The heart is a muscular pump that ensures continuous movement of blood through the vessels. Together, the heart and blood vessels make up the cardiovascular system. This system consists of the systemic and pulmonary circulation. From the left side of the heart, blood first moves through the aorta, then through large and small arteries, arterioles, and capillaries. In the capillaries, oxygen and other substances necessary for the body enter the organs and tissues, and from there carbon dioxide, metabolic products, are removed. After this, the blood turns from arterial to venous and again begins to move towards the heart. First along the venules, then through smaller and larger veins. Through the inferior and superior vena cava, blood again enters the heart, only this time into the right atrium. A large circle of blood circulation is formed.
Venous blood from the right side of the heart is sent through the pulmonary arteries to the lungs, where it is enriched with oxygen, and returns to the heart again - this is the pulmonary circulation.
Inside, the heart is divided by partitions into four chambers. The two atria are divided by the interatrial septum into the left and right atria. The left and right ventricles of the heart are separated by the interventricular septum. Normally, the left and right parts of the heart are completely separate. The atria and ventricles have different functions. The atria store blood that flows into the heart. When the volume of this blood is sufficient, it is pushed into the ventricles. And the ventricles push blood into the arteries, through which it moves throughout the body. The ventricles have to do more hard work, so the muscle layer in the ventricles is much thicker than in the atria. The atria and ventricles on each side of the heart are connected by the atrioventricular orifice. Blood moves through the heart in only one direction. In the systemic circle of blood circulation from the left side of the heart (left atrium and left ventricle) to the right, and in the small circle from the right to the left.
The correct direction of blood flow is ensured by the valve apparatus of the heart:
Valves:
- tricuspid
- pulmonary
- mitral
- aortic
They open at the right time and close, preventing blood flow in the opposite direction.
Aortic valve
Closes the entrance to the aorta. It also consists of three valves, which look like crescents. Opens when the left ventricle contracts. In this case, blood enters the aorta. When the left ventricle relaxes, it closes. Thus, venous blood (poor in oxygen) from the superior and inferior vena cava enters the right atrium. When the right atrium contracts, it moves through the tricuspid valve into the right ventricle. Contracting, the right ventricle ejects blood through the pulmonary valve into the pulmonary arteries (pulmonary circulation). Enriched with oxygen in the lungs, the blood turns into arterial blood and moves through the pulmonary veins to the left atrium, then to the left ventricle. When the left ventricle contracts, arterial blood enters the aorta through the aortic valve under high pressure and spreads throughout the body (systemic circulation).
The heart muscle is called the myocardium
There are contractile and conductive myocardium. The contractile myocardium is the actual muscle that contracts and produces the work of the heart. In order for the heart to contract in a certain rhythm, it has a unique conduction system. The electrical impulse to contract the heart muscle occurs in the sinoatrial node, which is located in the upper part of the right atrium and spreads through the conduction system of the heart, reaching every muscle fiber
First, both atria contract, then both ventricles, thereby ensuring the flow of blood to all organs and tissues of the body. The heart muscle has two membranes (external and internal). The inner lining of the heart is called the endocardium. The outer lining of the heart is called the pericardium.
Treatment tactics
Treatment of pulmonary artery diseases depends on the severity of the process. As for stenosis, in the absence of pronounced manifestations, there is no need for surgical intervention, but clinical observation and symptomatic therapy are required.
As the pathology progresses, the question of surgical treatment arises. When the pressure gradient increases above 50 mmHg, the question of surgery is not discussed - it must be performed immediately. Operation options are different. Valvuloplasty can be open, closed, endoscopic - balloon. Indications for a specific intervention are determined by a specialist.
The main directions in the treatment of pulmonary hypertension are the prevention of thrombosis, elimination of spasm of vascular smooth muscle fibers, stopping the proliferation of connective tissue structures of the vascular wall. In this case, the following application is indicated:
· drugs that normalize blood clotting;
· diuretics;
cardiac glycosides;
· vasodilators;
· oxygen therapy.
In case of hypertension, called secondary, complex measures should correct the underlying pathology - the root cause of the increase in pressure in the artery. The list often includes bronchodilators and corticosteroids.
Surgical treatment for hypertension: embolectomy, lung transplant, pulmonary-cardiac complex transplant.
Conduction system of the heart
The heart, like any organ, has its own nervous system. The nervous system of the heart has several levels. The first and main pacemaker of the heart is the sinus node, located in the right atrium. It is subject to the atrioventricular node, which is located on the border between the atria and ventricles and quite often slows down the heart rate set by the sinus node. Then the nerve impulse goes to the ventricles of the heart along the branches of the Hiss bundle, which are divided into the smallest nerve endings - Purkinje fibers.
Types of pulmonary embolism
Experts distinguish between small, submassive, massive (two or more lobar arteries) and fatal acute embolism with the volume of the pulmonary artery turned off 25%, 50%, more than 50% and more than 75%, respectively. In 10-25% of cases, following an embolism, a pulmonary infarction develops.
Symptoms of the disease
The clinical picture of pulmonary embolism varies significantly from an almost complete absence of symptoms (“silent” embolism) to a rapidly developing state of pulmonary heart failure in the acute stage, which leads the patient to death within a few minutes.
Symptoms include:
- tachycardia;
- chest pain;
- dyspnea;
- hemoptysis;
- rise in temperature;
- wet rales;
- cyanosis;
- cough;
- pleural friction noise;
- collapse.
Depending on the prevalence and combination of these symptoms, the following syndromes are distinguished:
- pulmonary-pleural syndrome: shortness of breath, chest pain (usually in the lower sections), cough sometimes with sputum. This syndrome most often occurs with small and submassive embolism, i.e. when one lobar artery or peripheral branches of the pulmonary artery are blocked;
- cardiac syndrome: pain and discomfort in the chest, tachycardia and hypotension up to collapse and fainting.
The patient may have swelling of the neck veins, a positive venous pulse, and a “loud” heartbeat. This picture is characteristic of massive pulmonary embolism.
In older people, cerebral syndrome is also observed: loss of consciousness, hemiplegia and convulsions as a result of hypoxia. These syndromes can occur in various combinations.
Risk factors
As you get older, your risk of developing chronic pulmonary hypertension increases. The disease is more often diagnosed in people aged 30 to 60 years. However, the idiopathic form is more common in young people.
Other factors that may increase the risk of pulmonary hypertension include:
- family medical history;
- excess weight;
- bleeding disorders or a family history of blood clots in the lungs;
- exposure to asbestos;
- genetic disorders, including congenital heart defects;
- life at high altitude;
- using certain drugs for weight loss;
- use of illegal and narcotic drugs;
- use of selective serotonin reuptake inhibitors, used to treat depression and anxiety.
Diagnosis of pulmonary hypertension
Pulmonary hypertension is difficult to diagnose at an early stage, so it is rarely detected during a routine physical examination. Even the symptoms of more advanced pulmonary hypertension are often similar to other heart and lung diseases.
The doctor performs a physical examination and asks questions about your medical and family history. After that, medical tests are prescribed that will help make a diagnosis of pulmonary hypertension and determine its cause. Tests for pulmonary hypertension may include:
- blood tests;
- chest x-ray;
- electrocardiogram (ECG);
- an echocardiogram (sometimes while exercising on a stationary bike or treadmill);
- right heart catheterization;
- computed tomography (CT);
- magnetic resonance imaging (MRI);
- pulmonary function test (measures how much air the lungs can hold and the flow of air into and out of the lungs);
- polysomnogram (during sleep);
- histological examination of biopsy material from an open lung;
- genetic tests (if the test result is positive, the doctor may recommend that other family members be tested as well).
Artery diseases
In the presence of diseases, obstacles appear to the transfer of venous blood to the lungs. Let's consider the main diseases of the pulmonary artery.
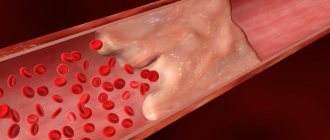
Thromboembolism
With increased formation of blood clots due to impaired blood flow and slow liquefaction of blood clots, the trunk and/or branches of the artery of the lungs may suddenly become clogged.
Pathological thromboembolism is life-threatening. It is typical:
- acute cerebral and respiratory and cardiac failure;
- ventricular fibrillation.
Eventually collapse occurs and breathing stops.
Pulmonary embolism
Thromboembolism occurs:
- massive - 50% of the vascular bed is affected;
- submassive with damage to 30-50% of the riverbed;
- non-massive with damage to the riverbed up to 30%.
It will also be useful for you to learn about the arteries that supply the brain on our website.
Patients are kept in bed during resuscitation measures. They are treated with heparin therapy and massive infusion treatment, and with the development of infarction-pneumonia - antibacterial. If necessary, thrombolectomy is used to remove the blood clot.
Embolism
In this case, the artery can become blocked with air, fat, amniotic fluid, foreign bodies, tumors, and more.
Stenosis
At the same time, the exit of the vessel from the ventricle on the right, next to the valve of the pulmonary artery, narrows. This increases the pulmonary arterial pressure difference in the right ventricle. If the pressure is exceeded, the amount of blood pushed out increases. Due to this, the following happens:
- pressure in the right atrium increases;
- hypertrophy and failure of the right ventricle begins;
- Defects develop in the septum between the atria.
Also in the article on our website you can familiarize yourself with the normal blood pressure in children by age. The table will help make this more clear.
Important. Stenosis in the exit passage of the pulmonary artery can only be eliminated surgically.
Valve insufficiency
When the valve of the pulmonary artery is affected, the symptoms will indicate a pathological condition.
Important. It is impossible to ignore attacks of shortness of breath, arrhythmia and palpitations, constant drowsiness accompanied by weakness and heart pain, persistent tachycardia. Cyanosis and hydrothorax are possible. Ascites can develop in the peritoneum and cardiac cirrhosis in the liver.
Pathologies lead to complications: aneurysm and pulmonary embolism may occur, which is life-threatening. To eliminate heart failure and prevent bacterial endocarditis, valve replacement is performed promptly.
After the operation, the patient is monitored, the composition of the blood delivered through the artery is checked, so as not to miss secondary endocarditis due to infection and degeneration of bioprostheses, since this entails re-prosthetics.
We also recommend studying this topic:
Diseases of the arteries of the lower extremities: occlusion, damage, blockage
Pulmonary hypertension
Arterial hypertension of the lungs
Arterial hypertension of the lungs develops with high pressure in the arteries of the lungs, if the resistance in the pulmonary vessel has also become higher or the volume of its blood flow has increased significantly. Primary pulmonary hypertension is fraught with vasoconstriction, hypertrophy and fibrosis.
In the artery for systolic pressure - the norm is 23-26 mm Hg. Art. (normal limit - 30 mm Hg), for diastolic - 7-9 mm Hg. Art. (upper limit limit - 15 mm Hg), average pressure norm - 12-15 mm Hg. Art.
If you experience constant fatigue with shortness of breath at the slightest exertion, discomfort in the sternum and fainting, you should measure the pressure in the arteries of the lungs and undergo a course of therapy. Dilatation agents are usually prescribed, and in difficult cases, lung transplantation is performed.
Portopulmonary hypertension
Pathology rarely develops in people with chronic liver diseases. Manifested by shortness of breath, chest pain, hemoptysis and increased loss of strength.
With the manifestation of edema, pulsation of the jugular veins, physical symptoms and changes in the ECG, we can talk about signs of cor pulmonale. Liver transplantation is not performed for this pathology, as it leads to complications and death.
Atresia
Pulmonary artery atresia indicates a lack of normal blood flow between the heart ventricles and the pulmonary artery. The cause and incidence of atresia are unknown. During the study, surgical, demographic and pathological methods and the hierarchy of heart defects are used.
Bulging of the pulmonary artery arch
Increased artery size
Patients are often diagnosed by ultrasound with an increase in the size of the artery. In this case, the pulmonary artery arch begins to bulge.
Attention! It is important to undergo a cardiovascular system check, do an ECHO-CG and an ECG. An enlarged artery and bulging of the PA arch may be a manifestation of heart disease and respiratory disease.
Bulging of the arch of the pulmonary artery more often occurs in people with mild thyrotoxicosis if they live in high and mid-altitude conditions.
If thyrotoxicosis is moderate or severe, then the cardiac waist flattens due to the bulging of the pulmonary arch, and the heart acquires a mitral configuration.
The pulmonary artery is an important vessel of the circulatory system. The normal functioning of the human body will be with effective blood flow and delivery of oxygen, nutrients, salts and hormones to the heart and other organs important for life and the removal of metabolic products from the body.
← Symptoms and treatment of right vertebral artery syndromes
Anatomy of the internal and external carotid artery →
We recommend studying similar materials:
- 1. Structure of the right and left subclavian arteries
- 2. Autoimmune hemolytic anemia in children: what is missing and how it manifests itself
- 3. How to choose a diet based on your blood type: losing weight together
- 4. The level of basophils in adults has decreased: how to treat basophilia
- 5. Functions and possible causes of pathologies of segmented neutrophils
- 6. Norms for the content of neutrophils in the blood and what functions they perform
- 7. Why does the body need bilirubin: its functions and how to get tested for the indicator
Content:
- Functional work
- Artery diseases
- Embolism
- Stenosis
- Valve insufficiency
- Pulmonary hypertension
- Portopulmonary hypertension
- Atresia
- Increased artery size
← Symptoms and treatment of right vertebral artery syndromes
Anatomy of the internal and external carotid artery →
Both branches of the artery originate from the right ventricle and have a diameter of up to 2.5 centimeters. The length of the right branch is slightly longer than the left and is 4 centimeters up to the division site. On the one hand, it departs from the trunk of the lungs at an angle between the superior vena cava and the ascending aorta, on the other hand, in front of the main bronchus on the right. Continuing the trunk of the lungs, the left branch extends to the descending aorta and left main bronchus.