Beautiful skin is first and foremost healthy skin. In order for your face to shine, you need proper nutrition, care and immunity support, incl. local, at the proper level. If acne appears on the face, especially in adulthood, the immune system cannot cope, it needs support. One of the most effective means is autohemotherapy. These are injections of the patient’s own blood, which help activate metabolic processes, strengthen the immune system and reduce inflammation.
How does the procedure work?
Previously, cosmetologists did subcutaneous injections. This made it possible to achieve the desired result, but there was a side effect in the form of hematomas. Injections began to be given intramuscularly. After them, no traces remain on the face, and the effect remains.
The procedure goes like this: blood is taken from a vein from the patient and injected into the muscles, usually the buttocks, on the opposite side. So, if blood was taken from the right arm, then an intramuscular injection is made to the left side. The course starts with 2 ml. and continue increasing with a factor of 2. The procedure is carried out every other day for 10 days, sometimes more.
Introduction
Despite the achievements of modern medicine, uncompensated blood loss remains the leading cause of death in patients with abdominal trauma [1, 11, 15, 16]. The tactics for compensating blood loss are to immediately stop bleeding, replace the volume of circulating blood and oxygen transport.
3-5% of patients with ongoing bleeding who require emergency intervention require massive blood transfusion [9, 10, 12, 13, 16]. The negative consequences of massive transfusion of allogeneic blood are well known [8-11, 13, 14, 16]. Note that massive blood transfusion also stimulates a systemic inflammatory response and significantly increases the incidence of purulent-septic complications in the postoperative period. The need for donor blood components makes it possible to reduce alternative methods, especially in situations in which it is impossible to refuse or limit blood transfusion [8, 10]. The use of autologous blood components is a common and safe alternative to donor blood, which has become widespread in elective surgery. In emergency surgery, when preoperative preparation is impossible, this problem can be solved by intraoperative reinfusion of spilled blood with Cell Saver devices [1-7, 8, 10]. Despite the existing positive experience, the methodological basis and material and technical equipment of hospitals limit the use of this method in emergency surgery.
The purpose of the study is to compare the effectiveness of intraoperative transfusion of donor and own red blood cells in patients with diseases and injuries accompanied by blood loss of more than 70% of the circulating blood volume.
Material and methods
A retrospective analysis of the course of anesthesia and the results of treatment of 91 patients with injuries and diseases complicated by intra-abdominal bleeding in a volume of more than 4 liters was carried out (Table 1).
All patients were operated on as an emergency to stop bleeding. Anesthesia was standard (ketamine, fentanyl, Nimbex in recommended doses). Artificial ventilation of the lungs was carried out in the normal ventilation mode with an air-oxygen mixture (FiO2 1.0). Intraoperative infusion-transfusion therapy (ITT) included colloid and crystalloid media, fresh frozen plasma, donor erythrocytes (DE) and autoerythrocytes (AE), obtained using intraoperative hardware reinfusion of shed blood on a continuous autotransfusion system CATS (Fresenius). ITT tactics were based on determining the volume of blood loss and differed at the stages of surgical intervention. Before stopping bleeding, solutions were predominantly used under the control of hemodynamic parameters (ratio of colloids to crystalloids 2:1). The indication for DE transfusion before bleeding stopped was a hemoglobin level of less than 90 g/l. To support hemodynamics when a high infusion rate was ineffective, sympathomimetics were prescribed (dopamine at a dose of 2 mcg/kg min, adrenaline at a dose of 0.1 mcg/kg min). Lost red blood cells and blood coagulation factors were compensated during bleeding control, continuing after surgical hemostasis was achieved. Correction of electrolyte disturbances and metabolic disorders was carried out throughout the intervention.
Depending on the transfusion media used, all patients were divided into 2 groups. Group 1 included 14 patients (9 men and 5 women), in whom DE was predominantly used (more than 60% of the total volume of blood transfusion). The severity of the injury on the ISS scale was 54.5±3.4 points. The average age of patients was 47±4.9 years. Globular volume deficit 55.9±4.1%. The 2nd group included 77 people (73 men and 4 women), in whom AEs returned using hardware reinfusion were predominantly used (more than 60% of the total volume of blood transfusion). The severity of the injury on the ISS scale was 44.1±3.2 points. The average age of patients was 43±2.1 years. Red blood cell deficiency 56.9±1.9%. In terms of age, severity of injury, volume of recorded blood loss, and red blood cell deficiency, the differences in the groups were statistically insignificant.
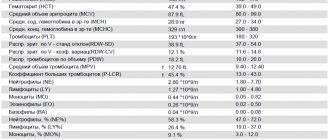
The immediate results of intraoperative blood transfusion were assessed by indicators of red blood (Hb, Ht), oxygen content in arterial (CaO2) and mixed venous (CvO2) blood, hemoglobin saturation in mixed venous blood with oxygen (SvO2), tissue oxygen extraction ratio (O2ER) and the dynamics of the content lactate (Lac). Mortality was analyzed - in-hospital, intraoperative and postoperative.
Statistical processing of the material was carried out using the statistical package IBM SPSS Statistics 19 (IBM Inc., USA). The average values (M), standard deviation (σ), and standard error of the mean (s) were determined. For intergroup comparison, the Mann-Whitney, Kruskal-Wallis, Friedman, and Wilcoxon tests were used. The relationship between variables was determined using the test (χ2), odds ratio (OR), Pearson correlation coefficient (R), Kendall (τ) and Spearman (ρ). Data are presented as M±s. P=0.05 was taken as the threshold level of statistical significance.
Results and discussion
In group 1, during the operation (182±19 minutes), 9503±1056 ml of infusion and transfusion media were administered to patients. Before surgical stop of bleeding (124±11 minutes from the start of the operation), 75±6.7% of the total volume of ITT was transfused. In total, during the operation, due to DE and AE, 54.4 ± 13.1% of lost erythrocytes were returned. In group 2, during 180±8.5 minutes of surgery, the volume of ITT was 11,258±547 ml, including 83±2.1% of the total intraoperative volume of ITT was used before surgical hemostasis (after 141±9 minutes). During surgery, 72.5±4.4% of lost red blood cells were returned. Differences in the volume and structure of infusion therapy between groups were statistically insignificant; the structure of ITT is presented in Table. 2.
There was a statistically significant difference in absolute blood transfusion volumes between groups. Thus, the volume of media containing erythrocytes was significantly less in group 1 (p = 0.008), therefore, with the predominant use of DE, it was possible to return fewer erythrocytes than with the combined use of AE and DE.
Hb and Ht levels are often used as reference indicators when assessing the results of blood transfusion. We found a statistically significant increase in Hb and Ht after blood transfusion in each group (Table 3),
however, these indicators were significantly lower than the reference values. There were also inverse relationships between the increase in Hb and Ht parameters after blood transfusion and the volume of used media containing erythrocytes - for Hb τ = –0.285 (p = 0.002), for Ht τ = –0.256 (p = 0.001). There was an inverse relationship between the volume of ITT and the levels of Hb at the end of surgery (τ= –0.225, p=0.004) and Ht at the end of surgery (τ= –0.221, p=0.004). With a volume infusion necessary to replenish the circulating blood volume and support, due to hemodilution, the need for blood transfusion supposedly increases (partial correlation coefficient adjusted for the volume of blood loss R = 0.529, p < 0.0001).
Blood transfusion is primarily aimed at compensating for lost oxygen carriers and, accordingly, CaO2 should increase after it. However, in both groups we did not detect significant dynamics of CaO2 after blood transfusion (see Table 2). In addition, the correlations between CaO2 at the end of surgery and the volume and quality of returned red blood cells were not statistically significant. Accordingly, intraoperative blood transfusion was not accompanied by an immediate increase in CaO2, and hemic disturbances in oxygen transport persisted immediately after blood transfusion.
The central place in the pathophysiology of any critical condition is occupied by oxygen debt, which directly affects the survival of patients and the development of complications. In the clinic, it is determined by indirect signs - CvO2, SvO2, Lac, O2ER. At all stages of the study, in both groups, CvO2 was below normal values, without significantly differing between groups and at intervention stages within the group (see Table 2). Of all the correlations between CvO2 and ITT characteristics, only the connection with the degree of compensation for blood loss (percentage of returned red blood cells compared to lost ones) had statistical significance - τ = 0.223 (p = 0.038).
SvO2 also did not differ significantly between groups or within each group during the study phases. Its average values remained reduced and depended on the volume of blood transfusion (τ=0.197, p=0.046) and the volume of ITT (τ= –0.197, p=0.046).
O2ER exceeded expected values at all stages of the study. In group 1 it changed insignificantly. In group 2, there was a tendency toward normalization of O2ER after ITT (see Table 2), when it decreased by 26.2% (p>0.05). At the end of the operation, O2ER in both groups exceeded normal values and depended on red blood cell deficiency (τ=0.205, p=0.04), the volume of intraoperative ITT (τ=0.197, p=0.046) and the degree of compensation for lost red blood cells, expressed as a percentage (τ = –0.197, p=0.046).
In both groups, mean Lac values increased during surgery (see Table 3). In the 1st group, the Lac content after stopping bleeding increased by 37% (by 3.06±0.50 mmol/l; p<0.0001), in the 2nd group - by 43.6% (by 2.80 ±0.39 mmol/l; p=0.015). In group 2 at the end of the operation, the Lac level was significantly lower than in group 1 (p = 0.032). When analyzing the correlations between Lac at the end of the operation and ITT characteristics, there was a statistically significant relationship with the volume of DE used (τ=0.428, p<0.0001), the proportion of DE in the structure of blood transfusion (τ=0.309, p=0.0003), and the volume of blood transfusion (τ=0.242, p=0.004), volume of ITT (τ=0.253, p=0.003). Of course, the Lac level increased at the end of the operation for many reasons, and the identified associations reflected only the contribution of some characteristics of intensive care.
So, intraoperative transfusion of large volumes of AE and DE and replacement of circulating blood volume did not lead to immediate restoration of the hemic component of oxygen transport and compensation of oxygen debt.
When analyzing mortality rates, we found significant differences between groups. Thus, in the 1st group, 12 (85.7%) patients died, in the 2nd group - 45 (58.4%) patients (p = 0.039). Intraoperative mortality did not differ between groups. In group 1, 5 (35.7%) patients died on the operating table; in group 2, 28 (36.4%) patients died. Postoperative mortality was significantly lower in group 2. In the 1st group, 7 (50%) people underwent surgery and died in the postoperative period (on the 1st day - 21.4%, after 3 days - 28.6%), in the 2nd group - 17 (22% ) patients (on the 1st day - 14.3%, on the 2-3rd day - 1.3%, later than 3 days - 6.4%) (p = 0.018).
Statistically significant differences in mortality between groups were also reflected in the odds ratio (OR) of survival (“survived/died”). In group 1, this figure was 0.403 (95% confidence interval - CI = 0.183-0.885; p = 0.011), in group 2 - 1.385 (95% CI = 1.101-1.741). Consequently, predominantly intraoperative DE transfusion increases the risk of death in the postoperative period.
Of course, intraoperative factors influencing mortality in acute blood loss require further study, including a detailed analysis of the features of intraoperative ITT.
Thus, with the predominantly intraoperative use of autoerythrocytes to compensate for blood loss of more than 70% of the circulating blood volume, hospital and postoperative mortality is reduced.
With maximum intraoperative use of autologous blood, there is less accumulation of lactate at the end of the operation.
In case of acute blood loss of more than 70% of the circulating blood volume, intraoperative hemotransfusion of autoerythrocytes and donor erythrocytes in any ratio is not accompanied by an immediate increase in hemoglobin and hematocrit, normalization of oxygen balance (oxygen content in arterial and mixed venous blood, hemoglobin saturation in mixed venous blood with oxygen, oxygen extraction coefficient ).
Types of autohemotherapy
Fresh, unpurified blood is most often injected into the muscles, but this is not always the case. In some cases, various drugs are added to the plasma and injected into reflexogenic points or back into the vein. Types of autohemotherapy:
- Introduction of autologous blood. The molecular composition of plasma can be changed by exposure to X-ray waves, ultrasound, or freezing.
- Biopuncture. Blood mixed with oxygen, which enters it as a result of shaking, is injected into reflexogenic points. Sometimes homeopathic medicines are added to the composition.
- Ozone cleaning. To enhance the immunomodulatory, anti-inflammatory and antiviral effect, plasma is ozonated. This composition is injected into a vein, and not into the muscles.
- Stepwise technique. If the problem is infectious, antibiotics are added to the plasma.
Other symptoms
In addition to the skin, psoriasis affects nails, hair, as well as joints and internal organs. Changes on the nail plate begin at the base and are characterized by subungual hyperkeratosis. Subsequently, the surface becomes striated, and impressions form on it (thimble symptom). Psoriatic arthritis begins with damage to small joints and is accompanied by pain and inflammation. Also, scaly lichen is characterized by itchy skin. The result is scratching, superficial cracks and a tendency to bleed. In places of trauma, pathogenic microbes can multiply, which leads to secondary infection and the development of dermatitis.
Contraindications to the procedure
There are few absolute contraindications, but there are certain restrictions. Autohemotherapy will have to be postponed during pregnancy and lactation, with a low level of hemoglobin, with a viral infection, menstruation, during menopause, inflammatory processes of the appendages, etc. The procedure is not recommended for severe forms of arrhythmia, the presence of neoplasms (malignant and benign). The final decision on the possibility of using the method in a particular case is made by the doctor.
Prices for services
| Intravenous infusion of ozone-saturated saline solution, 1 procedure | RUB 2,376 |
| Intravenous infusion of ozone-saturated saline solution, 5 procedures | 6,050 rub. |
| Intravenous infusion of ozone-saturated saline solution, 10 procedures | 11,000 rub. |
| ILBI (intravascular laser irradiation of blood), 1 procedure | RUB 3,459 |
| ILBI (intravascular laser irradiation of blood), 5 procedures | 6,050 rub. |
| ILBI (intravascular laser irradiation of blood), 10 procedures | RUB 11,385 |
| Autohemotherapy (without the cost of the drug), 1 procedure | RUB 1,185 |
The term “psoriasis” comes from the Greek word “psoriasis”, which means “pruritus” or “itchy skin”. It is these symptoms that most clearly characterize this non-infectious dermatological problem. With such dermatosis, skin cell division occurs almost thirty times faster. Since they do not have time to fully mature, intercellular contacts are lost. This leads to the formation of characteristic scales. The body’s immune system is also involved in the pathological process: protective elements are directed against its own cells, which causes chronic inflammation in the lesion. Let us describe in more detail the question of what psoriasis is and how to treat it.