Glomerulonephritis is a common kidney disease. As a rule, the renal glomeruli are affected (to a lesser extent, the interstitial tissue and tubules). If the disease is chronic, the symptoms may be almost invisible or completely absent. But if the disease is acute, then this condition can lead to serious complications that can lead to disability of a person at an early age.
Glomerulonephritis refers to inflammatory diseases of the urinary system. Those, in turn, affect the functioning of not only the kidneys, but also the functioning of the heart. This is explained by the fact that the work of the cardiac and renal systems is connected, therefore, signs such as increased blood pressure or other symptoms of diseases of the cardiovascular system are often concomitant symptoms for diseases of the urinary system. Therefore, it is necessary to start treatment of glomerulonephritis on time to avoid many negative consequences.
At the same time, the success of treatment largely depends on the timeliness of contacting a doctor. It is necessary to pay attention to such signs of pathology as the appearance of edema and blood in the urine.
General information
With glomerulonephritis, damage occurs to the glomeruli - the glomeruli of the kidneys. Most often this occurs due to an infectious or inflammatory process, but other causes may also influence the appearance of pathology.
According to statistics, glomerulonephritis is one of the three most common kidney diseases occurring in adult patients. The danger is that this disease often leads to disability due to the development of chronic renal failure if treatment is not started in time.
At the same time, there is one very interesting pattern. The use of effective antibacterial treatment can reduce the proportion of acute glomerulonephritis, but the number of patients whose disease becomes chronic is steadily growing. This situation is explained by poor quality nutrition, as well as environmental degradation.
Most often, glomerulonephritis is diagnosed in adult patients under 40-50 years of age. But the disease also occurs in childhood. Moreover, men suffer from it much more often than women.
How is glomerulonephritis treated today?
Since this is a fairly serious disease, therapy is possible only in a hospital setting, especially in the phase of pronounced symptoms or in the presence of renal failure. Modern treatment of glomerulonephritis is a complex of measures, of which the most important is given to drug therapy, which, depending on the characteristics of the course of the disease, includes:
- antibacterial drugs to fight streptococci or other infections that provoke the development of inflammation of the renal glomeruli;
- antifungal medications if the disease is caused by a fungal infection;
- anti-inflammatory drugs to reduce inflammation in the kidneys;
- symptomatic medications - antihypertensives, diuretics, immunosuppressants, anticoagulants, etc.
Severe renal failure requires hemodialysis. If the kidney is seriously damaged, a transplant may be needed.
One of the powerful therapeutic factors is a special diet for glomerulonephritis, which reduces the load on the kidneys, allowing the tissues to recover. It is based on the limitation:
- table salt – no more than 3-5 grams per day;
- proteins – no more than 80 grams per day;
- carbohydrates – no more than 350 grams per day;
- fats – no more than 90 grams per day.
The main dishes are cereal soups with potatoes, cereal porridges, pasta, herbs and vegetables, low-fat dairy products, low-fat fish, meat and poultry. Pickles and smoked foods, fried foods, sausages, chocolate, legumes, and canned food are completely excluded. In the hospital, patients receive food as part of diet No. 7, but even after discharge it is recommended to adhere to food restrictions.
Main symptoms of glomerulonephritis
The acute course of the disease is characterized by 3 main groups of symptoms:
- urinary – increased red blood cells and protein in the urine;
- edematous – swelling of the arms, legs and face;
- hypertensive – an increase in blood pressure that cannot be reduced with conventional blood pressure medications.
It all starts with an increase in body temperature, a headache begins, and the general condition worsens. Swelling of the eyelids is visible, appetite decreases, and the skin turns pale.
Another telltale sign is a change in urine color caused by blood. In 85% of cases, microhematuria develops, in 15% - macrohematuria (this condition is characterized by a change in the color of urine to a very dark color).
Another symptom of glomerulonephritis in adults is facial swelling. It is very pronounced in the morning, gradually disappearing during the day.
Other symptoms include:
- gagging;
- pain in the lumbar region;
- urge to urinate;
- swelling of the limbs.
Diagnostic tests
Currently, the diagnosis of glomerulonephritis does not cause difficulties, especially in cases where the symptoms of the disease are well expressed. But even with mild symptoms, laboratory tests and hardware tests allow the doctor to establish a complete picture of the disease, especially in the presence of a previous infection. To do this, it uses the following assignments:
- general and biochemical blood tests;
- general and biochemical urine tests;
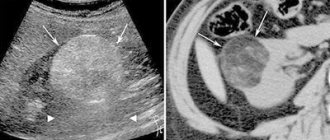
- Ultrasound of the kidneys and ultrasound examination of the renal blood vessels;
- X-ray and CT scan of the kidneys;
- nephroscintigraphy;
- excretory urography (only for patients with acute form);
- ECG;
- fundus examination;
- kidney tissue biopsy (in some cases).
The presence of glomerulonephritis is indicated by the presence of protein in the urine, hematuria, increased levels of cholesterol and nitrogenous waste in the blood, as well as critically high values of immune complexes.
After making a diagnosis, the nephrologist prescribes appropriate therapy, taking into account the characteristics of the course of the disease and the general condition of the patient.
Symptoms according to the form of the disease
Each form of glomerulonephritis has its own signs and symptoms. The acute stage occurs in different ways: some patients have severe symptoms, others have them, but are not so intense. The main features include:
- swelling;
- general weakness, feverish state;
- strong thirst;
- increased blood pressure;
- blood in urine.
This stage develops within three weeks from the moment of infection. The peculiarity of acute glomerulonephritis in children is that it often leads to recovery, while in adults, the acute form is more pronounced, becoming chronic (without proper treatment).
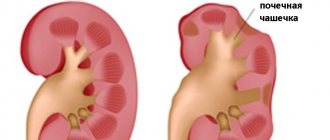
The chronic form of glomerulonephritis is characterized by the death of the renal glomeruli, which are replaced by connective tissue.
If drug therapy fails to get rid of the inflammatory process, the situation may worsen due to various complications. Moreover, if you start the course of chronic glomerulonephritis, the kidneys will become wrinkled in the later stages of this process, i.e. There is a real danger to life if therapy is not started.
In what cases does the disease develop?
Most often, streptococci or staphylococci become the impetus for the development of the inflammatory process in the renal glomeruli. Doctors consider the main causes of glomerulonephritis to be:
- acute viral infections - influenza, pneumonia, sore throat, scarlet fever;
- vaccination with “live” vaccines”;
- allergic reactions of the body;
- systemic diseases - lupus erythematosus, vasculitis.
You should not discount the accompanying unfavorable factors, first of all:
- chronic infections - caries, sinusitis, tonsillitis, viral hepatitis, etc.;
- uncontrolled use of medications;
- prolonged exposure to the sun;
- frequent consumption of salty foods;
- Presence of unhealthy habits – consumption of alcohol, drugs.
The inflammatory process occurs due to damage to the immune mechanism: antibodies form protein complexes with antigens left in the blood by the infection, and these proteins settle on the walls of the capillaries in the glomeruli. Blood circulation in the kidneys worsens, tissue cells begin to die, which is why the filtering function of the glomeruli deteriorates and the general intoxication of the body increases, which is expressed in a certain set of manifestations.
Features of treatment
Regardless of the form of glomerulonephritis, all treatment is carried out exclusively in an inpatient setting. The length of hospitalization depends on the severity of the individual case.
The treatment regimen is determined by the attending physician. Here is just one of the possible options:
- Diet No. 7.
- Bed rest.
- Antibacterial therapy (erythromycin, oxacillin + ampicillin).
- Taking prednisolone and non-hormonal drugs to correct immunity.
During treatment, various drugs are also used to eliminate associated symptoms. These are diuretics to eliminate swelling, drugs to lower blood pressure, and anti-inflammatory drugs.
Medical recommendations are standard: exclude spicy, salty foods from the diet, refrain from smoking and drinking alcohol. You need to monitor your weight, periodically loading yourself with physical exercise.
Herbs for glomerulonephritis
Herbs are powerful medicines. In an individually selected combination, herbal infusions can provide a full range of “services” necessary in the treatment of glomerulonephritis: reduce blood pressure, eliminate swelling and inflammation, restore tissue, harmonize metabolism, remove toxins and reduce their formation, etc. Can herbal infusion completely replace drug therapy? The answer to this question is very individual. In any case, only a herbalist can select it after examining the patient and familiarizing himself with the results of laboratory and instrumental studies. A herbalist can carry out his own diagnostics, for example, using the method of determining the state of various body systems using the iris of the eye (iridology).
In the treatment of patients suffering from glomerulonephritis, other holistic methods of traditional medicine can be used - classical and resonant homeopathy, osteopathy, acupuncture, qigong therapy. An individually selected diet and exercise regimen play a big role.
Are the methods of classical medicine combined with traditional ones? Yes. The “proportion” is determined by the duration and severity of the disease, the individual characteristics of the body and the course of the disease, and the choice of the person himself.
Make an appointment
Possible complications
As a rule, complications are caused by chronic glomerulonephritis. The consequences can be quite serious:
- Kidney failure.
- Serious heart problems.
- Uremic coma.
- Nephritic encephalopathy.
Glomerulonephritis is a disease that often leads to early disability. It is important to begin conservative treatment when the first signs of the disease are detected.
At the end of therapy, sanatorium treatment is recommended. You need to be regularly monitored by a specialist.
Classification (forms)
In recent years, the classification of chronic glomerulonephritis has been changed. Previously, the disease was divided into types (species) based on symptoms. Today, classifications are based on pathomorphological changes, which are identified by examining a kidney biopsy.
In the CIS countries, the clinical classification , authored by E.M., Tareev. According to this division, there are the following forms of chronic glomerulonephritis:
- Hematuric
- Latent
- Nephrotic
- Hypertensive
- Mixed
According to the classification of Serov V.V. and other authors, based on pathomorphological characteristics the following forms of the disease can be distinguished:
- With half moons
- Diffuse proliferative
- Membranoproliferative
- Mesangioproliferative
- Minimal change nephropathy
- Membranous nephropathy
- Fibroplastic
- Fibrillar-immunotactoid
- Focal segmental glomerulosclerosis
Doctors believe that each of these forms can be acute or chronic.
Prevention
Glomerulonephritis can be prevented by following several effective preventive measures. Here are the main ones:
- Engage in an active hobby (especially if your job involves sitting for long periods of time).
- Stop or significantly limit alcohol consumption and smoking.
- Minimize the consumption of salty foods.
- Avoid hypothermia.
- Constant control of blood sugar (diabetes).
Glomerulonephritis is a progressive disease, the course of which can be stopped if the cause of the pathology is determined in time. Moreover, the overall picture is very favorable: most cases end in complete recovery (in about 30% of cases the disease progresses to the chronic stage).
Diagnosis of chronic glomerulonephritis
For diagnosis, it is important to identify the leading syndrome: nephrotic, acute nephrotic, isolated urinary, arterial hypertension. Symptoms of chronic renal failure are also important.
Nephrotic syndrome most often occurs with:
- membranous glomerulonephritis
- glomerulonephritis with minimal changes
- kidney amyloidosis
- diabetic glomerulosclerosis, renal amyloidosis
Acute nephritic syndrome is a combination of hematuria, hypertension, edema and often deterioration of the filtration function of the kidneys. It can occur with the following diseases:
- mesangiocapillary glomerulonephritis
- rapidly progressive glomerulonephritis
- exacerbation of lupus nephritis
- mesangioproliferative glomerulonephritis
Arterial hypertension in combination with proteinuria and minimal changes in urinary sediment occurs, in addition to chronic glomerulonephritis, with diabetic nephropathy, kidney damage as part of hypertension.
Urinary syndrome is a combination of proteinuria, hematuria, cylindruria, leukocyturia with lymphocyturia (any combination of the above).
There are the following causes of isolated hematuria :
- infection
- stone
- tumor in the urinary tract
- Berger's disease
- Allport's disease
Proteinuria occurs with inflammatory and non-inflammatory lesions of the glomeruli or with tubulointerstitial lesions of various etiologies. A special variant of massive proteinuria is overflow proteinuria, which is associated with the presence of paraprotein in the blood and myeloma. Benign proteinuria occurs with obstructive sleep apnea syndrome, heart failure; sometimes occurs during emotional stress, hypothermia, or becomes a consequence of a febrile reaction. It is called benign because the prognosis for kidney function is favorable.
Kidney biopsy
A puncture biopsy of the kidney is performed to determine the morphological form of chronic glomerulonephritis, which affects the choice of treatment tactics. Contraindications :
- Hypocoagulation
- The presence of not two, but one functioning kidney
- Suspicion of renal vein thrombosis
- Suspicion of malignancy
- Increased venous pressure in the systemic circulation
- Polycystic kidney disease
- Hydro- and pyonephrosis
- Impaired consciousness
- Renal artery aneurysm
Differential diagnosis
Differential diagnosis is carried out with the following diseases:
- acute glomerulonephritis
- chronic pyelonephritis
- chronic tubulointerstitial nephritis
- nephropathy in pregnancy
- amyloidosis
- alcoholic kidney damage
- kidney damage in systemic connective tissue diseases
- diabetic nephropathy
Characteristic features of chronic pyelonephritis that need to be taken into account when diagnosing:
- neutrophiluria
- bacteriuria
- exacerbations with fever and chills
- changes in the collecting system
- asymmetry of the lesion
In acute glomerulonephritis, a history of connection with a previous streptococcal infection is considered, but, however, unlike IgA nephropathy, the time interval is 10-14 days. Typically acute onset. Among the patients are mainly teenagers and children.
Chronic tubulointerstitial nephritis has the following features (taken into account in differential diagnosis):
- slight proteinuria
- polyuria
- urine acidification disorder
- decreased relative density of urine
If amyloidosis is suspected, an underlying pathology should be looked for, namely chronic inflammation, which occurs, for example, with rheumatoid arthritis. Amyloidosis is suspected when chronic renal failure persists with enlarged or normal kidney size and in the presence of nephrotic syndrome. Tissue biopsy is of decisive importance in the differential diagnosis of such cases.
The diagnosis of diabetic nephropathy is likely (as well as chronic pyelonephritis) if a person has diabetes mellitus or its complications, slowly increasing chronic renal failure, scanty changes in urinary sediment, normal or slightly enlarged kidney sizes.
Nephropathy in pregnant women is said to occur if symptoms of kidney damage appear in the second half of the gestational period, accompanied by high hypertension and other signs of preeclampsia and eclampsia.
Bibliography
- Clinical recommendations “Diagnostics and treatment of acute post-streptococcal glomerulonephritis”. Developer: Scientific Society of Nephrologists of Russia, Association of Nephrologists of Russia. Moscow, December 18, 2014
- O. V. Tirikova, I. A. Filatova. Glomerulonephritis. Textbook of Irkutsk State Medical University (2017)
- A. V. Malkoch, A. Yu. Nikolaev, N. N. Filatova. Acute post-streptococcal (post-infectious) glomerulonephritis. 2021, no. 1.
- A. L. Kalinin. Symptomatology and diagnosis of acute and chronic glomerulonephritis and pyelonephritis. Gomel State Medical University, 2021
- Glomerulonephoritis. .
Author:
Baktyshev Alexey Ilyich, General Practitioner (family doctor), Ultrasound Doctor, Chief Physician
Acute post-streptococcal (post-infectious) glomerulonephritis
Acute immune complex diffuse proliferative glomerulonephritis, often associated with infectious diseases, is called acute post-infectious glomerulonephritis. The leading role in the development of acute glomerulonephritis belongs to streptococcus, which determines another name for this disease - acute post-streptococcal glomerulonephritis. This most studied and common form of acute glomerulonephritis, most often affecting children, is the topic of this review.
Etiology and epidemiology of acute glomerulonephritis
Acute post-streptococcal glomerulonephritis develops as a result of a previous or persistent streptococcal infection and has typical serological and morphological signs. Its causative agent is most often β-hemolytic streptococcus of group A, the most famous nephritogenic strains of which include M-types 1, 2, 4, 12, 18, 49, 55, 57 and 60 [1–3].
The focus of streptococcal infection in the lymphoid tissues of the oropharynx (palatine and pharyngeal tonsils) is typical; the primary localization of streptococcus in the skin with impetigo or erysipelas is not uncommon; the disease may develop after otitis media or osteomyelitis. The risk of developing acute post-streptococcal glomerulonephritis after infection with streptococcus depends both on the specific strain of streptococcus and on the location of the outbreak. Thus, when infected with streptococcus serotype 49, the risk of developing glomerulonephritis with a skin infection is 5 times higher than with pharyngitis [4, 5].
In developed countries of North America and Central Europe, there has been a decrease in the incidence of acute post-streptococcal glomerulonephritis, where the disease occurs mainly in the form of sporadic cases. In developing countries in South America, Africa, China and Southeast Asia, cases of cluster diseases are observed in poor areas and epidemic outbreaks in densely populated areas. The cause of epidemics of streptococcal infections leading to outbreaks of acute glomerulonephritis are increasingly atypical (mutant) strains of group A β-hemolytic streptococcus, resistant to penicillins, macrolides and tetracyclines, as well as other streptococci (the causative agent of cow mastitis Streptococcus zooepidemicus and the nephritogenic strain of streptococcus pyogenes - Streptococcus pyogenes M49), capable of “escaping” the immune response. Acute glomerulonephritis resulting from infection with similar strains, as a rule, is more severe and has a high percentage of chronicity [6, 7]. One of the most famous was the epidemic of acute glomerulonephritis associated with infection with Streptococcus zooepidermicus, noted from December 1997 to July 1998 in the state of Nova Serrana in Brazil, when the total number of cases was 253 people (from 4.5 to 18.1 per year). 1000 population), and the source of infection was cheese made from cow's milk [6].
Acute post-streptococcal glomerulonephritis is much more common in children than in adults. The peak incidence occurs between 2 and 6 years of age. About 5% of cases occur in children under 2 years of age, and up to 10% in adults over 40–50 years of age, mostly men. Boys get sick more often than girls [1, 2, 8]. Acute post-streptococcal glomerulonephritis often develops in the winter months 10–12 days after a streptococcal infection (pharyngitis, tonsillitis, scarlet fever), or acute respiratory tract infection.
The development of acute post-streptococcal glomerulonephritis is more likely in the presence of predisposing factors, such as a family history of infectious and allergic diseases, increased family susceptibility to streptococcal infection, the presence of chronic foci of infection in the child, hypovitaminosis, and helminthiasis [3, 8]. Provoking factors for the development of acute post-streptococcal glomerulonephritis in children who are carriers of hemolytic streptococcus can be hypothermia and respiratory viral infections.
In addition to streptococcus, acute glomerulonephritis can develop as a result of other infections (bacterial, viral, parasitic). Among the viruses, the most important are influenza, measles, rubella, hepatitis A and B viruses. Thus, acute glomerulonephritis is recorded during epidemics of influenza and hepatitis A. In African and Asian countries, the cause of acute glomerulonephritis will often be parasitic infections (tropical malaria, schistosomiasis) [ 1, 3, 8].
Non-infectious factors can also provoke the development of acute glomerulonephritis, which is associated with high allergenicity of the population. Such sensitizing agents include primarily drugs (antibiotics, sulfonamides), vaccines and serums, pollen, poisons of insects and other animals, food products with individual intolerance and other allergens (Table 1).
Pathogenesis and pathomorphology
In the development of acute post-streptococcal glomerulonephritis, the formation of soluble immune complexes in the blood plays a leading role. In acute post-streptococcal glomerulonephritis or other post-infectious nephritis, there is no direct damage to the kidneys by an infectious agent, and the disease is caused by an immunopathological reaction to the pathogen and its antigens. That is why, in the “classical” course of acute post-streptococcal glomerulonephritis, the first signs of the disease appear 1–3 weeks after a sore throat, during which the body is sensitized to streptococcal antigens.
The “nephritogenicity” of certain strains of streptococcus is of great importance in the development of acute post-streptococcal glomerulonephritis. Nephritogenic strains of streptococci produce proteins - endostreptolysins, which have a pronounced affinity for the structures of the renal glomeruli. When these proteins enter the circulation, binding to areas of the glomeruli, they activate complement and form immune complexes, which leads to damage to the endothelium of the glomerular capillaries with the development of exudative and proliferative processes, provokes activation of the hemostatic system and the development of local intravascular coagulation with microthrombosis of the glomerular capillaries.
Another mechanism is realized by streptococcal neuraminidase damaging normal IgG molecules, which, deposited in intact glomeruli and binding to anti-IgG antigens, form immune complexes that damage the kidney [1, 3, 8].
The role of other antigens and toxins of β-hemolytic streptococcus, such as M-type membrane antigens, endotoxin D, nephritis-associated plasmin receptor, erythrogenic exotoxin B, is reduced to triggering proliferation mechanisms in the renal glomeruli, activation of the C3 fraction of complement and renin-angiotensin- aldosterone system (RAAS), which in turn leads to sodium and water retention and renal vasoconstriction [1, 2, 9–12].
Acute post-streptococcal glomerulonephritis is characterized predominantly by subepithelial deposition of immune complexes with the formation of diffuse endocapillary proliferative glomerulonephritis, which in its development can go through several stages: exudative, exudative-proliferative, proliferative and a phase of residual phenomena that replace each other.
Immunohistochemical examination reveals IgG and C3 in the early stages of the disease, which are distributed diffusely along the walls of the capillaries in the form of small granules.
A pathognomonic sign of acute post-streptococcal glomerulonephritis, detected by electron microscopy, will be deposits of IgG and C3 deposits in the form of “humps” on the epithelial side of the basement membrane of the capillaries.
Initially, the changes are exudative in nature with swelling of endothelial and mesangial cells and infiltration of polymorphonuclear leukocytes, the severity of which depends on the degree of immune complex deposits. Subsequently, the processes of proliferation of mesangiocytes and endothelial cells begin to predominate, while the number of infiltrating cells gradually decreases. Morphological changes after acute glomerulonephritis can persist in the form of an increase in the mesangial matrix, uneven density and irregular contour of the glomerular basement membrane, and synechiae.
Damage to the glomerular capillaries at the onset of acute glomerulonephritis leads to their congestion, stasis, increased permeability and damage to the walls. Red blood cells penetrate into the cavity of the glomerular capsule and tubules, which causes the development of hematuria of varying severity. With significant disruption of microcirculation, the glomerular filtration rate (GFR) can significantly decrease, which will be clinically manifested as oliguria.
Impaired renal hemodynamics and renal ischemia lead to activation of the RAAS with reabsorption of sodium in the nephron tubules. This is also facilitated by activation of tubuloglomerular feedback and impaired GFR. These pathogenetic mechanisms lead to hypernatremia, acute hypervolemia and volume-sodium-dependent hypertension with volume overload of the left ventricular myocardium.
In rare cases, pronounced proliferation of the parietal epithelium and extracapillary accumulation of monocytes develop. Extracapillary proliferation (proliferative extracapillary crescents) in more than 30% of glomeruli leads to rapidly progressive acute nephritis with a rapid outcome in nephrosclerosis with terminal uremia.
Renal acute renal failure (ARF) complicates other rare variants of severe acute glomerulonephritis:
- with fibrinoid necrosis of the renal arteries with uncontrolled hypertension;
- with myorenal syndrome with rhabdomyolysis with recurrent renal eclampsia.
Clinical picture and course of the disease
Acute post-streptococcal glomerulonephritis usually manifests itself 1–3 weeks after a sore throat or pharyngitis or 3–6 weeks after a skin infection. Clinical manifestations of acute glomerulonephritis can vary from scant changes in urine to a clear manifestation in the form of acute nephritic syndrome with the classic triad of symptoms: hematuria, edema, hypertension, and oliguria (Table 2). With targeted questioning, symptoms such as thirst, weakness, and decreased urine output can be identified. As the disease progresses, shortness of breath, palpitations, headache, and nausea occur, largely due to acute hypertension. Low back pain is felt by 5–10% of patients. The pain is dull, symmetrical, caused by stretching of the renal capsule as a result of edema of the renal parenchyma.
Hematuria is a mandatory sign of acute glomerulonephritis. Microhematuria is found in 2/3 of patients, and macrohematuria in the rest. After increasing urine output, gross hematuria usually disappears, while microhematuria may persist for many months after the acute period. Edema, due to sodium and water retention during the clinical course, is detected in 80–90% of patients. The primary location of edema is the face. Swelling is most pronounced in the morning and may subside during the day, giving way to swelling of the ankles. In some patients, facies nephritica develops: swelling of the face, pallor of the skin, swelling of the neck veins. Oliguria develops in the first days of the disease and usually persists for 2–3 days. Anuria is not typical. Long-term oliguria may be considered an unfavorable prognostic sign.
Arterial hypertension develops in more than 80% of patients, most often moderate. Its pathogenesis is based on an increase in the volume of circulating blood, an increase in the stroke volume of the heart, an increase in cardiac output and peripheral vascular resistance. A prolonged and persistent increase in blood pressure (BP) is considered an unfavorable prognostic sign and may indicate the development of congestive heart failure or the formation of renal eclampsia.
Proteinuria, which is almost always observed, as a rule, does not reach high numbers and persists on average for no more than 7–10 days. Moderate and trace proteinuria may take longer to detect.
A general urine test reveals casts (hyaline, granular and erythrocyte casts); in the first days of the disease, leukocytes can be detected, represented mainly by segmented neutrophils, eosinophils and lymphocytes, reflecting the immune inflammatory process in the glomeruli.
A general blood test reveals neutrophilic leukocytosis, possible eosinophilia, increased erythrocyte sedimentation rate (ESR), and anemia. There is a moderate decrease in GFR with normal or increased renal blood flow. The nitrogen excretion function of the kidneys is often not impaired or there is a slight increase in the content of nitrogenous products. Dysproteinemia (hyper-α-2- and hyper-γ-globulinemia), hypocomplementemia are characteristic.
Serological blood tests reveal elevated titers of antistreptolysin O, antistreptohyaluronidase, and antistreptokinase in most patients. In the first week of the disease, circulating immune complexes and a decrease in the concentration of the C3 fraction of complement are detected. In the blood serum, the concentration of IgG, IgM, and rarely IgA increases.
Disturbances in the blood coagulation system are manifested by a reduction in prothrombin time, an increase in the prothrombin index, inhibition of fibrinolytic activity, and the appearance of fibrin and fibrinogen degradation products in the blood serum and urine.
Acutely developed hypervolemia leads to hypertension with expansion of the cavities of the heart. At the same time, the boundaries of relative dullness of the heart expand, tachycardia is often detected, less often - bradycardia, weakening of the first sound, emphasis of the second sound on the aorta. In severe cases, a gallop rhythm may appear. The electrocardiogram shows low voltage, prolongation of the P–Q wave, biphasicity and flattening of the T wave, and sometimes a shift in the ST interval. A spasm of the fundus vessels appears, hemorrhages and swelling of the optic nerve head are possible.
During the period of reverse development of acute nephritis, polyuria appears, edema and gross hematuria disappear, and blood pressure normalizes. After about 1.5–2 months, urine parameters normalize and complete clinical and laboratory remission occurs. However, complete recovery with reverse development of morphological changes in the kidneys occurs after 1–2 years.
If individual clinical symptoms persist for more than 6 months, this indicates a protracted course of acute glomerulonephritis; The duration of symptoms for more than 1 year is regarded as a transition to chronic nephritis. However, in children, isolated microhematuria can persist for more than 1 year after acute glomerulonephritis without chronicity of the disease [3, 8].
A distinctive feature of the course of modern acute glomerulonephritis is the predominance of low-symptomatic variants, which occur tens of times more often than manifest ones. This atypical subclinical course of acute glomerulonephritis is characterized by isolated urinary syndrome (in the form of hematuria) and the absence of extrarenal manifestations, or they are so minor and short-lived that they go unnoticed. “Classical” acute nephritic syndrome is rare.
As a rule, subclinical forms of acute glomerulonephritis are detected accidentally during a laboratory test or are discovered after the fact with a careful examination of the anamnesis.
Complications of acute glomerulonephritis
In severe cases of acute nephritis, life-threatening complications are possible in the initial period:
- renal eclampsia with cerebral edema;
- acute heart failure;
- pulmonary edema;
- acute renal failure.
The most severe complication is eclampsia (angiospastic encephalopathy), which is always accompanied by an increase in blood pressure and is caused by spasm of cerebral vessels and subsequent edema. Eclampsia is manifested by tonic-clonic convulsions that occur after a short period of precursors - headache, nausea, vomiting, visual impairment. During a seizure, there is no consciousness, the skin and mucous membranes become cyanotic, breathing becomes uneven, wheezing, foam appears at the mouth, and involuntary urination occurs. The attack lasts several minutes, sometimes a series of attacks is observed. In the absence of urgent adequate therapy, death from hemorrhage in the brain is possible.
A typical cause of acute renal failure is radiopaque nephropathy. The risk of this complication when performing intravenous urography or angiography in acute nephritis is sharply increased. In acute nephritis, the risk of iatrogenic nephropathies is high - with the use of NSAIDs, nephrotoxic antibiotics, and cyclosporine. In the presence of profuse macrohematuria causing ureteral obstruction, cases of the development of postrenal acute renal failure have been described.
Acute cardiovascular failure in children occurs rarely and is characterized by a sharp increase in liver size, an increase in peripheral edema and a clinical picture of acute left ventricular failure, progressing to cardiogenic pulmonary edema.
Diagnosis and differential diagnosis
Edema, hematuria and arterial hypertension constitute a triad of clinical symptoms that serve as the main criterion for the clinical diagnosis of acute glomerulonephritis. Difficulties in recognizing the disease arise with an atypical or erased course, when only microhematuria and slight proteinuria are detected in the child. In these cases, the diagnosis is helped by data on a recent streptococcal infection, monitoring the dynamics of blood pressure and the renal process, and the results of additional studies, including determination of the titer of antistreptococcal antibodies and the concentration of complement components in the blood serum.
Differential diagnosis should be carried out with urological diseases with hematuria (urolithiasis, nephroptosis, kidney tumors and tuberculosis, renal vein thrombosis), exacerbation of chronic glomerulonephritis, acute pyelonephritis, acute tubulointerstitial nephritis (infectious, drug-induced), IgA nephritis (primary and secondary), Alport syndrome, thin basement membrane disease, hemolytic-uremic syndrome [1, 3, 8].
To carry out a differential diagnosis, it is important to carefully collect anamnesis, find out whether there has been any previous swelling, changes in urine tests, or high blood pressure. An exacerbation of chronic nephritis is also supported by a decrease in the concentrating ability of the kidneys and changes in the fundus.
Sometimes the issue of differential diagnosis is resolved by long-term observation of the child, and in some cases, with long-lasting symptoms, a morphological examination is necessary - a kidney biopsy. The development of nephrotic syndrome or a rapidly progressive course requires the exclusion of another form of glomerulonephritis, which manifested itself under the guise of “acute” [13–15].
Treatment
Treatment of patients with acute glomerulonephritis is carried out in a hospital. In the acute period, bed rest, rest, and warmth are necessary to improve blood circulation in the kidneys. The regimen is expanded as edema disappears and hypertension is corrected.
Considering the connection of acute post-streptococcal glomerulonephritis with streptococcal infection, at the onset of the disease it is advisable to prescribe antibiotics from the penicillin group (for example, protected penicillins), cephalosporins for 10 days. Antibacterial therapy is indicated for the development of acute glomerulonephritis with pharyngitis, tonsillitis, skin lesions, especially with positive results of throat cultures or with high titers of antistreptococcal antibodies in the blood.
Diet
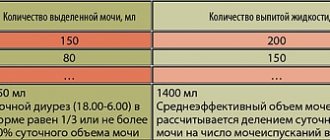
During the acute period of the disease, especially with a rapid onset with edema, oliguria and arterial hypertension, it is necessary to sharply limit the consumption of sodium chloride and water. During the development of oliguria, the daily amount of fluid consumed is calculated by the formula: diuresis for the previous day + losses due to perspiration (15 ml/(kg × day) or 400 ml/(m2 × day)). Subsequently, the amount of fluid consumed increases according to the increase in diuresis. A salt-free diet is prescribed in the first week of the disease, and if oliguria and/or arterial hypertension persists, for a longer period. Reducing elevated blood sodium concentrations is the basis of pathogenetic therapy for nephritic edema and arterial hypertension. In most patients with nephritic syndrome, a decrease in blood sodium concentration, even in the absence of other therapy, leads to rapid relief of edema and hypertension syndromes.
After stable normalization of blood pressure and diuresis, it is allowed to add salt to food at the rate of 0.5–1.0 g/day. If the course of the disease is favorable, salt intake is restored from 4–5 weeks at the rate of 50 mg/(kg × day).
Convincing evidence of the positive effect of a low-protein diet on the course of acute glomerulonephritis has not been obtained. Traditionally, it is customary to limit protein intake to about 1.0 g/kg per day. The diet is expanded mainly through vegetable protein; the consumption of animal proteins is limited for 2–3 weeks. Spicy dishes and products containing extractives and allergens are contraindicated; Foods rich in potassium should be avoided. The total energy value of food should meet the child's needs.
Treatment of edematous syndrome
Diuretic therapy is prescribed for severe edema, helping to reduce hypervolemia and the threat of complications. Hydrochlorothiazide is effective only when GFR is normal. Spironolactone is not used due to the risk of hyperkalemia. The most commonly prescribed drug is furosemide, which is effective even in patients with reduced GFR. The drug is used in a dose of 1.0–2.0 mg/kg per day parenterally in 1–2 doses; if necessary, the dose of the drug can be increased. After a few days, the patient can be transferred to oral administration of the drug. For severe edema, signs of left ventricular failure with arterial hypertension, furosemide is prescribed at a dose of up to 4 mg/kg per day or more.
Antihypertensive therapy
Antihypertensive therapy is necessary for hypertension that is not corrected by the regimen and saluretics. For treatment, calcium antagonists of the dihydropyridine series are used: nifedipine (0.25–1 mg/kg per day), amlodipine (6–17 years: 2.5–5 mg/day), isradipine, 0.15–0.8 mg/day kg per day (up to 20 mg/day), etc.; central sympatholytics: methyldopa (10 mg/kg per day), moxonidine; cardioselective β-blockers. Angiotensin-converting enzyme inhibitors - enalapril (0.1–0.5 mg/kg per day), captopril (0.3–1.5 mg/kg per day), lisinopril (0.07–0.6 mg/kg per day) ramipril, fosinopril - used under control of the level of GFR and blood potassium in combination with furosemide.
When precursors of renal eclampsia or pulmonary edema appear, a transition to intensive infusion therapy with furosemide (up to 480 mg per day) with peripheral vasodilators (intravenous drip: nitroglycerin or sodium nitropruside, diazoxide) and alpha blockers (dihydrolazine) is necessary. If there is no effect with an increase in hypertension with encephalopathy, transfer to the intensive care unit with sessions of isolated ultrafiltration, hemodialysis or intermittent hemofiltration is indicated. Extracorporeal fluid removal is also indicated in the development of critical overhydration with the threat of acute left ventricular failure.
Immunosuppressive therapy
Immunosuppressive therapy is indicated for patients with associated nephrotic syndrome (lasting more than 2 weeks), with a decrease in GFR without a tendency to return to normal. To select an immunosuppression regimen, a kidney biopsy is required. For nephrotic syndrome with extracapillary proliferation in individual glomeruli, prednisolone is used orally at a dose of 1–2 mg/kg per day. In case of rapidly progressing acute nephritis with the detection of extracapillary proliferative crescents in more than 30% of the glomeruli of the renal biopsy, intravenous methylprednisolone “pulses” are used.
The basic principles of treatment of acute post-streptococcal glomerulonephritis are presented in table. 3.
Prevention and prognosis
To prevent acute glomerulonephritis, timely diagnosis and adequate treatment of streptococcal diseases, sanitation of foci of chronic infection, and rational implementation of preventive vaccinations are necessary. In the presence of chronic tonsillitis and/or adenoiditis, it is necessary to consult an otolaryngologist and decide on the need for tonsillectomy or adenectomy [8].
Dispensary observation of children who have suffered acute post-streptococcal glomerulonephritis is carried out for 5 years, and if the slightest changes in urine tests persist - until transfer to the adult network.
The prognosis for acute post-streptococcal glomerulonephritis in children is quite favorable. On average, about 90% of children recover; in the rest, residual changes in the urine can persist for a long time [3, 8]. The progression of acute glomerulonephritis to end-stage chronic renal failure in children is observed in no more than 1–2% of cases. Deaths are recorded extremely rarely. In a child who continues to have hypertension or edema or proteinuria above 1 g/day within 1 year after the onset of acute glomerulonephritis, chronicity should be excluded through inpatient examination.
In adults, the risk of chronic acute glomerulonephritis resulting in end-stage chronic renal failure is almost 10 times more common than in children [2–4, 8].
Currently, there is insufficient data on the possibility of transformation of acute glomerulonephritis into chronic nephritis. Since a kidney biopsy is performed only in cases of prolonged acute glomerulonephritis or the development of nephrotic syndrome, in most cases it is impossible to judge the evolution of morphological changes in the glomeruli.
Cases of chronic acute glomerulonephritis are recorded during infection with atypical strains of β-hemolytic streptococcus or its other species, as well as with the development of acute glomerulonephritis due to parasitic infections (for example, tropical malaria). These observations concern mainly adult men who have suffered acute glomerulonephritis as a result of epidemic outbreaks. [16, 17].
Literature
- Nephrology. Textbook for postgraduate education, ed. E. M. Shilova. M.: GEOTAR-Media, 2007.
- Acute glomerulonephritis - are all the issues resolved? From the editor // Clinical nephrology. 2009. T. 2. P. 4–9.
- Khasabov N. N., Malkoch A. V. Modern ideas about glomerulonephritis. In the book: Nephrology of childhood (edited by V. A. Tabolin and others). M.: ID Medpraktika-M, 2005. pp. 306–390.
- Jankauskiene A., Pundziene B., Vitkevic R. Postinfectious glomerulonephritis in children in Lithuania during 1995–2004: prevalence and clinical features //Medicina (Kaunas). 2007. Vol. 43. Suppl 1. P. 16–22.
- Nasr SH, Markowitz GS, Stokes MB et al. Acute postinfectious glomerulonephritis in the modern era: experience with 86 adults and review of the literature // Medicine (Baltimore). 2008. Vol. 87. No. 1. P. 21–32.
- Balter S., Benin A., Pinto SW et al. Epidemic nephritis in Nova Serrana, Brazil // Lancet. 2000. Vol. 355. No. 9217. P. 1776–1780.
- Francis AJ, Nimmo GR, Efstratiou A. et al. Investigation of milk-borne Streptococcus zooepidemicus infection associated with glomerulonephritis in Australia // J. Infect. 1993. Vol. 27. No. 3. P. 317–23.
- Papayan A.V., Savenkova N.D. Clinical nephrology. St. Petersburg: Sotis, 1997. 712 p.
- Yoshizawa N., Oshima S., Sagel I. et al. Role of a streptococcal antigen in the pathogenesis of acute poststreptococcal glomerulonephritis. Characterization of the antigen and a proposed mechanism for the disease // J. Immunol. 1992. Vol. 148. No. 10. P. 3110–3116.
- Viera N., Pedreanez A., Rincon J., Mosquera J. Streptococcal exotoxin B increases interleukin-6, tumor necrosis factor alpha, interleukin-8 and transforming growth factor beta-1 in leukocytes // Pediatr. Nephrol. 2007. Vol. 22. No. 9. P. 1273–1281.
- Viera N., Pedreanez A., Rincon J., Mosquera J. Streptococcal zymogen type B induces angiotensin II in mesangial cells and leukocytes //Pediatr. Nephrol. 2009. Vol. 24. No. 5. P. 1005–1011.
- Gadau J., Peters H., Kastner C. et al. Mechanisms of tubular volume retention in immune-mediated glomerulonephritis // Kidney Int. 2009. Vol. 75. No. 7. P. 699–710.
- Wong W., Morris MC, Zwi J. Outcome of severe acute post-streptococcal glomerulonephritis in New Zealand children // Pediatr. Nephrol. 2009. Vol. 24. No. 5. P. 1021–1026.
- Raff A., Hebert T., Pullman J., Coco M. Crescentic post-streptococcal glomerulonephritis with nephrotic syndrome in the adult: is aggressive therapy warranted? // Clin. Nephrol. 2005. Vol. 63. No. 5. P. 375–380.
- El-Husseini AA, Sheashaa HA, Sabry AA et al. Acute postinfectious crescentic glomerulonephritis: clinicopathologic presentation and risk factors // Int. Urol. Nephrol. 2005. Vol. 37. No. 3. P. 603–609.
- Pinto SW, Sesso R., Vasconcelos E. et al. Follow-up of patients with epidemic poststreptococcal glomerulonephritis // Am. J. Kidney Dis. 2001. Vol. 38. No. 2. P. 249–255.
- Sesso R., Pinto SW Five-year follow-up of patients with epidemic glomerulonephritis due to Streptococcus zooepidemicus // Nephrol. Dial Transplant. 2005. Vol. 20. No. 9. P. 1808–1812.
A. V. Malkoch1, Candidate of Medical Sciences A. Yu. Nikolaev, Doctor of Medical Sciences, Professor N. N. Filatova, Candidate of Medical Sciences
Federal State Budgetary Educational Institution of Further Professional Education RMANPO Ministry of Health of the Russian Federation, Moscow
1 Contact information