Classification
Depending on the number of bacteria, some experts conditionally distinguish minor and severe bacteriuria. In clinical practice, only one classification is used to determine the patient’s treatment tactics:
- Asymptomatic bacteriuria.
It is characterized by the detection of bacteria in the urine in the absence of any complaints and other laboratory signs of urinary system infections (leukocyturia, etc.) in the patient. - Symptomatic bacteriuria.
A combination of clinical symptoms and identification of bacteria in a urine sample.
Preparing for a urine test and rules for collecting urine
The biochemical composition of urine directly depends on the quantity and quality of fluid and food consumed, as well as physical and psycho-emotional stress. Therefore, on the eve of the procedure, it is recommended to avoid fatty and spicy foods, sweet or spicy delicacies. It is necessary to reduce physical activity.
Urine is collected in the morning in a clean and dry container. For research, it is advisable to take a “medium” portion. Before collecting biomaterial, it is recommended to carry out hygienic treatment of the external genitalia using a shower or wet wipes. During menstruation, it is advisable to refrain from taking the test, as its results during this period may be inaccurate. It is not recommended to collect material after sexual intercourse and defecation, or to use urine that has been in the refrigerator for more than 3 hours for research.
Causes of bacteriuria
Violation of preparation for analysis
A fairly common cause of bacteriuria. Improper preparation for a urine test, especially failure or careless toileting of the external genitalia, can lead to false positive results. It is also considered incorrect to take a urine test during menstruation. Blood, being a breeding ground for bacteria, creates a favorable environment for their reproduction.
When using non-sterile containers to collect urine, the sample may be contaminated with foreign flora. To submit urine to a bacteriological laboratory for culture, it is recommended to use special tubes with preservatives (boric acid, formate and sodium borate) that stabilize the bacterial composition of urine.
Asymptomatic bacteriuria
Detection of bacterial flora in the urine without clinical and laboratory signs of infectious and inflammatory diseases UVP occurs in 1-5% of healthy premenopausal women, in 2-10% of pregnant women, in 4-20% of healthy elderly men and women. In young healthy men, asymptomatic bacteriuria is almost never observed.
Such age-sex characteristics of bacteriuria are associated with the anatomical and physiological characteristics of the female urogenital system, changes in hormonal levels during pregnancy and menopause, as well as age-related changes in local immunity. Asymptomatic bacteriuria is a benign condition and does not require any intervention, except in some patients at high risk for developing UTI infection.
Bacteriuria
Urinary tract infections
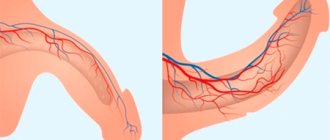
The most common cause of bacteriuria is acute, chronic and recurrent forms of urinary tract infections. The causative agents of these pathologies are mainly gram-negative enterobacteria - Escherichia coli, Klebsiella, Proteus. Very rarely, infections of the genitourinary system are caused by gram-positive flora - staphylococci, enterococci. Infection occurs in several ways. The most common is the ascending route - through the urethra to the bladder and/or kidneys.
Less commonly, a hematogenous or lymphogenous route is possible. This option occurs when there is an additional source of infection in the body - pneumonia, infections of the oral cavity, ENT organs. The degree of bacteriuria can be different; it does not correlate with the severity of the disease and disappears almost from the first days of treatment with properly selected antibacterial drugs.
- Pyelonephritis.
This is an infectious inflammation of the renal collecting system involving interstitial tissue. It develops mainly in young women (5-6 times more often than in men). - Cystitis.
Inflammation of the mucous membrane of the bladder. A single episode of cystitis occurs in half of women worldwide. - Nonspecific urethritis.
Inflammation of the urethra, on the contrary, is more common in men due to a longer and narrower urethra.
Genital infections
Bacteriuria in infections of male and female genital organs is very rare. They are caused by nonspecific opportunistic gram-negative and gram-positive flora (Escherichia coli, enterococci, anaerobic bacteria) and often occur together with cystitis and urethritis. The severity of bacteriuria is in no way related to the intensity of the inflammatory process.
- Infections of the male genital area.
These include bacterial prostatitis (occupies about 10% of all cases of inflammation of the prostate gland), and extremely rarely, orchitis and epididymitis (inflammation of the testicle and its epididymis), balanoposthitis (inflammation of the head and foreskin of the penis). - Infections of the female genital area.
These infections include inflammation of the vagina and/or vulva (vaginitis, vulvovaginitis), and cervix (cervicitis).
It is worth noting that in the case of infectious diseases of the genital organs caused by bacteria that provoke sexually transmitted diseases, such as chlamydia, mycoplasmosis, gonorrhea, bacteriuria does not develop. These infections are diagnosed by other special research methods.
Risk factors for bacteriuria
This group includes diseases or conditions that contribute to the appearance of microorganisms in the urine:
- Glucosuria
: poorly controlled hyperglycemia in diabetes mellitus, long-term use of glucocorticosteroids, various endocrine disorders (Cushing's disease/syndrome, pheochromocytoma, glucagonoma). - Previous UTIs
. - Impaired urine outflow
: urolithiasis, congenital anomalies of the structure of the urinary system, ureteral stenosis. - Reverse reflux of urine
: vesico-ureteropelvic reflux. - Presence of an installed urinary catheter
. - Shift in urine pH to the alkaline side
: dietary habits, medications.
Mycoplasma urethritis.
They are caused by bacteria that have a plastic shell and contain DNA and RNA. The ability of mycoplasmas to take any form allows them to penetrate bacterial filters.
Infection with mycoplasma infection occurs primarily through sexual contact. Intrauterine infection of the fetus and during its passage through the infected birth canal have been established. Mycoplasma attaches to the urethral epithelium and can be transferred by sperm; in addition, it colonizes the foreskin. The incubation period lasts from 3 to 5 weeks.
There are no specific signs for mycoplasma urethritis. As a rule, urethritis of mycoplasma origin is chronic. In this case, there are often lesions of the prostate gland, seminal vesicle, and epididymis, which leads to infertility. By attaching to the head of the sperm, mycoplasma can reduce its fertilizing ability. Under certain conditions, mycoplasma infection can cause inflammatory processes in the genitourinary organs (cystitis, pyelonephritis). Urogenital mycoplasmosis is often combined with intestinal damage (enterocolitis).
Diagnostics
There are several diagnostic methods for detecting bacteriuria. Proper preparation required before taking the test. In a specific clinical situation, the attending physician selects a specific study or a combination of methods:
- Microscopy.
Detection of bacteria by direct microscopic examination of centrifuged urine sediment. The method has extremely low diagnostic value. Microscopy may reveal signs of improper patient preparation - an abundance of diverse flora, a large amount of mucus and squamous epithelial cells. - Nitrite test.
During their life, bacteria that colonize the genitourinary tract convert nitrates from food into nitrites. Urine test strips have a special reagent zone that stains in the presence of nitrites. The test may be false negative if there are no nitrates in the patient’s diet, infection with bacteria that do not form nitrites (streptococci), or high levels of ascorbic acid in the urine. - Bacteriological culture.
This method is considered the gold standard for diagnosing bacteriuria. In the laboratory, a urine sample is cultured with culture media for specific bacteria. To confirm the diagnosis of asymptomatic bacteriuria, at least 2 cultures are required with an interval of 24 hours. The disadvantage of this method is the long waiting time for results - 2 or 3 days. - Flow cytometry.
Some modern automatic analyzers are capable of performing a detailed assessment of the cellular composition of a urine sample, including counting the number of bacteria.
Microscopy, nitrite test and flow cytometry are considered indicative methods for detecting bacteriuria, and microbiological culture is a confirmatory method. An important point is that in the case of bacterial growth reaching a clinically significant titer (above 10x5 colony-forming units per ml) during culture, sensitivity to antibacterial drugs must be determined. This is necessary for selecting therapy.
In addition to detecting bacteriuria, additional studies are required to differentiate the etiology of its occurrence:
- Analysis of urine.
TAM indicators help to determine the cause of bacteriuria. For example, the presence of leukocytes and an alkaline urine reaction highly likely excludes asymptomatic bacteriuria; an increase in protein content and red blood cells may indicate pyelonephritis. Detection of transitional epithelial cells by microscopy indicates damage to the bladder or urethra, and renal epithelium and a large number of cylinders indicate damage to the kidneys. - Ultrasound.
Ultrasound of the kidneys with pyelonephritis shows an expansion of the ventricular region, and abnormalities in the structure of the ureters can also be detected. With prostatitis, ultrasound of the prostate gland reveals an increase in its size and a decrease in echogenicity. With epididymitis, ultrasound of the testicle visualizes enlargement of the epididymis and diffuse changes. - Examination by a gynecologist.
If you suspect a gynecological disease, you need to consult a gynecologist who examines the genital organs, bimanual vaginal examination, and colposcopy. If necessary, a smear is taken from the mucous membranes or secretions for cultural examination. - Examination by a urologist.
Similarly, if indicated, men are scheduled to consult a urologist for a digital rectal examination, collection of prostatic fluid or ejaculate.
Culture of urine on nutrient media
Herpetic urethritis.
Caused by two serotypes of DNA containing herpes simplex viruses HSV-1 and HSV-2. Herpes is one of the most common human infections.
The disease is transmitted primarily through sexual contact from a patient with genital herpes. Often, the genital virus is transmitted from a carrier of herpes who does not have symptoms of the disease. The method of infection with the virus can be genitogenital, oral-genital, genital-anal. There is a risk of neonatal infection of newborns, which can occur both during the passage of the birth canal and in the postpartum period with active herpetic manifestations in the mother or medical personnel.
During the initial infection caused by the herpes simplex virus, the virus penetrates the cells of the susceptible surfaces of the mucous membrane or skin. It is then captured by sensory nerve endings and transported to the nerve cells of the dorsal root ganglia, where it is stored. Infection can occur latently, when the virus is present in the body without causing illness; and virulent when the herpes is activated and causes local lesions. The disease in this case occurs as chronic, recurrent, cyclical with localized, less often generalized manifestations.
The initial symptoms of herpetic urethritis may be general complaints: fever, weakness, myalgia, headache. At the same time, a burning sensation appears in the urethra, which intensifies during urination, and pain in the lymph nodes. On the head, skin of the penis, on the visible part (possibly also on the invisible) mucous membrane of the urethra, the typical development of herpetic elements is noted, accompanied by a feeling of burning, itching, pain in the genital area. First, bubbles appear, which erode, become wet, then dry out, forming crusts that fall off as epithelization occurs. Temporary hyperemia and pigmentation remain at the site of the lesion. Light yellow discharge may appear from the urethra.
Clinical manifestations of the primary infection last about 3 weeks, local symptoms appear on the 2-14th day. Recurrent infection in the presence of antibodies to the virus is less pronounced. The clinical picture develops within 8-15 days. Recurrence is promoted by stressful situations, overheating, hypothermia, decreased body defenses, etc. Herpes, by destroying the human immune system, can cause secondary immunodeficiency.
Some researchers note a connection between genital herpes and cervical cancer and prostate cancer.
Correction
If bacteriuria is detected, you must consult a doctor for correction. Asymptomatic bacteriuria in the vast majority of cases does not require treatment. The exceptions are pregnant women, patients with installed urinary catheters, patients with poorly controlled diabetes mellitus - these patients are indicated for antibacterial therapy. For symptomatic bacteriuria, the following treatment is recommended:
- Pyelonephritis
. First-line drugs are pecinillins (amoxicillin/quavulanate), cephalosporins (cefixime, ceftibuten). For strains that are resistant to them, they resort to fluoroquinolones (levofloxacin, ciprofloxacin), new generation cephalosporins (cefepime). - Cystitis
. Fosfomycin trometamol or nitrofurans (nitrofurantoin, furazolidone) are used. For recurrent cystitis, medications based on cranberry extract, D-mannose, and herbal remedies (canephron) are prescribed. Also, for relapses, some experts recommend lyophilisate of bacterial lysate of Escherichia coli. - Genital tract infections
. For prostatitis and epididymitis, fluoroquinolones and macrolides (azithromycin) are used; for vulvovaginitis, cervicitis, instillations of antiseptic solutions and antibiotics active against anaerobic flora (metronidazole, clindamycin) are used.
Urine analysis according to Zimnitsky
Urine analysis according to Zimnitsky
is one of the ways to check the excretory function of the kidneys, which helps determine how correctly these organs are functioning and whether the patient is at risk of possible complications in the form of acute renal failure. This study is recommended in cases of certain diseases:
No special preparation is required for Zimnitsky's analysis. The patient does not need to limit himself in food and drink. Immediately before collecting biomaterial, it is recommended to exclude spicy dishes and foods that stain urine - beets, rhubarb - from the regular menu. For the study, you will have to stock up on a set of 8 clean jars, as well as a notepad for recording the volume of liquid consumed and the time for collecting the analysis in the next container. Every time before visiting the toilet, it is necessary to perform genital hygiene.
When examining urine, any detected deviations from established standards in the direction of exceeding them are considered to be pathology.
Improper functioning of the kidneys is also indicated by the presence of protein, epithelial cells, and bacteria in the urine. Don't panic and self-medicate. Only a specialist can correctly interpret the analysis results!
Sign up for a urine test
Make an appointment
Forecast
Bacteriuria in itself cannot serve as a predictor of clinical outcome. The prognosis is directly determined by the underlying disease - the most favorable for asymptomatic bacteriuria, cystitis, urethritis. Frequently occurring pyelonephritis contributes to the formation of kidney stones. With severe bilateral pyelonephritis, serious life-threatening complications can develop - carbuncle, kidney abscess, hydronephrosis. An extremely rare and most fatal consequence of pyelonephritis is urosepsis.