Acute pyelonephritis (kidney inflammation)
is a rapidly developing and life-threatening disease. It is characterized by increasing serous-purulent inflammation in the kidney, leading to severe intoxication (poisoning of the body with infectious and other toxins).
In this case, the patient most often complains of pain in the lumbar region (“impossible to touch”), fever (up to 39 degrees with chills), severe general weakness, headache, nausea, vomiting, dry mouth, bloating. In the absence of adequate treatment for kidney inflammation, a picture of infectious-toxic shock may develop: a drop in blood pressure, loss of consciousness, tachycardia, pallor of the skin.
The main distinguishing feature of acute kidney inflammation is the possibility of rapid progression with a fatal outcome. The reason for this is the peculiarities of the blood supply. 20-25 percent of the circulating blood “passes” through the kidneys, so in a situation where the kidney turns into, in fact, an abscess, there is a danger of generalization of inflammation (spread to the entire body).
Causes of acute pyelonephritis
– an infectious process in the kidney caused by bacteria. Pathogens (usually Escherichia coli - E.Coli) can enter the organ in two main ways: from the lower urinary tract (for example, from the bladder in chronic cystitis) and from the blood (for example, if there is a focus of infection somewhere - caries, tonsillitis, sinusitis, etc.). However, out of the blue, pyelonephritis (inflammation of the kidneys) develops extremely rarely. Most often, there are so-called “predisposing factors”: urolithiasis, abnormal development of the genitourinary organs, the presence of narrowing of the ureters, prostate adenoma, etc.
If acute pyelonephritis is suspected, the patient must be immediately hospitalized in a specialized clinic.
Drugs against kidney stones
Tablets for the kidneys, which dissolve and remove stones for urolithiasis (nephrolithiasis, urolithiasis), are not the same. The choice of product depends on the type of stones, which can be urate, oxalate, phosphate and others. After tests, ultrasound, and radiography, the patient will be offered the following medications:
- Allopurinol, the active substance is allopurinol. Disturbs the synthesis of uric acid, suitable for dissolving urates. When taken, it increases the excretion of urates in the urine and prevents salts from depositing in the kidneys. It can also be used in complex therapy of calcium oxalate nephrolithiasis.
- Blemaren, active substances sodium citrate, potassium bicarbonate. Dissolves urates, prevents the formation of calcium oxalate stones. Produced in the form of effervescent tablets.
- Xidifon, active substance etidronic acid. It works against phosphorus and calcium stones, and is also indicated for certain types of nephritis.
- Tiopronin and Penicillamine. Medicines can be used to treat all types of nephrolithiasis.
Also effective drugs for treating kidney stones are Litostat, Potassium citrate, Biliurin, Urodan. The duration of treatment can be 3-12 months.
Chronic pyelonephritis (kidney inflammation)
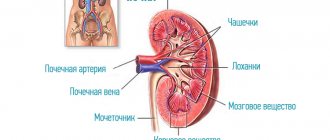
– a sluggish infectious and inflammatory disease characterized by damage to the tissue (panenchyma) and pyelocaliceal system of the kidney.
During this disease, two phases can be distinguished. Remission is the subsidence of the pathological process. Exacerbation is the manifestation of vivid clinical, laboratory and pathomorphological symptoms.
Chronic kidney inflammation is usually based on two components: a violation of the outflow of urine from the kidneys and the presence of a urinary tract infection.
Causes of chronic pyelonephritis
- usually develops after acute pyelonephritis. The main causes of chronic kidney inflammation are as follows:
- Unresolved disturbance of urine outflow (acute pyelonephritis was treated with antibiotics, but the cause was not eliminated),
- Incorrect treatment of acute pyelonephritis (insufficient duration of treatment, inadequate medications),
- Chronic foci of infection in the body (tosillitis, caries, enterocolitis, etc.),
- Immunodeficiency conditions and metabolic diseases (for example, diabetes).
Chronic pyelonephritis is an extremely common disease. In adults, kidney inflammation occurs in more than 200 people per thousand of the population. Moreover, women suffer from this disease 4-5 times more often than men. Chronic pyelonephritis is the most common cause of chronic renal failure.
Chronic kidney inflammation is a sluggish but dangerous disease. Its essence lies in the fact that as it develops (periodic activation and attenuation of inflammation), gradual scarring of the kidney tissue occurs. Ultimately, the organ is completely replaced by scar tissue and ceases to perform its function.
In the remission phase, chronic pyelonephritis can proceed for years without clear clinical symptoms. In the initial phases of kidney inflammation, patients may periodically notice mild malaise, an increase in body temperature to subfebrile levels (up to 37.5 degrees), decreased appetite, increased fatigue, mild dull pain in the lumbar region, and pale skin. Urinalysis shows a moderate increase in the number of leukocytes and bacteriuria. With further development of kidney inflammation, progression of the described complaints is noted. Impaired kidney function leads to thirst, dry mouth, increased urine production, and night urination. In laboratory tests, the density of urine decreases. As the pathological process deepens in the kidneys, nephrogenic arterial hypertension (increased pressure) develops, which is particularly “malignant”: high diastolic pressure (more than 110 mmHg) and resistance to therapy. In the final stages of the disease, symptoms of chronic renal failure are observed.
A separate nosology is “ asymptomatic bacteriuria
“- a situation where there are no clinical or laboratory symptoms, but an increased number of bacteria is detected in the urine. In such a situation, the likelihood of developing a manifest urinary tract infection against the background of hypothermia, decreased general immunity and other provoking factors is increased. Asymptomatic bacteriuria is a reason to consult a urologist and find out its causes!
pyelonephritis of pregnant women” is especially dangerous.
" Its essence lies in the fact that the enlarged uterus compresses the ureters and the outflow of urine is disrupted. Against this background, severe forms of pyelonephritis may develop, the treatment of which is very difficult, since most antibiotics are contraindicated during pregnancy. In this regard, pregnant women require constant monitoring of urine parameters. And when pyelonephritis (inflammation of the kidneys) occurs, the installation of internal ureteral stents is often required to drain urine from the kidneys.
Antispasmodics
Drugs in this group are indispensable for renal colic. The latter can occur both during an acute inflammatory process and when a stone moves through the ureter. Due to irritation of the nerve endings, smooth muscles spasm, resulting in increased pain. Taking an antispasmodic relaxes the urinary tract, urine flow is restored, small stones leave the body, and the pain goes away.
There are different types of antispasmodics that can be used for kidney diseases:
- Neurotropic drugs (with central action). They block the transmission of pain signals to muscle cells, as a result the fibers stop spasmodic contraction. Particularly popular are M-anticholinergic drugs - Atropine, Platiphylline, Metacin, Gomatropine.
- Myotropic drugs. They work at the local level, act directly on the muscles of the ureters and bladder, helping them relax. This group includes well-known drugs - No-shpa, Drotoverine, Mebeverine, Papaverine.
Usually, with renal colic, a person takes two tablets of No-shpa, because this medicine is most often offered in pharmacies for a similar problem. If the pain is severe and unbearable, it is better to inject No-shpa - the lumen of the ureter will quickly expand, the risk of obstruction will decrease, as will the pain syndrome.
Treatment of pyelonephritis
consists primarily in eliminating its cause - the underlying disease (urolithiasis, ureteral strictures, prostate adenoma, etc.). In addition, adequate antimicrobial therapy is necessary, selected on the basis of urine culture and determination of the sensitivity of bacteria to antibiotics. There are a number of additional treatments for kidney inflammation.
What's important? The patient must understand that chronic pyelonephritis is a “gentle killer” of the kidneys. And if you don’t fight it, it will probably lead you to the hemodialysis department. Modern methods of treating kidney inflammation make it possible to effectively prevent the development of this disease.
How do medications work?
The choice of medication for the treatment of a particular disease will depend entirely on the symptoms, cause, type of pathology, and it should be entrusted to a doctor (urologist, nephrologist). The optimal selection of a drug or complex of drugs works as follows:
- Eliminates or reduces the etiological factor - the presence of stones, sand, bacteria;
- Has a symptomatic effect - alleviates the manifestations of the disease to the maximum;
- Normalizes the functioning of the organ;
- Prevents the disease from becoming chronic or recurrent.
Usually a whole range of medications is used for treatment. For example, to reduce symptoms and relieve inflammation in pyelonephritis, you will have to take antibiotics, antispasmodics, painkillers, and herbal remedies.
When kidney stones appear, you need to drink not only drugs that dissolve them, but also diuretics to remove sand, and antiseptics to eliminate associated inflammation.
Each group of drugs acts in its own way, here are the main ones:
- Diuretics;
- Anti-inflammatory and painkillers;
- Antibiotics, uroantiseptics;
- Herbal medicines and vitamins;
- Antispasmodics.
In complex therapy, the patient may also be prescribed corticosteroids, vascular agents, drugs to improve venous outflow, antihistamines and drugs to lower blood pressure. For oncological diseases, specific treatment is carried out under the supervision of an oncologist.
Herbal medicines for the kidneys
There are a number of plants that are natural uroantiseptics, so many herbal remedies for kidney therapy have been created on their basis. Here are the most famous medicines (composition in brackets):
- Canephron (centaury, rosemary, lovage). It has a diuretic and disinfecting effect, helps with sand, kidney stones, gently removes them and relieves inflammation. Available in drops and tablets.
- Nephroleptin (lingonberry, knotweed, bearberry, propolis, licorice). Has a diuretic, analgesic, anti-inflammatory effect.
- Cyston (mumiyo, extracts of vernonia, onosma, madder, saxifrage and other plants). The drug is a local immunomodulator, improves resistance to infection in chronic nephritis, and also prevents the formation of stones.
- Phytolysin (lovage, knotweed, parsley, wheatgrass, fenugreek, onion, horsetail, pine oil, sage, orange, mint). The medicine is a natural preparation for dissolving all types of stones, and perfectly washes away sand. It is produced in the form of a paste, which is diluted in water.
- Urolesan (oregano, castor oil, carrot extract, mint, fir oil, hop extract). Antispasmodic, diuretic, acidifies urine, prevents the formation of urates.
Typically, herbal remedies are prescribed for 2-3 months, otherwise the effect may be temporary and insufficient. Other well-known herbal medicines are Fitolit, Prolit, Ginjaleling, Rowatinex.
Are there any side effects from the drugs?
Any drug has its side effects, and abuse of use is not recommended. Among the side effects of herbal remedies, allergic reactions (rash, itchy skin) are most often observed, and less often - abdominal pain, nausea, and signs of individual intolerance to the components.
Antispasmodics can disrupt the gastrointestinal tract, reduce blood pressure, cause nausea, vomiting, and rarely, breathing problems and insomnia. A number of medications provoke headaches, heart rhythm disturbances, and changes in blood composition when taken for a long time.
Unpleasant effects from taking stone dissolvers are diarrhea, imbalance of salts in the body, changes in metabolism. NSAIDs have the most severe side effects - long-term use often results in ulcers and gastritis, erosions and gastrointestinal bleeding.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
If you find an error, please select a piece of text and press Ctrl+Enter