Acute pyelonephritis is a nonspecific inflammatory disease of the kidneys. Bacterial attack plays a direct role in the occurrence of the disease. Penetration of bacterial agents into the kidneys occurs through the bloodstream or from the urinary tract.
The inflammatory process affects the pyelocaliceal system and interstitial renal tissues. Acute pyelonephritis most often affects women and small children. This is explained by anatomical features and physiology.
What are the stages of the disease?
The clinical course of acute pyelonephritis has several stages. Each of them develops in accordance with the pathomorphological changes occurring in the kidneys.
At the initial stage of pathological development, serous inflammation occurs. This stage is characterized by a slight increase in kidney tension and perivascular infiltration. If a specialist is contacted in a timely manner, the patient is prescribed conservative therapy, with the help of which the inflammatory process is replicated. The patient makes a full recovery. If there is no treatment at the initial stage, the disease will progress, and purulent-destructive kidney damage will subsequently occur.
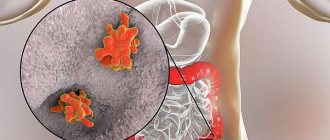
The next stage is called apostematous pyelonephritis. This is an inflammatory disease when pustular formations are formed, localized in the renal cortex. If there is no adequate therapy, such pustules will merge and form a large purulent focus. It is called a kidney carbuncle. When this condition develops, the risk of kidney abscess formation increases. Purulent contents can spill into the perinephric tissue. If treatment is started in a timely manner, the infiltration lesion heals, scars are formed, which consist of connective tissues.
Pathomorphology
The following morphological forms of acute pyelonephritis are distinguished:
- purulent
- serous
- purulent with mesenchymal reaction
In chronic pyelonephritis, the inflammatory process is focal and polymorphic. Histological changes can be different; a common morphological sign is lymphohistiocytic infiltration. The same changes can occur with endemic Balkan nephropathy, chronic tubulointerstitial nephritis while taking analgesic drugs, and primary changes in the vessels of the kidneys. Chronic pyelonephritis differs from other kidney diseases by the simultaneous involvement of the pyelocaliceal system of the organ. Changes in the kidneys as the process progresses are characterized as focal, uneven and asymmetrical.
What are risk factors?
There are a number of extrasexual factors that increase the risk of developing acute pyelonephritis:
- Congenital or acquired anomaly, pathology of the structure of the kidneys and other organs of the urinary system.
- AIDS virus.
- Urolithiasis disease.
- Diabetes. With increased sugar content in the urine, pathogenic microorganisms will multiply.
- Age.
- The spinal cord and peritoneal organs are injured.
- Surgery or other medical intervention on the urinary system.
- Bacterial chronic disease, the presence of an infectious focus in the body.
The occurrence of acute pyelonephritis in a man may be associated with prostate disease and an increase in its size.
Pathogenesis of kidney pyelonephritis
Routes of entry of the pathogen into the body:
- hematogenous
- urogenic
- lymphogenous
Factors that influence the development of pyelonephritis:
- Neurogenic bladder dysfunction
- Urinary tract obstruction
- Pregnancy (the tone and peristalsis of the ureters decreases, functional insufficiency of the vesicoureteral valves develops, the dynamics of blood in the kidney changes, the enlarged uterus compresses the ureters)
- Sexual activity
- Vesicoureteropelvic reflux
In chronic pyelonephritis, arterial hypertension may be observed, which is associated with infiltration of interstitial tissue. As a result, the dynamics of blood inside the kidneys is disrupted and the production of renin increases. When the inflammatory process subsides, hypertension disappears. Prerequisites for the preservation of hypertension are created in the case of sclerotic processes in the kidneys, including in the area of the vascular pedicle.
Why does acute pyelonephritis occur?
Movement of infection along an ascending path
The infection enters the bladder through the urethra, then spreads to the canals of the upper structures, then to the kidneys. This is the most common cause of the development of acute pyelonephritis.
This disease is more common in women. The fact is that their urethra is shorter and wider than that of men. The urethra is located in close proximity to the genitals and anus, as a result of which pathogenic microorganisms penetrate into the bladder and then into the kidneys without any difficulty.
As for men, acute pyelonephritis develops due to the presence of an obstruction in the urethra, when it becomes difficult to excrete urine. As a result, it stagnates. As an obstacle, we mean kidney stones, as well as if the prostate tissue has grown. The fluid accumulates, and infectious agents multiply and spread to the organs that produce and filter it.
Women can also develop acute pyelonephritis due to the presence of a cyst, stone, tumor formation, or stricture.
Vesiculourethral reflux
With vesiculourethral reflux, a certain amount of urine backflows. It will be located in the renal pelvis. This happens because the outflow through the ureter is obstructed.
This pathology, which causes inflammation in the kidneys, is in most cases diagnosed in children. An attack of an acute form of the disease in a child is dangerous due to its complications. Scarring of the kidney tissue may occur.
During puberty, an attack of acute pyelonephritis and tissue scarring occurs due to certain physiological characteristics. Namely:
- Low fluid pressure compared to an adult body.
- Children under 5 years of age are unable to completely empty their bladder.
- Reduced immune resistance of the child during the first years of life. This also includes a bacterial infection, since personal hygiene may be insufficiently observed, and there are also no bactericidal components in the urine.
- The disease is difficult to diagnose at an early stage.
- Unlike adults, the descending route of infection is more common in children. The cause may be tonsillitis, caries, scarlet fever and more.
There is a significant decrease in kidney function if tissue begins to scar. Approximately 10% of patients who require hemodialysis develop scar tissue due to pyelonephritis, which they suffered in childhood.
Infectious agent
The most common pathogenic microorganism that provokes the development of pyelonephritis is Escherichia coli. In addition, there are other causative agents of the disease. Namely:
- Staphylococci.
- Proteas.
- Enterococcus.
- Pseudomonas.
- Pseudomonas aeruginosa.
- Enterobacter.
- Pathogenic fungal microorganism.
If the infection moves along an ascending path, E. coli will be present in the urine discharged. It can be determined by undergoing laboratory testing. If the pathogen is introduced during instrumental manipulation, the causes of the disease include Klebsiella, Proteus, and Pseudomonas aeruginosa.
Epidemiology
In the CIS countries, according to statistics, there are 15-16 cases of acute pyelonephritis per 100,000 population. There are also 18 cases of chronic pyelonephritis per 1000 population.
The peak incidence of pyelonephritis occurs in three age periods. The first one is up to 3 years old. For every 8 sick girls there is 1 sick boy. The second peak of incidence occurs during active reproductive age - from 18 to 35 years. For every 7 sick women there is 1 sick male. Elderly and senile age is the third peak of incidence. Starting from the age of 60, the number of sick women and men becomes equal. Among patients over 70 years of age, the majority are men, since they develop tumor and hypertrophic processes in the prostate gland, which disrupts the dynamics of urine.
In the first two age periods, girls and women are more likely to get sick, which is explained by the peculiarities of the hormonal status, which changes during pregnancy and leads to dilatation, hypotension and dyskinesia of the urinary tract. Also another reason is the anatomical and physiological characteristics of the urethra (it is short, the rectum and genital tract are located nearby). The increase in female morbidity is also influenced by the use of oral contraceptives.
Signs of the disease in women
Women are most susceptible to developing pyelonephritis. Symptoms of the disease may vary depending on its form. As a rule, signs of acute pyelonephritis in a woman are:
- Change in the color and odor of urine. The fluid may become cloudy and contain bloody or purulent inclusions.
- Increased body temperature above 38 degrees. In some cases, there is a sharp change in indicators.
- Burning sensation when urinating, frequent visits to the toilet.
- Nausea, accompanied by vomiting, chills.
- Having a headache.
- Painful sensations when tapping with the edge of the palm in the kidney area.
Symptoms
Signs of chronic pyelonephritis are less pronounced than in the acute period and depend on the stage and causes of inflammation of the kidney tissue. The disease has a relapsing course - the active phase is replaced by an asymptomatic one. Remission is characterized by the absence of clinical manifestations of the disease and abnormalities in laboratory tests of urine and blood.
Active inflammation has several forms that determine the clinical picture:
- Latent form.
The patient complains of general malaise, headache, fatigue, low-grade fever. There is no lower back pain or urinary syndrome. In some cases, the release of a small portion of urine or the formation of excess fluid is noted, and slight anemia appears.
- Recurrent form.
It has a wave-like course when the active phase of inflammation goes into remission. Clinically determined by aching pain in the lower back, changes in the volume of urine produced, and painful urination. In the acute stage, pale skin, dizziness, rapid heart rate, and weakness are noted.
- Hypertensive form.
Hypertensive syndrome dominates - dizziness, headaches and heart pain, sleep disturbance, tinnitus, nausea, vomiting, blurred vision. Urinary syndrome is unstable, mild.
- Anemic form.
It occurs with signs of hypochromic anemia: lack of energy, headache, rapid heartbeat, poor appetite, and flickering of spots before the eyes. Urinary syndrome has an intermittent course, hypertensive is not expressed.
The azotemic form is less common
- this disease is detected at the stage of chronic renal failure.
Signs of pyelonephritis in men
Male patients are diagnosed with the disease less frequently than females. This is due to differences in the urinary system. The reasons for the development of pyelonephritis may be diseases that impede the outflow of urine from the kidneys.
As a rule, in males the disease occurs in a chronic form. Signs of the development of pyelonephritis in men are:
- Decreased appetite. Rapid fatigue of the body.
- Difficulty in urinating.
- Moderate intensity pain in the lumbar region.
- Constant thirst.
- Frequent urge to urinate.
In some cases, male patients experience bloody inclusions in their urine. This may indicate displacement of kidney stones.
Classification
There are three stages in the development mechanism of chronic pyelonephritis:
- Stage I.
In the interstitial tissues of the kidneys, many neutrophilic leukocytes are found, which indicates inflammation, the collecting ducts are atrophied, the renal glomeruli are not damaged.
- Stage II.
The stroma and tubules of the kidney are replaced by scar tissue, and the lumens of the tubules narrow. Neurons are involved in the pathological process, the renal glomeruli become empty, and vascular obliteration occurs.
- Stage III.
The kidney loses size, looks wrinkled, and scarring of the kidney tissue is noted.
According to localization, the inflammatory process can be one- or two-sided, according to the etiological factor - primary (initially develops in the kidneys) and secondary (occurs against the background of other diseases and conditions). Based on the patency of the urinary tract, infiltrative and sclerotic forms are distinguished.
Signs of the disease in children
In childhood patients, when the disease manifests itself, a sharp change in body temperature is observed. The indicator exceeds 38 degrees. The disease is accompanied by nausea, vomiting, chills, and girdle pain in the abdomen and lower back. In some cases, constant drowsiness is possible.
If symptoms appear in a child, you should immediately contact a specialist. It is impossible to diagnose pyelonephritis without the presence of appropriate education. The specialist will conduct diagnostic measures and prescribe the necessary treatment. Failure to go to the clinic in a timely manner can lead to the development of complications.
Treatment methods for pyelonephritis
Treatment of pyelonephritis should be carried out under the supervision of a doctor, who will establish this diagnosis through research, prescribe a course of treatment, and monitor the progress of recovery. It is very important not only to treat pyelonephritis itself, but also to eliminate the causes that led to the development of the disease.
For treatment of pyelonephritis in Moscow, you can contact Family Doctor JSC. Treatment of the disease is carried out by urologists.
Doctors at Family Doctor are highly qualified and have extensive experience in treating pyelonephritis in children and adults, which allows them to implement an individual approach that takes into account the characteristics of each specific case of the disease.
Drug treatment
Treatment of pyelonephritis is carried out using antibacterial therapy and anti-inflammatory drugs. To strengthen the immune system, immunomodulators and multivitamins are used. For chronic pyelonephritis, diuretics and drugs that improve renal blood flow are also prescribed.
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Rate how useful the material was
thank you for rating
Signs of pyelonephritis in pregnant women
In some cases, the disease occurs in pregnant women. The form of pyelonephritis in pregnant women can be either acute or chronic. Most often the disease manifests itself at the end of the second, beginning of the third trimester.
The occurrence of pyelonephritis is promoted by an increase in the volume of the uterus. It begins to put pressure on the ureters, disrupting the normal flow of urine. With stagnation in the kidneys, pathogenic microorganisms begin to multiply.
During pregnancy, a woman's kidneys are subject to high stress. The disease can occur simultaneously with cystitis. It is impossible to diagnose pyelonephritis in a pregnant woman without specialized education and experience.
Lifestyle and prevention
During treatment and during the recovery period, diet No. 7 is indicated. Adequate hydration is important. Vigorous activity should be kept to a minimum. Patients receiving outpatient treatment can begin work two weeks after their condition returns to normal, that is, on average 21 days after the onset of the disease.
Prevention of OP consists of reducing the intensity of sexual life, conducting a preventive course of antibiotic therapy (for example, for bacteriuria in pregnant women), as well as early detection and treatment of cystitis.
If prophylactic measures have not eliminated the pathogen or reinfection or relapse (reinfection less than two weeks after completion of a course of antibiotics) has occurred, the patient should be carefully examined for anatomical, functional, or structural abnormalities of the kidneys.
What complications can there be?
With improper treatment or its absence, complications may develop. The pathology is especially dangerous for pregnant women and people with diabetes. The pathology is amenable to therapeutic treatment. Untimely or incorrect treatment contributes to the development of complications, in some cases leading to the death of the patient.
One of the complications of the disease is sepsis. If left untreated, pathogenic bacteria multiply rapidly. Once the limit is reached, microorganisms enter the bloodstream. Thus, the infection spreads throughout the body. The complication in some cases ends in the death of the patient.
In addition to sepsis, other complications may develop, such as kidney abscess, emphysematous pyelonephritis, kidney carbuncle, etc.
Symptoms
Pyelonephritis is divided into acute and chronic.
Acute is divided into primary pyelonephritis, which can develop in a practically healthy person, and secondary, which, in turn, can be obstructive and non-obstructive. A secondary obstructive process occurs when the outflow of urine is disrupted (a tumor blocking the ureters, their blockage with a stone and other conditions), and a secondary non-obstructive process occurs as a result of ascending (urinogenic) infection in inflammatory diseases of the urinary tract (urethritis, cystitis).
Chronic pyelonephritis can be a consequence of acute or occur as an independent disease.
The symptoms of an acute disease differ from the symptoms of a chronic one, however, secondary obstructive pyelonephritis has some similarities with the chronic process, so it is often difficult to differentiate them, in such cases the formulation “not specified as acute or chronic” can be used.
Acute pyelonephritis
The acute process is characterized by a sharp onset with an increase in body temperature to 38-39 °C and chills. The general condition is disturbed - weakness, headache, thirst appear, and with severe intoxication, nausea and vomiting are possible. There is pain in the lower back on palpation and a positive Pasternatsky sign - sharp pain when tapping the kidney area on the affected side. In some cases, swelling and increased blood pressure may occur.
With secondary pyelonephritis, urination disorders may occur - difficulty, pain, burning. Visually, the urine may become cloudy, mixed with flakes.
Chronic pyelonephritis
It may occur without a pronounced clinical picture, accompanied by minor disturbances in the general condition: weakness, lethargy, periodically low-grade fever, mild pain in the lumbar region with irradiation to the groin area and the anterior surface of the thigh.
With a long ongoing process, the patient develops signs of intoxication (weakness, chills, anemia), swelling of the face in the morning, frequent urination, and frequent nighttime urges to go to the toilet. Arterial hypertension may develop in 50-75% of cases.
Pain on palpation and a positive Pasternatsky sign are also present in the chronic form, however, if acute pyelonephritis is more often one-sided, then chronic pyelonephritis often affects both kidneys.
During chronic pyelonephritis, stages of remission and exacerbation are distinguished. In some cases, there are no symptoms, and the pathology is detected by chance, based on test results.
Features in certain categories of patients
The symptoms of pyelonephritis have characteristics in children and the elderly. In children, symptoms of intoxication often come to the fore; abdominal syndrome may develop - pain is localized in the abdomen, and not in the lumbar region. In elderly and senile age, the disease often occurs with a blurred clinical picture; local symptoms (pain syndrome) are dominated by general symptoms (weakness, fever, intoxication).
Diagnostic measures
If any symptoms appear, you should immediately contact a specialist. The doctor will examine, interview the patient and prescribe the necessary diagnostic measures. This allows the specialist to prescribe the correct treatment depending on the degree of development of the disease and its form. To make a diagnosis, the doctor:
1. Collects anamnesis based on the patient’s words and the studied medical documentation. The specialist pays attention to infectious diseases suffered by the patient, as well as disorders of the urinary system.
2. Interviews and examines the patient.
3. Prescribes laboratory tests and diagnostic measures using specialized equipment.
4. Tests prescribed for the diagnosis of pyelonephritis
5. To make a correct diagnosis, the specialist prescribes tests. In order to detect pyelonephritis, the following tests must be performed:
6. General blood and urine analysis.
7. Biochemical blood test.
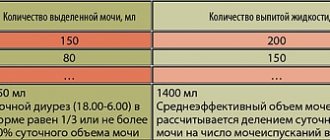
8. Zimnitsky test.
9. Urinalysis according to Nechiporenko.
10. Bacteriological analysis of urine.
The results of blood tests can determine the presence of inflammation in the body. It is indicated by an excess of the norm in the concentration of leukocytes and the erythrocyte sedimentation rate. In addition, the biochemical composition will change.
The urine collection procedure may affect the test results. Correct collection of biomaterial involves performing a morning toilet of the external genitalia and further collecting urine. To collect biomaterial, a specialized plastic container with a lid is used. With pyelonephritis, a general urine test shows an increased level of bacteria and leukocytes. When urine density is low, its pH is alkaline. There is protein and glucose in the urine. In some cases, bloody inclusions are possible.
Conducting research using specialized equipment
To make the correct diagnosis and prescribe treatment, specialists use instrumental diagnostic methods. The doctor resorts to this method after interviewing and examining the patient. Diagnosis is carried out using the following methods:
Ultrasonography. This diagnostic method allows you to determine the density of organs and their sizes. The doctor pays attention to changes and deviations from the norm. The reflection of ultrasonic waves (echogenicity) increases in chronic pyelonephritis, and decreases unevenly in acute pyelonephritis.
CT scan. Allows the specialist to get the most complete picture.
Excretory urography. A diagnostic method that allows you to examine the kidneys and urinary tract. The patient is given a radiopaque contrast agent intravenously. After an X-ray examination, it is possible to determine the structural features of the organs of the urinary system. Contraindication to excretory urography is individual intolerance to drugs.
Cystography. The method involves filling the bladder with a radiopaque substance by excretory urography or by introducing it through the urethra. Cystography is performed to detect vesicoureteral reflux.
When carrying out diagnostic measures for female patients, the specialist prescribes a gynecological examination.
Publications in the media
Pyelonephritis is a nonspecific infectious disease of the kidneys with predominant damage to interstitial tissue and the collecting system.
Classification • Course •• Acute: serous or purulent •• Chronic: latent and recurrent (occurs with exacerbations) • Primary (developed in a healthy kidney without urodynamic disturbances) and secondary (developed against the background of kidney disease, developmental anomalies or urodynamic disturbances: ureteral stricture , benign prostatic hyperplasia, urolithiasis, urinary tract atony, reflux dyskinesia) • Phases: exacerbation (active pyelonephritis), remission (inactive pyelonephritis) • Localization: unilateral (rare), bilateral • With the presence of arterial (symptomatic) hypertension • Complications: uncomplicated (usually in outpatients), complicated - abscess, sepsis (more often in inpatients, during catheterizations, in case of urodynamic disorders - urolithiasis, polycystic kidney disease, benign prostatic hyperplasia, in immunodeficiency states - diabetes, neutropenia) • Kidney function - intact, dysfunction, chronic renal failure • Community-acquired pyelonephritis (outpatient) and nosocomial (nosocomial) - developed within 48 hours of hospital stay • Special clinical forms •• Pyelonephritis of newborns and children •• Pyelonephritis of the elderly and senile age •• Gestational pyelonephritis - pregnant women . its fiber.
Statistical data • Morbidity according to appeal - 18 cases per year per 1000 population. Women get sick 2-5 times more often than men, girls - 6 times more often than boys. In older men with benign prostatic hyperplasia, pyelonephritis occurs more often than in younger men. Etiology • In acute pyelonephritis, most often monoflora, in chronic - associations of microbes •• Escherichia coli (75%), Proteus mirabilis (10–15%), Klebsiella and Enterobacter, Pseudomonas, Serratia, Enterococcus, less often - Candida albicans, Neisseria gonorrhoeae, Trichomonas vaginalis, Staphylococcus and Mycobacterium tuberculosis • In community-acquired pyelonephritis, E. coli is cultured in 80% of cases; in hospital-acquired pyelonephritis, it also predominates, but the frequency of coccal flora increases. Pathogenesis • Urodynamic disorders • Pre-existing kidney diseases, especially interstitial nephritis • Immunodeficiency conditions (treatment with cytostatics and/or prednisolone, diabetes, defects in cellular and humoral immunity) • Hormonal imbalance (pregnancy, menopause, long-term use of contraceptives) • Routes of infection •• Hematogenous - from an extrarenal focus (felon, boil, tonsillitis), with septicemia •• Ascending - from the lower urinary tract along the wall of the ureter in the presence of reflux (vesicoureteral, ureteropelvic, renal pelvis), after cystoscopy. Pathomorphology • In acute pyelonephritis, the kidney is enlarged in size, the capsule is thickened. In the interstitial tissue (cortex and medulla) there are perivascular leukocyte infiltrates with a tendency to form abscesses. When pustules merge or a vessel is blocked by a septic embolus, necrotic papillitis, an abscess, a kidney carbuncle may occur • Chronic pyelonephritis goes through stages from perivascular infiltration, focal sclerosis to kidney shrinkage - the kidney is reduced in size, the surface is lumpy, in places of sclerosis there are tissue retractions, the capsule is fused with kidney parenchyma, is difficult to remove.
CLINICAL MANIFESTATIONS Acute pyelonephritis often occurs with a clear clinical picture, with purulent pyelonephritis similar to a septic or infectious disease • Febrile fever with chills, heavy sweat • Pain in the lumbar region, tenderness on palpation, Pasternatsky’s symptom is positive, on the side of pyelonephritis - tension in the anterior abdominal wall (phenomena of peritonism) • Urinary syndrome - polyuria (more often) or oliguria (less often) with loss of fluid through the lungs and skin, dysuria - frequent and painful urination • Intoxication syndrome - headache, nausea, vomiting • With bilateral acute pyelonephritis, the development of acute renal failure is possible. Chronic pyelonephritis in most patients (50–60%) has a latent course • Low-grade fever, sweating, chills • Pain in the lumbar region, Pasternatsky’s symptom is positive • Urinary syndrome - polyuria, nocturia, less often dysuria • Symptoms of intoxication • Arterial hypertension (more than 70% of cases ) • Anemia (in some patients) • Clinical signs of exacerbation - increased body temperature (not always), increased blood pressure, increased or appearance of lower back pain, polyuria, dysuria, nocturia. Laboratory tests • Acute pyelonephritis •• Blood test ••• Increased ESR, neutrophilic leukocytosis, sometimes leukopenia, shift of the leukocyte formula to the left (with purulent pyelonephritis) ••• Increased urea and creatinine in the blood (with acute renal failure) •• Urine. May be cloudy (mucus, bacteria, desquamated epithelium), leukocyturia (neutrophils), active leukocytes (Sternheimer-Malbin, “pale”, arachnid) - formed in urine with low osmolarity (with hematogenous introduction, infections may be absent in the first days, with obstruction there are no ureters), bacteriuria, proteinuria, erythrocyturia (less commonly, hematuria - with necrosis of the renal papillae), hyposthenuria (possible hypersthenuria with oliguria) • Chronic pyelonephritis. In urine analysis: moderate proteinuria, leukocyturia, bacteriuria, microhematuria, Sternheimer-Malbin cells, active leukocytes, hyposthenuria, alkaline reaction of urine (especially characteristic of infection with Proteus, Klebsiella and Pseudomonas species) • Bacteriological culture of urine is required (more than 103–5 microbes in 1 ml of urine) with determination of the sensitivity of the isolated microflora to antibiotics. Instrumental data • Ultrasound of the kidneys •• In acute pyelonephritis - increase in size, decreased echogenicity, spasm of the pyelocaliceal system, smooth contours of the kidney; in case of renal carbuncle - cavity formation in the parenchyma •• In chronic pyelonephritis - decreased size, increased echogenicity, deformation and expansion pyelocaliceal system, tuberosity of the contours of the kidney, asymmetry of size and contours •• With obstruction of the urinary tract - signs of hydronephrosis on the affected side, stones. • Plain radiography: an increase or decrease in volume of one of the kidneys, tuberous contours, and sometimes a shadow of a stone. • Excretory urography (contraindicated in the active phase, with chronic renal failure) •• In acute pyelonephritis - late contrast on the affected side, decreased intensity of contrast, slower removal of contrast •• In chronic pyelonephritis, in addition to these symptoms - expansion and deformation of the calyces and pelvis. • Angiography: in the early stages - a decrease in the number of small branches of the segmental arteries until their disappearance, in the later stages - the kidney shadow is small, there is no border between the cortical and medulla layers; Deformations of blood vessels, narrowing and reduction in their number are detected. • Radioisotope renography and scintigraphy: kidney sizes are normal or reduced, isotope accumulation is reduced, the secretory and excretory phases of the curve are lengthened. • Chromocystoscopy •• In acute pyelonephritis - discharge of turbid urine from the mouth of the ureter of the affected kidney (or both kidneys), delayed or weakened release of indigo carmine on the affected side •• In chronic pyelonephritis, dysfunction of the affected kidney is also determined, but in many patients there is no disturbance in the release of indigo carmine discover.
Diagnosis • The diagnosis of active pyelonephritis (acute or exacerbation of chronic) is made on the basis of the clinical “triad” - fever, lower back pain, dysuria; laboratory data confirm the diagnosis (see above), incl. results of bacteriological urine culture and determination of sensitivity to antibiotics, instrumental data. • In case of latent pyelonephritis, it is advisable to conduct a prednisolone test (30 mg of prednisolone in 10 ml of 0.9% sodium chloride solution intravenously). The test is positive if, after the administration of prednisolone, the content of leukocytes and bacteria in the urine doubles. • Urinalysis according to Nechiporenko, the leukocyte formula of urine allows us to differentiate chronic pyelonephritis and glomerulonephritis: •• with glomerulonephritis, the number of erythrocytes exceeds the number of leukocytes, with pyelonephritis the number of leukocytes is higher •• with glomerulonephritis, lymphocytes predominate in the leukocyte formula of the blood, with pyelonephritis - neutrophils. • With chronic pyelonephritis, the concentrating ability of the kidneys is disrupted early (Zimnitsky test), with glomerulonephritis - later, at the stage of development of chronic renal failure. • Differential diagnosis • Infectious diseases accompanied by fever (typhoid fever, malaria, sepsis) • Pyonephrosis • Hydronephrosis • Acute purulent disease of the lower urinary tract • Kidney infarction • Acute glomerulonephritis • Pneumonia • Cholecystitis • Acute pancreatitis • Acute appendicitis • Splenic infarction • Dissecting aneurysm ism aorta • Herpes zoster. Associated diseases • Urinary tract obstruction • Urinary tract abnormalities • Pregnancy • Nephrolithiasis • Diabetes • Immunodeficiency conditions.
TREATMENT Diet • In the acute period - table No. 7a, then No. 7. Fluid consumption up to 2–2.5 l/day • With calculous pyelonephritis, the diet depends on the composition of the stones: with phosphaturia - acidifying urine, with uraturia - alkalizing. General tactics • Restoration of the patency of the upper and lower urinary tracts • Antibacterial therapy - on average 4 weeks (2-6 weeks) • Drugs that have an antispasmodic effect (platiphylline, papaverine hydrochloride, belladonna extract, etc.) • For oliguria - diuretics • Combating dehydration (with polyuria, fever) • For metabolic acidosis - sodium bicarbonate orally or intravenously • Antihypertensive therapy • For chronic pyelonephritis without exacerbation - resort treatment in Truskavets, Essentuki, Zheleznovodsk, Sairm • Surgical treatment - if necessary. Drug therapy • The goal is to eliminate the activity of the process, eradicate the pathogen. The criterion for the effectiveness of therapy is the normalization of clinical and laboratory parameters, abacteriuria • Antibacterial therapy for at least 2 weeks in courses of 7–10 days, empirical (before inoculating the pathogen) and targeted (after determining the sensitivity of the microflora to antibiotics) • Acute community-acquired pyelonephritis - begin with semisynthetic penicillins (ampicillin, amoxicillin; alternative drugs - protected penicillins such as amoxicillin + clavulanic acid, ampicillin + sulbactam) or oral cephalosporins (cephalexin, cefuroxime, cefaclor); it is also possible to prescribe co-trimoxazole, doxycycline •• Acute nosocomial pyelonephritis - start with fluoroquinolones (norfloxacin, ciprofloxacin, ofloxacin, levofloxacin, lomefloxacin); alternative drugs - protected penicillins, II-III generation cephalosporins, gentamicin + ampicillin (amoxicillin, carbenicillin), imipenem + cilastatin •• Exacerbation of chronic ambulatory pyelonephritis - start with protected penicillins, drugs of choice - fluoroquinolones, co-trimoxazole, cephalosporins (all drugs for prima orally) •• Exacerbation of chronic nosocomial pyelonephritis - start with fluoroquinolones, drugs of choice except those mentioned above - imipenem + cilastatin, gentamicin + ampicillin (cephalosporins II–III, azlocillin, carbenicillin, piperacillin), cephalosporins III + protected penicillins •• If staphylococcal pyelonephritis - vancomycin + oxacillin + gentamicin (amikacin) •• Anti-relapse therapy is carried out for 3-12 months, 7-10 days of each month, for purulent pyelonephritis - antibiotics (see above), for serous - uroantiseptics, alternately: nalidixic acid according 0.5–1 g 4 times/day, nitrofurantoin 0.15 g 3–4 times/day, nitroxoline 0.1–0.2 g 4 times/day. It is also effective to prescribe uroantiseptics once a night: co-trimoxazole, trimethoprim or nitrofurantoin 100 mg at night or 3 times a week (preventatively) • Immunocorrection • For acidosis - sodium bicarbonate 1-2 g orally 3 times a day or 100 ml 4% IV solution • For anemia - iron supplements, blood transfusion, red blood cell transfusion. Surgical treatment • For purulent pyelonephritis, in case of failure of conservative therapy - decapsulation of the kidney, pyelonephrostomy and drainage of the renal pelvis •• The calculus is removed only under the condition that the volume of the operation will not be significantly increased •• Stones from the pelvic ureter are removed when the patient recovers from a serious condition • For renal carbuncle - dissection of the inflammatory-purulent infiltrate or resection of the affected area of the kidney • For obstructive pyelonephritis, interventions are aimed at eliminating the obstacle to the outflow of urine (for example, removal of a stone) • For xanthogranulomatous pyelonephritis, partial excision of the kidney is performed.
Complications • Necrosis of the renal papillae • Renal carbuncle • Apostematous nephritis • Pyonephrosis • Paranephritis • Urosepsis, septic shock • Metastatic spread of purulent infection in the bones, endocardium, eyes, membranes of the brain (with the appearance of epileptic seizures) • Secondary parathyroidism and renal osteomalacia (with chronic pyelonephritis due to renal losses of calcium and phosphates) • Pyelonephritis wrinkled kidney • Nephrogenic arterial hypertension • Hypotrophy of newborns (with pyelonephritis in pregnant women) • Acute and chronic renal failure. Current and prognosis . The prognosis worsens as the duration of pyelonephritis increases, with nosocomial pyelonephritis, microbial resistance to antibacterial agents, urinary tract obstruction, the presence of purulent complications, immunodeficiency states, and frequent relapses. Complete recovery from acute pyelonephritis is possible with early diagnosis, rational antibiotic therapy, and the absence of aggravating factors. 10–20% of patients with chronic pyelonephritis develop chronic renal failure. In 10% of patients with arterial hypertension, it becomes malignant. Concomitant pathology • Urolithiasis • Renal tuberculosis • Benign prostatic hyperplasia • Uterine prolapse • Purulent-septic diseases • Diabetes • Spinal disorders. Pyelonephritis and pregnancy • Acute pyelonephritis affects 7.5% of pregnant women (usually right-sided). In the first pregnancy, pyelonephritis most often begins in the 4th month of pregnancy, in the second pregnancy - in the 6th–7th month • Features of the clinical picture: pain in the lower abdomen, dysuria. The disease begins with chills and fever. Severe intoxication, which is caused by renal pelvic reflux resulting from stretching of the renal pelvis • Pyelonephritis during pregnancy is an indication for emergency hospitalization. Termination of pregnancy is indicated only if there is a threat of urosepsis, the development of acute renal failure, or the addition of preeclampsia.
Age characteristics • Pyelonephritis in childhood •• The disease often occurs against the background of congenital anomalies of the urinary system (stenosis of the urethra, bending of the ureter, etc.), dysmetabolic processes (oxalaturia, uraturia) •• Possible rapid onset with high body temperature or latent - with low-grade fever •• Other symptoms: enuresis, pain or itching in the external genital area in girls, gastrointestinal dysfunction, swelling and pain in the lumbar region •• During treatment, a forced rhythm of urination is additionally prescribed. • Pyelonephritis in elderly and senile people. The disease proceeds latently. Characterized by decreased reactivity and mild clinical manifestations. Symptoms of general intoxication predominate. In men, pyelonephritis often develops against the background of benign prostatic hyperplasia. Prevention • Timely treatment of foci of infection • Treatment of urinary tract diseases that impede the outflow of urine • Regimen: balanced diet, prevention of overwork • Rational treatment of acute pyelonephritis. Synonyms • Ureteropyelonephritis • Ascending nephritis • Interstitial nephritis.
ICD-10 • N10 Acute tubulointerstitial nephritis • N11 Chronic tubulointerstitial nephritis.