general description
Gastroptosis is the prolapse of the stomach, which is accompanied by hypotension and elongation.
Most often, the disease is registered in women 16-50 years old. In the early stages it is asymptomatic. Then, as gastroptosis progresses, the patient begins to experience abdominal pain after eating or exercising.
In addition, advanced forms of the disease lead to prolapse of other internal organs with the appearance of corresponding symptoms. The main methods of treating gastroptosis are physiotherapy and exercise therapy.
Causes of gastroptosis
The reasons for the development of primary gastroptosis are:
- bend of the upper part of the duodenum;
- body features (tall, elongated limbs and fingers on them, thinness, long neck, narrow sternum, weak muscles);
- bowel prolapse.
The secondary form of the disease occurs against the background of the following conditions of the body:
- sudden weight loss;
- surgical intervention for the treatment of ascites;
- hypovitaminosis;
- undergone surgery to remove stomach tumors;
- poor nutrition, lack of protein in the diet;
- frequent childbirth;
- lung diseases that lead to prolapse of the diaphragm;
- Regular weight lifting, weightlifting and other strength sports.
Kinds
There are two types of illness:
- Congenital, also called constitutional. This congenital pathology is due to the peculiarities of the morphological structure of the human body. An asthenic physique is characterized by a disproportionate structure: the chest and shoulders are narrowed, and the body itself is elongated.
- Acquired – caused by weakening and stretching of the gastric ligaments. It can occur after childbirth, surgery, or after sudden weight loss.
Regarding the distribution in the intestine, it happens:
- partial – accompanied by muscle lengthening and low peristalsis;
- total – accompanied by numerous pathological changes in other internal organs.
There are 3 stages of prolapse, each of which is determined by the distance between the lower border of the stomach and the pectineal line:
- first - the intestine is 2 or more centimeters above the pectineal line;
- second - they are on the same level;
- the third is visible omission.
Symptoms of prolapsed stomach
The clinical picture largely depends on the severity of the disease. There are 3 degrees of gastroptosis, depending on the position of the upper concave edge of the stomach (above, at the level or below the line of the gallbladder).
| Stages of gastroptosis |
At the first and second stages, signs of gastroptosis are not expressed. The patient may complain of the periodic occurrence of the following symptoms:
- a feeling of heaviness in the upper abdomen, which intensifies after eating;
- frequent constipation, flatulence;
- heartburn;
- aversion to dairy products;
- nausea;
- change in gastronomic preferences.
At the third stage of the disease, pronounced symptoms appear:
- acute pain in the epigastric region, which intensifies with movement and decreases at rest;
- burping “rotten”;
- autonomic disorders: dizziness, tachycardia, increased irritability, hyperhidrosis;
- constipation, which is replaced by diarrhea;
- hypovitaminosis.
Diagnosis
G.'s diagnosis in the past was made often and in most cases unfoundedly; however, the often observed opposite tendency to consider G. as a variant of functional gastric dyspepsia [Marzhatka (Z. Maratka), 1967] also cannot be recognized.
When rentgenol, the study reveals a vertically elongated stomach, the convergence of its greater and lesser curvature; the anthralopyloric part, and especially the lower pole of the stomach, is lowered, in some cases it goes into the pelvis.
Diagnosis of gastroptosis
The main methods for diagnosing the disease are:
- collecting anamnesis, interviewing the patient;
- external examination - the doctor notices a slightly saggy lower abdomen;
- Ultrasound;
- esophagogastroduodenoscopy;
- electrogastrography;
- radiography using a contrast agent.
| Gastroptosis: X-ray |
Concept
According to what is written in the Encyclopedic Dictionary of Medical Terms, “Gastroptosis (gastro- + Greek ptosis, fall, prolapse) is a pathological downward displacement of the stomach; develops, for example, as a result of a sharp weakening of the muscles of the abdominal wall, with significant weight loss, after extraction of ascitic fluid.”
Splanchnoptosis is often associated with gastroptosis (see below), which, in general, is quite understandable, because, in particular, the large intestine is fixed to the stomach by the gastrocolic ligament (lig. gastrocolicum), its fibers connect the greater curvature with the transverse colon gut. The stomach descends, and the transverse colon also descends.
Treatment of gastroptosis
Therapy for the disease is complex and includes several stages.
Diet
The diet for gastroptosis includes easily digestible foods. You need to eat at the same time, in small portions (5-6 times a day, in small portions). After eating, you need to take a horizontal position for at least half an hour.
If the patient has a decreased appetite, then taking foods with a choleretic effect is indicated. If you have constipation, you need to eat more foods rich in plant fiber.
| List of foods allowed for gastroptosis | List of foods prohibited for gastroptosis | ||
| oatmeal/buckwheat porridge with water | semolina porridge, rice | ||
| vegetables and fruits | fatty, spicy, salty | ||
| dairy products | marinades, smoked meats, pickles | ||
| boiled dietary meat and fish | fresh bread, sweet products | ||
| low-fat broth | coffee, cocoa | ||
| compote, weak tea, juice | carbonated, alcoholic drinks | ||
Exercises for prolapsed stomach
All patients diagnosed with gastroptosis are prescribed courses of physical therapy. The attending physician selects exercises based on the severity of the disease, age and individual characteristics of the patient’s body.
Perform the exercises in a lying position, legs should be slightly elevated. The main load should fall on the abdominal cavity and legs. The patient needs to lift and bend his legs at different angles while lying down.
The training is completed with an abdominal massage, after which the patient should spend some time at rest.
| Exercises for prolapsed stomach |
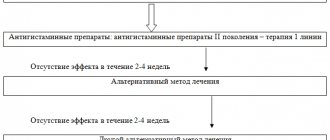
Drug therapy
Treatment of gastric prolapse with drugs is prescribed at the third stage of the disease. Therapy is symptomatic and includes taking the following groups of medications:
- antispasmodics - to relieve cramps and abdominal pain;
- sedatives - to relieve or reduce autonomic disorders;
- enzyme preparations - indicated for disturbances in the production of gastric juice.
Surgery
It is rarely used for prolapsed stomach; surgery is usually performed if frequent relapses of gastroptosis occur. In addition, surgical intervention may be prescribed if massages, exercise therapy, diet and medications do not produce results, and the patient’s condition continues to deteriorate.
Author's technique of modified fundoplication
During the operation, I use a Toupet partial fundoplication of 270 degrees, in which a cuff is created from the stomach wall to prevent the reflux of stomach contents into the esophagus. Thanks to the improved technique, for which a patent has been received, the functioning of the sphincter between the stomach and esophagus remains undisturbed, while the gag reflex and belching - protective functions - are also preserved.
The surgical intervention is performed using laparoscopy, using high-quality endoscopic equipment, which allows all manipulations to be performed with maximum precision, without the risk of damaging the structures located in this area: vessels, fascial spaces, vagus nerve. During laparoscopic surgery, I create a functional valve between the stomach and esophagus, which allows the patient to do without medications in the future. Due to the fact that all manipulations are performed through 3-4 small incisions, an excellent cosmetic result is guaranteed, since after healing, the marks from the incisions will become almost invisible.
When isolating the stomach and esophagus, I use the LigaSure device for dosed electrothermal tissue ligation, thanks to which the vessels can be “sealed” without damaging the surrounding tissues. The use of the latest generation of absorbable suture material and anti-adhesion barriers allows the operation to be performed quickly and efficiently.
If there are several diseases that require surgical treatment, in our clinic the patient can count on a simultaneous operation. Instead of several interventions, the interval between which should be 5-6 weeks, the person being operated on during one anesthesia can immediately get rid of a number of diseases.
Patients are discharged, as a rule, on days 1-3, and after 2-3 weeks they return to their usual activities. For the first two months you will have to adhere to a strict diet; over the next six months, the diet will gradually expand. In the future, a person who has undergone treatment in our clinic will be able to do without medications and without following a strict diet. We managed to reduce the number of relapses during the first year to 2%; five years after the operation, this figure does not exceed 4%.
I have performed more than 2000 operations on the stomach and esophagus, the accumulated experience is summarized in three monographs and more than 50 scientific publications, which can be found in professional peer-reviewed publications published in our country and abroad.
Gastroptosis prognosis
With timely treatment, the prognosis is favorable. If therapy for gastroptosis is not carried out, the disease continues to progress, the stomach begins to put pressure on the intestines, which also shifts and begins to put pressure on the prostate in men, the uterus in women, which leads to the appearance of new unpleasant symptoms and a further deterioration in the patient’s quality of life.
In addition, the consequences of gastroptosis can be:
- weakening of the motor and secretory functions of the stomach;
- slowing down the movement of the food coma through the gastrointestinal tract;
- development of stomach and intestinal cancer.
Complications
The result of aggressive contents entering the esophagus can be damage to the esophageal mucosa; due to regular exposure to an aggressive environment, an inflammatory process develops, which leads to the appearance of reflux esophagitis - inflammation of the lower parts of the esophagus. If left untreated, an ulcer may form - damage to the esophageal wall down to the submucosal layer. In severe cases there is a risk of bleeding. After the ulcer has healed, scars may remain that can cause stricture. The result of deterioration in the patency of the esophagus will be dysphagia in combination with heartburn, which only aggravates the situation.
One of the severe complications is Barrett's esophagus syndrome, in which the squamous cell epithelium in the esophagus is replaced by columnar gastric epithelium - metaplasia, and the likelihood of degeneration into cancer increases by 30-40 times.
Prevention of gastroptosis
The main measures to prevent the disease are:
- if you have low body weight, visit a nutritionist and develop a diet that will help you gain the required weight;
- giving up a sedentary lifestyle - regular walks in the fresh air, physical exercise;
- normalization of diet;
- refusal of heavy physical labor;
- Women's use of contraceptives - too frequent childbirth can lead to the development of gastroptosis.
Good health to you!
Lack of awareness
Not every actively practicing physician will immediately agree that in 70% of gastroenterological patients with symptoms of “gastric dyspepsia” or “functional dyspepsia,” no significant pathological signs can be found during endoscopic examination of the upper gastrointestinal tract. Nevertheless, this is an established fact, albeit from Western sources. Hand on heart, we could give us a similar figure, but the logic is brought down by the fact that almost all such patients have dyspepsia, but in the absence of significant visual changes, we prescribe antiulcer treatment, and even eradication therapy (if there is a hint for H. pylori
) .
However, somehow I can’t bear to accept the tactics of blanket treatment for ulcers, when there is not even gastritis...
What is the problem and ways to solve the problem at least in some cases?
Firstly, it is necessary to remember that there is a whole list of diseases that fall under the category of “functional disorders”. With them, no matter how hard we try, we cannot identify any morphological signs that could provide grounds for a specific diagnosis such as “peptic ulcer” or something like that.
However, there is a “second thing”. I dare to assure my colleagues that not all, but many patients who complain of very painful “gastric” symptoms, have the latter caused by gastroptosis. Not recognizing the first or second means dooming a person to a waste of time, money, health, visiting doctors and research. Quite often we see patients who, indeed, losing a lot of strength and resources, walk in circles without any prospect of improvement, because therapeutic measures can have serious success only when the true cause of suffering is accurately established.
Apparently, in the West they also don’t think too much about gastroptosis, and all patients of this kind end up in one cohort, which is called “functional dyspepsia.”
List of sources
- Stepanov N.P., Ivanov A.I., Tobokhov A.V., Nikolaev V.N., Sleptsov V.D. “Diagnostics and surgical correction of gastroptosis”, article in the journal “Clinical Medicine”
- Shulgai A.M., Kabakova A.B., Klim L.A., Glushko K.T. “The problem of gastroptosis as a manifestation of undifferentiated connective tissue dysplasia in the practice of a pediatric gastroenterologist,” article in the journal “Clinical Medicine”
- Plechev V.V., Latypov R.Z. “Pancreatobiliary complications in gastroptosis”, article in the journal “Clinical Medicine”
Etiology and pathogenesis
When reading the literature, one gets the impression that the issue of the etiology and pathogenesis of gastro- and splanchnoptosis is discussed little. More precisely, they talk about the reason, but somehow in passing and in the same way, so let’s take part in the discussion.
Previously, a definition was given from the Encyclopedic Dictionary of Medical Terms, which indicates the origin of gastroptosis. However, the definition is clearly limited: “... develops, for example, as a result of a sharp weakening of the muscles of the abdominal wall, with significant weight loss, after extraction of ascitic fluid.”
A large number of patients with proven gastroptosis and the clinical picture associated with it passed through without a hint of ascites; more precisely, from this cohort there was not a single patient with ascites. Many of the examined patients not only are not distinguished by “sharp weakening of the abdominal wall muscles”, on the contrary, they are quite physically developed and are involved in fitness. Although it must be admitted that almost all patients with gastroptosis were thin. Yes, lack of fat in the abdominal cavity, mainly in the mesentery, is one of the factors associated with gastric prolapse. Nevertheless, in first place I would put not the weakening of the anterior abdominal wall and thinness, but primary mesenchymal insufficiency, i.e. genetic defects and connective tissue deficiency.
Mesenchymal failure is a separate issue. When applied to gastroptosis, it is important that this condition is associated with weakness of connective tissue structures. Patients have hypermobility of the joints, some elongation of the limbs (in particular the fingers), flat feet, and certain manifestations of dysmorphism (high palate, altered bite, scoliosis, etc.), although there is no talk of obvious marfanism.
It is reasonable to put mesenchymal failure in first place. Therefore, in the diagnosis of gastroptosis, a very important point is the first glance at the patient. A typical patient is tall, thin, with fingers longer than those of the doctor (if the height is comparable, you can put “palm to palm”). Further examination usually reveals other manifestations: the patient easily brings his thumb to his forearm, clasps his hands behind his back between the shoulder blades, reaches the floor with his entire palm when bending over, etc.
Noteworthy are longitudinal and transverse flat feet, scoliosis, and sometimes funnel chest deformity. By the way, in most of the photographs presented, scoliosis of the spine is clearly visible. This is far from an accident: scoliosis is one of the typical manifestations of congenital mesenchymal deficiency.
I consider mesenchymal deficiency (congenital deficiency of connective tissue) to be the main cause of gastro- and splanchnoptosis.
In this regard, one cannot help but express great doubt that gastroptosis can occur after pumping out ascites or as a result of any other “weakening of the anterior abdominal wall.” I would be grateful if someone could explain why a person should develop gastroptosis due to ascites if there was no gastroptosis before the accumulation of transudate in the abdominal cavity began. In my opinion, formed and pumped out ascites cannot provoke gastroptosis, i.e. Lengthening the ligaments of the stomach: it is not so easy to make the ligaments several times longer. Moreover, in ascitic fluid the organs are weightless, and the gas-containing colon apparently also acquires additional buoyancy. At the moment of fluid removal, even having lost support from the flabby anterior abdominal wall, the gastric ligaments will not suddenly stretch.
The idea creeps in that the position that “flabby anterior abdominal wall” is associated with gastroptosis or is its main cause is simply thoughtlessly copied from one work to another and has even been introduced into the definition printed in the “Encyclopedic Dictionary of Medical Terms.”
However, the truly real cause of gastroptosis should be recognized as long-term gastroparesis or mechanical obstruction at the level of the outlet of the stomach or duodenum, but again, most likely, only in the presence of congenital mesenchymal failure. In this case, prolapse of the stomach is possible as a result of constant overfilling of the organ, as is observed in the patient whose photograph is presented in Fig. 10. Her connective tissue is also clearly defective - this is indicated by scoliosis. The stomach is hypotonic, without peristalsis, distended with a huge amount of contents (the contrast study was done without any preparation).
Relevance of the problem
The relevance of the problem can only be judged on the basis of personal experience. And so it turns out: if you show one of your colleagues a patient with pronounced gastroptosis, you see two types of reactions: either true interest and surprise that this is possible; or skepticism and denial of significance. Let’s discard the last option as, to put it mildly, shallow and counterproductive.
Counterproductive, also because the doctor loses the chance to see the bright emotions of the patient, who, looking at her own x-rays, expresses genuine amazement. The effect is enhanced if you first show her what the normal topography of the organ looks like using a picture in a book or the Internet.
Emotions are emotions, but the main thing, of course, is the medical aspects - the ability to identify the anatomical and physiological features to explain the symptoms of the patient. Sometimes, after looking at the picture, a person himself comes to the solution to a clinical puzzle, for example, one patient exclaimed: “So that’s why after eating my lower abdomen becomes enlarged, as if from a baby!” Indeed, in her case, the contrasted stomach – without the slightest exaggeration – “lay on the uterus” with its lower pole.
In order to facilitate the demonstration of visual material, you will have to slightly change the usual order of presentation of the clinical topic, starting from the middle.
Epidemiology, prevalence
With all this, it is pointless to judge the frequency and prevalence of gastroptosis based on literary data, since, firstly, gastroptosis as a cause of human suffering is rarely considered at all: few colleagues come up with the idea of identifying gastric prolapse. If not identified, it means there is no problem. In short, ignorance is the main obstacle.
On the other hand, not all gastroptoses cause symptoms. Naturally, no one will set themselves the task of identifying a disease that, in fact, does not exist. Yes, and there is no particular need to identify asymptomatic gastroptosis.
The third aspect is quite common: there are many patients with pronounced prolapse of the stomach, who have symptoms and happily don’t care about the discomfort - maybe it will go away on its own.