group [10, 11].
In turn, the results obtained provided the basis for the use of tolterodine as monotherapy in men with predominant irritative symptoms in benign prostatic hyperplasia and the absence of bladder outlet obstruction. In two clinical studies, tolterodine resulted in statistically significant reductions in urgency urinary incontinence, frequency of urination during the day and night, and urgency-related urination compared with placebo. Subsequent analysis showed that tolterodine was more effective in men with prostate specific antigen levels less than 1.3 ng/mL, which is associated with a small prostate volume [12–14].
Thus, tolterodine is a first-line treatment for overactive bladder and has comparable efficacy to other anticholinergic drugs, but its high organ specificity provides the advantage of a lower incidence of side effects.
Side effects of tolterodine
The use of drugs that contain the substance tolterodine, according to reviews, causes side effects from various body systems, namely:
- Visual impairment, dizziness, headache, xerophthalmia, drowsiness and fatigue (nervous system and sensory organs);
- Arterial hypertension (cardiovascular system);
- Dry mouth, nausea, dyspepsia, constipation, flatulence, diarrhea and abdominal (gastrointestinal) pain;
- Urinary tract infections and dysuria (genitourinary system).
Also, drugs containing tolterodine, according to reviews, cause allergic reactions and flu-like symptoms, weight gain, sinusitis, bronchitis and dry skin.
Contraindications to the use of Tolterodine
Tolterodine and analogues are not prescribed to people who have hypersensitivity or individual intolerance to the substance, urinary retention, myasthenia gravis that cannot be treated, angle-closure glaucoma, megacolon, severe ulcerative colitis.
Due to the fact that there have been no strictly controlled and adequate studies in pregnant and breastfeeding women, Tolterodine can be taken during pregnancy only if there is a clear indication from the attending physician, and also if the potential therapeutic benefit to the mother significantly outweighs the threat to the fetus.
If it is necessary to prescribe medication during lactation, it is recommended to temporarily stop breastfeeding.
Overdose
Reviews of Tolterodine report that in case of an overdose, hallucinations, convulsions, severe agitation, respiratory failure, mydriasis, tachycardia, accommodation paresis, painful urge to urinate, and urinary retention may occur.
In the event of the development of these effects, it is necessary to perform mandatory gastric lavage. In case of urinary retention, catheterization of the bladder is recommended; in case of agitation or convulsions, benzodiazepines are taken; in case of severe respiratory failure, artificial ventilation is performed.