Symptoms
Signs of uterine prolapse consist of dysfunction of those organs that are involved in the pathological process. The displacement of the uterus itself causes:
- feeling of a foreign body in the vagina
- discomfort during sexual activity
- pulling sensations in the lower abdomen.
It is important to remember the fact that the uterus lies at the apex of the vagina, so its prolapse is inevitably accompanied by prolapse of the anterior/posterior wall of the vagina, and therefore the bladder/rectum.
This is why patients with “prolapse of the uterus” complain:
- for urinary disorders (difficulty urinating, a feeling of incomplete emptying of the bladder, frequent urination, loss of urine when straining or against the background of a strong urge, etc.)
- for problems with defecation (difficulty defecating, defecation in portions, the need to reduce prolapse to completely empty the bowel, etc.).
| anonymously to the doctor, through the feedback form, we will try to help you. | Ask a Question |
What to do if the uterus prolapses?
I am 55 years old. I want to tell my story, I will be glad if it helps at least one person maintain their health, and maybe even their life.
I contacted the state gynecology department about genital prolapse, they gave me a referral for surgery and a list of necessary examinations, and the doctor told me how the operation would proceed. Arriving home, I decided to consult the Internet - it turned out that after such operations there is often a perforation of the urinary and rectal intestines and other complications. I decided to find out if there were other methods for such operations, and as a result I ended up on the website of the Swiss University Clinic, where the method developed by Professor Konstantin Viktorovich Puchkov was described. In order not to rely only on my intuition, which suggested that this was what I needed, I talked with gynecologists I knew, some did not even know that such a technique existed, but everyone confirmed that this was the best solution.
At the appointment, the professor explained in detail how the operation would take place, they gave me a list of examinations, which included an examination of the bladder (which I really liked, because in case of problems, they will also be corrected during the operation), and a colonoscopy (which I really did not like). I liked it because three years ago I was examined by a proctologist - they did not find any pathology, especially since in the state hospital this examination was not required for the operation - which means it is not necessary). I started taking all the tests, and decided to do the colonoscopy last, in the hope that I would still be able to somehow manage without it. But Konstantin Viktorovich was adamant, for which I am now very grateful to him, because during the examination it turned out that I had stage 2 sigmoid colon cancer. I underwent the necessary additional examinations (biopsy, CT, MRI, Holter) in the clinic in two days (at the state clinic the biopsy is ready only after 10 days), and already on the fourth day after I learned about the diagnosis, laparoscopic surgery was performed. On the 5th day after the operation I was at home. After the operation, she underwent 6 courses of chemotherapy. Yesterday I received the CT results, so far everything is fine. I really hope that the result of the treatment will be positive and, thanks to Konstantin Viktorovich, I will live a full life. Now it’s even scary to think how it would have ended if I hadn’t ended up in this clinic.
I cannot help but say a word of gratitude to the doctors who fought my illness.
Communication with anesthesiologist Igor Borisovich Kholodov before the operation was short, but it instilled calm and confidence in the professionalism of this person.
Professor Serebryansky Yuri Evstafievich is very attentive, takes his duties very seriously, thoroughly examined everything that raised doubts so that there were no unpleasant surprises during the operation, he will always support and give the necessary advice.
My attending physician is Evstratov Roman Mikhailovich, who accompanied my “chemistry” for three months, to whom I can turn for help at any time if problems arise or any questions arise.
I don’t want to single out anyone from the rest of the clinic staff, because it’s impossible - everyone is attentive, conscientious, always comes when called, will ask you ten times how you are feeling, if you need anything, and surround you with care, attention, and sympathy.
And, of course, the most important person is Konstantin Viktorovich Puchkov, who insisted on this unpleasant colonoscopy procedure and undertook to perform the operation using the laparoscopic method, thereby prolonging my life and saving me from the terrible torment that awaited me if the diagnosis had not been made in time .
I am infinitely grateful to you, Konstantin Viktorovich, for your responsible and conscientious approach to preoperative examinations and for your wonderful talent as a surgeon! Health and happiness to you!
Causes
The causes of uterine prolapse can be described according to the life course model. At the beginning, a person has one or another predisposition to the development of this pathology. Then various aggressive factors begin to act on it, which lead to the onset of the disease. At the first stage, the body copes with the damage that has arisen, but age and the accumulation of damage leads to its manifestation and, in fact, to the complaints that were described above. All pathological factors can be divided into the following:
- Heredity. It has been proven that if close relatives have the disease, the likelihood of occurrence increases several times. Most often, there is a congenital weakness of the connective tissue, which affects other systems of the body, manifesting itself in diseases of the musculoskeletal system, varicose veins, and hemorrhoids. However, heredity is still not a death sentence, and what makes it a reality are the risk factors, which will be discussed below.
- Childbirth and pregnancy. Perhaps the main factor that leads to changes in the qualitative composition of the supporting apparatus of the pelvic floor and its partial damage. Unfortunately, with severe tissue failure, complete prolapse of the uterus can develop immediately after childbirth. On the other hand, for most women in labor, the prolapse completely regresses within the first year.
- Increased loads. And this is not only hard physical labor, but also chronic constipation, lung diseases accompanied by a constant and severe cough, and obesity. All these factors lead to damage to the ligamentous apparatus of the pelvic organs and their prolapse.
- Age. This factor has a complex effect on all supporting structures of the pelvic floor. Firstly, with age, hormonal levels change, and with it the quality of connective tissue (it becomes looser and weaker). In some patients, hormonal changes lead to deformation and changes in the cervix, such as its elongation and hypertrophy. Secondly, muscle tone decreases, including that of the pelvic floor. In this regard, injuries to the ligamentous apparatus once received lose their support and become obvious.
Prevention
Preventive measures are simple and understandable for any woman, regardless of her age and stage of development of the disease. Hormones
- Contact specialists in a timely manner. Any consultation will not be superfluous for a woman.
- Consider switching births that may result in trauma to a caesarean section.
- Use hormone replacement therapy for menopause or estrogen deficiency.
- Perform special sets of exercises to strengthen the pelvic muscles.
- If the integrity of the perineum is compromised, try to restore it completely, and not just the outer integument.
Diagnostics
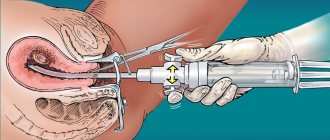
Diagnosis of uterine prolapse does not raise questions among specialists. To do this, it is necessary to conduct a standard gynecological examination, on the basis of which the stage of prolapse is set and the part of the vagina involved in the pathological process is determined.
Most often, damage occurs to all three sections of the pelvic floor: anterior, posterior and apical.
In total, there are four degrees of uterine prolapse: the first (initial), when the patient is practically not bothered by anything, the fourth degree is accompanied by complete prolapse of the pelvic organs.
The study can be supplemented with a digital rectal examination to exclude rectal prolapse.
As instrumental methods, ultrasound of the pelvic organs and sometimes MRI are performed.
| Most patients receive care for free (without hidden additional payments for “network”, etc.) as part of compulsory health insurance ( under the compulsory medical insurance policy ). | Application for treatment under compulsory medical insurance |
What to do in advanced cases
In this case, the walls of the vagina descend so much that the pelvic organs and even the abdominal cavity are displaced into the genital tract. Prolapse of the cervix and its body is often observed. Grade 3-4 prolapse requires only surgical treatment.
With advanced prolapse of the vaginal walls, the following may occur:
- Cystocele is prolapse of the bladder. Occurs when the anterior wall subsides.
- Rectocele is prolapse of the rectum. Occurs when the posterior wall subsides.
- Enterocele is prolapse of loops of the small intestine. Occurs when the upper-posterior part of the vaginal wall prolapses.
Cystocele, rectocele, enterocele
To eliminate this condition, colporrhaphy is performed, which can be:
- Anterior – correction of sagging anterior vaginal wall and bladder prolapse.
- Posterior – treatment of prolapse of the posterior wall with the return of intestinal elements to their place.
- Combined or complete. In this case, both walls of the vagina are tightened, and all displaced organs return to their correct position.
Treatment
Treatment of uterine prolapse includes surgical and conservative treatment methods.
Conservative methods include:
- Kegel exercises for uterine prolapse are aimed at increasing the tone of the pelvic floor muscles. Due to this, the damaged ligamentous apparatus has a foundation that prevents the pelvic organs from descending excessively. Unfortunately, it is quite difficult to perform these exercises correctly, since it is difficult to train something that you cannot see and do not control. To solve this issue, biofeedback devices (BFB therapy) were developed, which increases the effectiveness of exercises several times. This method will be useful for young patients and women after childbirth.
- Pessaries and bandages are aimed at creating an obstruction in the path of descending organs. When the uterus prolapses, the pessary is placed in the vagina and serves as a kind of spacer. Unfortunately, the presence of a foreign body inside often causes discomfort, chronic inflammation and, most importantly, requires regular visits to the gynecologist to change it. In the case of bandages, they are simply tight underwear that prevents prolapse from leaving the vagina. Sometimes it is combined with a pessary and works like a “plug”. These methods can be used if the operation cannot be performed for some reason. This can be compared to a crutch for a limb injury.
Patient reviews
Reviews from women who have undergone various procedures for treating uterine prolapse confirm the need to use a set of various measures.
- Galina: After surgery, I prepared a tincture from eggshells. The mixture consisted of shells and lemon, infused with regular vodka. Daily use relieved all post-operative unpleasant symptoms.
- Marina: Treatment required surgery. But in the postoperative period, herbal baths, decoctions and mixtures helped.
- Olga: uterine prolapse is an insidious disease. Few people manage to identify it in the initial stages. It turns out that I had it, but I didn’t even know about it, since there were no manifestations. The doctor diagnosed it during an examination. Did Kegel exercises. I believe that this is the most effective way to treat the disease. This, of course, only with minor prolapse.
- Lyudmila: During treatment I performed only two exercises. I did them before going to bed, lying in bed. Before the exercises, I carried out rubbings prepared from various medicinal herbs, honey and oak bark.
Operation
The main method of treatment is still surgical, since the supporting apparatus of the pelvis is not restored. Unfortunately, the most popular method, removal of the uterus, often does not help, since not only the uterus, but the pelvic organs (bladder, rectum) prolapse.
For this reason, this approach leads in 30-50% of cases to the development of prolapse of the vaginal stump.
Another problem with hysterectomy is posthysterectomy syndrome, which leads to impaired urination, defecation and decreased sexual function, including due to postoperative shortening of the vagina. Reconstructive operations performed through the vagina seem to be the most optimal and proven. On the one hand, they allow you to achieve a good anatomical result, on the other, a good cosmetic effect. One of the most modern techniques are hybrid operations, which allow the operation to be individualized for each specific patient, while maximizing the use of his own tissues, and, if necessary, supplementing them with a prosthesis only in the busiest places.
Pathogenesis of the disease
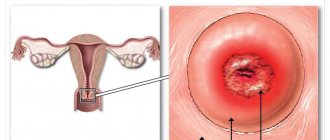
In a healthy person, the uterus is located above the vagina in the pelvic cavity. Anterior to it are the bladder and urethra, posteriorly the rectum. This position helps the organs to be supported by powerful muscles and ligaments of the pelvis. The complex of these structures is otherwise called the pelvic floor. The normal anatomy of the pelvic organs is shown in the diagram below:
When the pelvic floor weakens, the topography of the pelvic organs changes, they move downwards under the force of the earth's extension. The reason for this may be factors related to lifestyle and work activity. Women who have given birth most often get sick. Any reason leading to an increase in intra-abdominal pressure leads to weakening of the muscles and ligaments of the pelvis. This could be a simple cough that lasts for a long time, or sneezing.
Weakening of the muscles and ligaments of the uterus leads to its descent. She begins to pass through the vaginal canal, “crushing” the vagina in front of her. Depending on the anatomical level of the uterus, there are several degrees of prolapse, the last of which is prolapse. Schematically, uterine prolapse looks like this: