With the onset of the autumn-winter season, from year to year, the circulation of non-influenza respiratory viruses (adenoviruses, respiratory syncytial viruses, parainfluenza viruses) begins in the space around us. Sporadic detection of influenza A and B viruses is also periodically observed. Many of these diseases are called colds. But in fact, there is no such disease as a cold in official medicine, but only acute respiratory infections or acute respiratory viral infections.
• What are acute respiratory infections, acute respiratory infections and acute respiratory viral infections • How to distinguish between acute respiratory infections and acute respiratory viral infections • The difference in symptoms • Modern approaches to treatment in adults • Drugs for etiotropic therapy • Drugs for antiviral therapy
What are acute respiratory infections and acute respiratory viral infections?
The term acute respiratory infections refers to a whole group of diseases that affect the respiratory system. The pathology is caused by various pathogens: protozoa, viruses, fungi, pathogenic bacteria. The diagnosis of acute respiratory infections is made when the etiology is unclear, when the doctor was unable to identify the main pathogen. In this case, mandatory laboratory examinations are indicated, on the basis of which the cause and name of the disease are clarified.
Since acute respiratory infections are caused by many infections, the disease is often acute and severe. A pronounced clinical picture is noted, the patient is worried about malaise, general weakness, runny nose, headaches and sore throat. Also prolonged fever, chills and eye sensitivity.
ARVIs are a number of pathologies that arise as a result of the penetration of various viruses into the body. Often the causative agents are adenoviruses, rhinoviruses, parainfluenza and influenza viruses. The main signs are a sore throat, runny nose, nasal congestion, high fever, weakness and headache.
A reliable way to distinguish coronavirus from other types of acute respiratory viral infections
Even experienced doctors often fail to make an unambiguous diagnosis simply by comparing the symptoms of influenza and coronavirus. In order to accurately determine the type of disease in patients, it is necessary to conduct special laboratory tests.
You can distinguish coronavirus from influenza by doing the following types of tests:
- PCR study. Produced on the direction of a doctor. The patient will only need a swab of the throat and nose; in some cases, it is possible to extract another biological fluid - blood, sputum, or rinse water from the bronchi. The resulting material is studied in laboratory conditions, and specialists look for virus cells in it. The approximate turnaround time for results is 1–3 days.
- Immunoglobulin test. Allows you to determine the presence of antibodies in the blood. It is used to clarify the current stage of COVID-19 in patients with a confirmed diagnosis, as well as to identify people who have had the disease asymptomatically.
It is extremely difficult to make a diagnosis on your own. Even the presence or absence of characteristic symptoms does not guarantee infection. Tests can also give false positive or false negative results, but their accuracy is quite high in any case. If you experience symptoms of ARVI or a cold, you should definitely consult a doctor. Only after receiving the results of the study can we speak with confidence about the presence of COVID-19 pathogens in the body and begin adequate treatment.
The difference between acute respiratory infections and acute respiratory viral infections
The main difference between acute respiratory viral infections and acute respiratory infections is the etiology of the diseases. In the first case, the causes are viruses, in the second - pathogenic bacteria, viruses and other pathogens.
The symptoms are also different. Acute respiratory diseases are characterized by a slightly high temperature, cough, runny nose, and inflammatory damage to the mucous membrane of the larynx. The development factor is hypothermia of the body. Treatment is carried out with antiviral and antibacterial agents. The duration of acute respiratory infections is at least 14 days in the absence of complications.
With ARVI, the situation is different. During the development of infection, high body temperature is recorded, up to 40 C or more. The patient complains of malaise, severe weakness and body pain. There is redness of the eyes with conjunctivitis, runny nose, and nasal congestion. Infection with pathology occurs from a specific pathogen. Therefore, treatment is targeted, antiviral drugs and symptomatic drugs are prescribed.
What diseases are there?
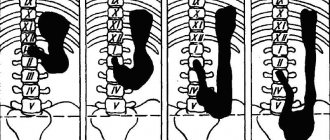
The human respiratory system is divided into upper and lower sections. The upper part is affected by chlamydial organisms, microplasmas, influenza viruses, herpes, streptococci, staphylococci, pneumococci, and Haemophilus influenzae.
Half of the infections are influenza viruses; there are mixed infections, but it is the virus that causes epidemics, complications and human death. Therefore, it is important to treat the signs of acute respiratory infections at the infection stage than to treat the consequences of non-treatment.
ARVI is difficult to treat, just like distinguishing the flu. Colds are mild.
Reasons for development
The main cause of ARVI is viral cells. Acute respiratory infections develop as a result of various infections: fungi, pathogenic bacteria, less often protozoa and parasites, and viruses.
Secondary factors provoking diseases are:
- Weak immune system.
- Nervous overstrain.
- Hypothermia of the body.
- Concomitant pathologies, including chronic forms.
- Deficiency of vitamins and minerals necessary for normal functioning.
- Poor nutrition.
- Unfavorable environment in the place of residence (dirty air, water).
History of influenza
Everything about the flu can be found in specialized literature, the media, and discussions on the street. Interesting facts about the disease have been known for a long time; the killer flu has claimed many lives on the planet. Scientists are constantly modifying and creating new vaccines, drugs, and antibiotics in the fight against the disease.
The history of influenza dates back to the time of Hippocrates, who described the first signs of the disease. Chronological sources provide a description identified by the historian T. Livy of the causes of the epidemics of 212 BC. According to assumptions, the name of the flu, like the disease, Italian fever spread to Europe and America.
Interesting facts about influenza are known in history - the English doctor D. Keyes described the disease in the 16th century and called it “sweating disease.” He saw the main reason as poor nutrition of the population and cooling down during the cold season.
In 1570, the epidemic began in Russia, spread to Europe, Africa, and several cities in Greece were destroyed. The history of the discovery of influenza is diverse; the infection spread quickly throughout the Earth.
At the beginning of the 20th century, Dr. R. Shoup, during a study of pig diseases, identified viruses, and a couple of years later, virologists identified the first pathogens, strains of the influenza virus - “A”.
Viruses mutate every year, they update and mutate. Information about the flu has been transmitted for years, frightening the population. Every 20 years, countries are affected by epidemics (Avian H5N1, swine virus A/H1N1). More than 350 people died from bird flu between 2003 and 2008. The swine virus spread to Mexico and America and killed 2,000 people between 2009 and 2011.
The whole truth about the flu is contained in the official sources of the Ministry of Health, which during outbreaks notifies the population about the mass disease and preventive measures.
Health care workers in clinics should inform patients about what they need to know about influenza, reliable information and the truth about influenza and its consequences. The main cause is type A and its subtypes, which infect humans and animals.
Symptoms of acute respiratory infections and acute respiratory viral infections
Symptoms help differentiate between acute respiratory viral infections and acute respiratory infections. However, diseases do not appear immediately. At the stage of incubation development, there are no signs. Their occurrence is observed 2-3 days after infection. Less often after a week if the person has a strong immune system.
At this time, it is recommended to undergo a medical examination so that the doctor can correctly diagnose and prescribe competent treatment tactics.
Symptoms characteristic of acute respiratory infections:
- Sneezing, runny nose.
- Weakness, malaise.
- Temperature rises to 38 C.
- Painful sensations in the throat.
- Wet cough with clear sputum.
- Diarrhea is possible.
- Watery eyes, inflammation of the mucous membranes of the eyes.
In acute respiratory viral infections, the following symptoms are observed:
- Sudden onset of illness.
- High body temperature up to 40 C or more. Lasts a long time, hard to knock off.
- Inflammatory lesion of the throat; when complications develop, a sore throat with a specific plaque occurs. The sputum changes color to green or yellow.
- Severe weakness, general malaise. Therefore, the patient often feels sleepy.
- Dry cough – at the beginning of an infection. Afterwards, sputum separation is observed, against the background of which bronchitis, tracheitis and other complicated conditions develop.
- Headache.
- Nasal congestion.
Feeling unwell, fever and sore throat, many people go to the clinic. And to the question: “What do I have, doctor?” – they may hear the answer: ARVI, ARI or ARI. Many people wonder: is this the same diagnosis? After all, the symptoms of the disease are, in most cases, the same. Then why does the doctor prescribe antiviral drugs in one case, antibiotics in the second, and a regular throat treatment in the third? And what can you take in all these cases to reduce the incidence of colds? Let's figure it out together.
What are acute respiratory viral infections, acute respiratory infections and acute respiratory infections?
ARI (acute respiratory disease) is a condition caused by an infectious-inflammatory process in the respiratory tract that occurs for a variety of reasons. The most common are hypothermia, allergies, infection and decreased immunity due to stress, lack of vitamins, untreated chronic diseases and adverse environmental factors. Various acute respiratory infections have similar development mechanisms and many common symptoms. According to localization, acute respiratory infections are usually divided into diseases of the upper and lower respiratory tract. It is important to note that the diagnosis of “ARD” is often made when the exact nature of the respiratory system disease is not known in a person.
Infectious diseases of the upper respiratory tract include rhinitis, nasopharyngitis, pharyngitis, rhinosinusitis and sinusitis, tonsillitis, otitis media, epiglottitis. Tracheitis, bronchitis and pneumonia are diseases of the lower respiratory tract. Laryngitis occupies an intermediate position. All of these diseases can be caused by viruses, bacteria, fungi and parasites. Therefore, they are combined under the general term “ARI”, or “acute respiratory infection”.
Well, the name “ARVI”, or “acute respiratory viral infection”, speaks for itself. It means that the cause of the disease is viruses, and only viruses. Based on the totality of symptoms, an experienced specialist can distinguish not only the nature of the disease, but also the suspected pathogen. Laboratory diagnostic methods further clarify the picture. Hence the “different” diagnoses with seemingly similar symptoms. It should be noted that most often the cause (90% of cases) of inflammation in the respiratory tract is still an infection.
When are you more likely to catch a cold?
Every year, with the arrival of changeable autumn and cold winter weather, we are attacked by more than 200 types of viruses: coronaviruses, adenoviruses, influenza viruses, parainfluenza, etc. With reduced immunity, each virus can become a “conductor” of a bacterial infection. A noticeable surge in colds is also observed in the spring. Why is this happening?
The maximum prevalence of ARI in the autumn-spring, as well as winter months, is most often associated with hypothermia, which contributes to the development of these diseases. High-risk groups include children, the elderly, pregnant women, and people with chronic heart and lung diseases.
The source of infection is the sick person. Transmission of infection occurs through airborne droplets, as well as through contaminated hands or objects containing pathogens of respiratory infections. Therefore, if one person in a team or family has caught a cold, the rest should also take care.
Why does my throat often hurt when I have a cold?
This symptom most often appears due to damage to the mucous membrane of the oropharynx by various viruses and bacteria. It is the mucous membrane of the respiratory tract and throat that is the “entry gate” for pathogenic agents. Under the influence of viruses and bacteria, the mucous membrane of the nasal cavity is damaged and a large amount of mucus is released, which flows from the nasal cavity down the back wall of the pharynx and causes coughing, developing and maintaining local inflammation. The mucous membrane of the throat swells, turns red, and becomes painful. A sore throat also occurs due to inflammation of the mucous membrane of the pharynx and its drying out with difficulty in nasal breathing and breathing through the mouth. Therefore, complaints about a sore throat should be taken seriously and the disease should not be left to chance.
Currently, in treatment programs for acute respiratory infections, accompanied by pain and sore throat, much attention is paid to pharmaceutical herbal remedies developed on the basis of modern technologies. A good choice is Tonzilgon® N (manufactured by Bionorica, Germany). Tonsilgon N is a combined preparation of plant origin, which includes: extracts of chamomile, marshmallow, horsetail, oak bark, dandelion, yarrow and walnut leaves. Together, these herbs have immunomodulatory, anti-inflammatory and antiseptic effects. The use of the drug is also possible as an addition to therapy with antiviral or antibacterial agents.
The role of herbal medicine Tonsilgon N in acute respiratory infections
Children and adolescents suffer from acute respiratory infections 4-5 times more often than adults. This is explained by age-related imperfections of immunity and the peculiarities of the anatomy and physiology of the child. According to many medical specialists, the unstable functioning of the immune system, which is typical for children and adolescents, can be leveled out with the help of a course of taking specially developed herbal medicines. Tonsilgon N is one of these drugs. Considering that Tonsilgon N acts as an immunocorrector on the one hand and an antiseptic on the other, it is very effective in the treatment of acute and exacerbation of chronic diseases of the upper respiratory tract. It reduces the severity of acute respiratory infections and the frequency of exacerbations of chronic tonsillopharyngitis.
Considering all the properties of the drug Tonzilgon N, it can be recommended both as an independent treatment of respiratory diseases of the upper respiratory tract, acute tonsillopharyngitis, exacerbation of chronic tonsillitis and pharyngitis in children and adults, and as part of complex therapy. Its therapeutic and preventive effect on the mucous membrane of the throat can be useful in preventing complications of acute viral infections, especially in the difficult conditions of the COVID-19 pandemic.
What is important to know about Tonsilgon N?
Tonsilgon H provides a complex effect on the mucous membrane of the upper respiratory tract. Thanks to its balanced herbal composition, it is well tolerated. Tonsilgon N is used in the treatment of acute respiratory infections, accompanied by a sore and sore throat, difficulty swallowing, and cough. The drug is convenient to use. It is available in two dosage forms: as an aqueous-alcoholic extract (drops for oral administration) and film-coated tablets. Tonsilgon N in drops is indicated for children from 2 years old, and in tablets - from 6 years old. Both forms of the drug can be taken by adults. It is important that the alcohol content in the solution ranges from 16 to 19.5% vol. (one drop of the drug contains approximately 0.008 g of pure ethyl alcohol), which is not significant in terms of the child’s body weight and does not exceed the alcohol content in one package kefir Therefore, from this point of view, the drug is safe for children. Tonsilgon N is the No. 1 drug prescribed by pediatricians among all products. It is among the TOP 10 best-selling herbal preparations in Russia. Tonsilgon N has been successfully used for more than 50 years in Germany, 20 years in Russia and 18 years in Belarus.
How to take Tonsilgon N?
The use of Tonsilgon N reduces the likelihood of complications of acute respiratory infections and the development of recurrent colds. The drug has also proven itself in the treatment of complicated ARVI. Tonsilgon N plays an important role in the treatment of frequently ill children attending preschool and school institutions. Its use is very important in the autumn-spring period, when the risk of colds increases. Dosage regimen:
| Form of the drug | How to take for children | How to take for adults |
| Drops Contraindicated for children under 2 years of age! |
|
|
| Pills Contraindicated for children under 6 years of age! |
|
|
Tonsilgon N is an excellent remedy for sore throat and sore throat, which also helps prevent complications from acute respiratory infections. Take it so you don't get sick!
Literature:
1. O. I. Pikuza, E. V. Generalova, I. I. Zakirov. Herbal medicine in the rehabilitation of adolescents with recurrent respiratory diseases. "Medical Almanac" No. 3, 2008
2. ARVI in children during a difficult epidemiological situation. Interview with Professor of the Department of Otorhinolaryngology of the Medical Institute of RUDN University, Head of the Otorhinolaryngology Center “On-Clinic”, Doctor of Medical Sciences, Irina Mikhailovna Kirichenko. "Medical Council" No. 18, 2020
3. S. O. Klyuchnikov, O. V. Zaitseva, I. M. Osmanov, A. I. Krapivkin, E. S. Keshishyan, O. V. Blinova, O. V. Bystrova. Acute respiratory diseases in children. A manual for doctors. "Russian Bulletin of Perinatology and Pediatrics", Appendix No. 3, 2008
4. A. S. Milakova, V. V. Trubnikov. Scientific supervisor – Doctor of Medical Sciences V.S. Ledneva, Ph.D. E.D. Chertok. Choice of therapy for acute respiratory diseases in children on an outpatient basis. “Russian pediatric journal” (Russian journal) No. 22(5), 2019
5. Acute respiratory infections and influenza. Prevention.
6. O. A. Malyavko. ORI. What it is?
7. Instructions for medical use of Tonsilgon N for specialists
Treatment of acute respiratory infections and acute respiratory viral infections
Since acute respiratory viral infections and acute respiratory infections are caused by different factors, their treatment is not the same.
Treatment of acute respiratory diseases is difficult. Sometimes it is difficult to identify the main pathogen. To do this, a series of medical examinations are carried out. A bacterial or viral infection of the body is often diagnosed, and based on this, etiological and symptomatic therapy is prescribed.
If the cause is pathogenic bacteria, antibacterial agents are prescribed. For a viral infection, antiviral drugs are indicated. Additionally, antipyretic, expectorant, and vasoconstrictor medications are prescribed. Also aerosols, nasal drops, vitamins, plenty of warm drinks and bed rest.
It is forbidden to treat ARVI on your own for more than 3 days. In this case, the risk of complications increases. You need to see a doctor. Patients are prescribed a course of antiviral therapy. To relieve symptoms, anti-inflammatory, antihistamine, and antipyretic drugs are prescribed. It is useful to gargle with decoctions of medicinal plants. Navizin and Pinosol are used for a runny nose. For pain and high fever, Paracetamol and Ibuprofen are prescribed. ACC, Mucaltin and other expectorants are effective for treating cough.
It is important to maintain rest, bed rest, drink more fluids and take vitamin complexes.
Note!
It is very important to pay attention to several points when purchasing a drug.
Firstly, this is the quality of medicines. European manufacturers working according to the GMP standard guarantee the quality and safety of medicines. GMP (Good Manufacturing Practice) is a standard applied to the production of medicines. Guarantees high quality products, which is achieved through careful control over the production process at all stages from the production of components to packaging of the finished product.
Secondly, it is necessary to carefully study the composition of the complex product. There are medicines that contain a huge number of components, but this does not guarantee fast and better treatment. Some components may be incompatible with each other or should not be taken by children. For example, due to the toxicity of rimantadine (found in some flu medications), the benefits of taking it are much less than the possible negative consequences. You should also remember that children should not be given aspirin, as it weakens the walls of blood vessels.
Another important rule that you need to know is that you should not try to treat the flu with antibiotics and antiviral drugs without a doctor’s prescription. Remember that antibiotics only kill bacteria and are not effective against viral infections. Sometimes the doctor prescribes antibiotics for the flu, but only if complications caused by bacteria (inflammation of the lungs, middle ear or paranasal sinuses) have arisen during the illness. And it is important to remember that treatment for colds and flu should always be correct!
Author: Anna Orekhova
Flu prevention
The best measure is to prevent infection, infection. It is necessary to strengthen the immune system year-round by consuming vitamins, excluding bad habits and contact with sick people. If necessary, during epidemics, do not visit places with large crowds of people (cafes, hospitals, entertainment and shopping centers).
Prevention measures:
- Vaccination.
- Hardening.
- Doing physical exercises and exercises.
- Balanced, proper nutrition.
- Lubricating the nasal passages with oxolinic ointment, interferon, and Vaseline.
- Maintain hand hygiene.
- Use of individual utensils.
- Regular ventilation of the room.
The correct drinking balance removes unnecessary substances from the body and helps eliminate infection. The best prevention of the disease is vaccination. The flu shot is given every year.