Meningococcal infection is an acute infectious disease, the first sign of which is acute nasopharyngitis or inflammation of the nasopharynx, followed by the development of meningococcemia and purulent meningitis.
The causative agent of purulent meningitis and meningococcemia is Neisseria meningitidis, a gram-negative bacterium that exists in the form of different serological types, that is, it has a fairly large variety of antigens against which the human immune system will have to produce antibodies in case of contact with this infection.
Large epidemics of meningitis are most often caused by group A meningococcus. However, group B meningococcus is also of great importance in the epidemiology of meningitis.
Meningococcal infection, routes of infection
Meningococcal infection is transmitted by airborne droplets. The source of infection is always a person suffering from acute nasopharyngitis, with an acute generalized form of meningococcal infection, or a healthy carrier. Usually the number of carriers of meningococcus is no more than 5 percent, but during an epidemic in the source of infection the proportion of carriers can reach 50%. In this case, carriage of meningococcus is usually short-lived, about a week.
Periodic rises in the disease occur approximately every 10 to 12 years.
Advantages of JSC "SZDCM"
Laboratory tests are extremely important in the treatment, especially of such serious diseases. It is important to get not only the fastest, but also the most accurate and detailed result.
At your service:
- Laboratory with technological equipment.
- Qualified and friendly staff.
- Fast analysis and several options for obtaining results.
Medical centers and terminals are located in places with convenient transport links in St. Petersburg, Leningrad region, Veliky Novgorod, Staraya Russa, Okulovka and Pskov.
Meningococcal infection, signs and symptoms
As already mentioned, the most common form of meningococcal infection is nasopharyngitis. When meningococcus enters the upper respiratory tract, a local inflammatory process develops on the mucous membrane of the nasopharynx. The incubation period is 2–3 days, followed by the prodromal or initial period of the disease, during which the patient with meningococcal infection is most contagious. Acute nasopharyngitis develops over 1 to 3 days and is characterized by a rise in temperature to 38.0 C, bright hyperemia (redness) and granularity of the posterior wall of the pharynx, which is covered with mucopurulent discharge. Redness of the tonsils, cough, runny nose with mucous discharge mixed with greenery and pus are also noted. The disease can last 3-5 days and end with recovery, or it can become a generalized form. In this case, penetration of the pathogen into the bloodstream is accompanied by the appearance of chills, headache, and a rise in temperature to 40 C. Generalized meningococcal infection can lead to the development of purulent foci in various internal organs: lungs, heart, joints. But the worst complication is meningococcemia (meningococcal sepsis). Moreover, in young children, meningococcemia can occur suddenly against the background of complete health, with an increase in body temperature to 40 - 41 degrees C in a few hours and is accompanied by headache, uncontrollable vomiting, pain in the muscles and limbs. A characteristic sign of meningococcemia is the appearance of a star-shaped hemorrhagic rash (small pinpoint hemorrhages on the skin that resemble a starry sky).
And finally, another severe form of meningococcal infection is meningitis, which also develops against the background of acute nasopharyngitis. Meningococcal meningitis begins acutely, with a rise in body temperature to high numbers, a sharp painful headache, and uncontrollable vomiting not associated with food intake.
All forms of generalized meningococcal infection require immediate hospitalization in a specialized infectious diseases department and antibacterial and intensive detoxification therapy.
Treatment
When treating meningococcal infection, regardless of the degree of manifestation of the disease and its form, the doctor considers the patient’s condition as mortally dangerous. This is especially true for children, because more than half of them go through intensive care. The patient is hospitalized for emergency diagnostics. Antibiotics can be prescribed only after laboratory tests.
Depending on the serotype, the basis of treatment may be drugs such as penicillin, ampicillin, chloramphenicol. In epidemiological conditions with limited resources, ceftriaxone is preferred. Antibiotics are the basis of treatment, however, antipyretic, anticonvulsant and decongestant drugs, infusion, detoxification and oxygen therapy medications are used together with them. In this way, complex treatment of meningococcal infection is carried out with individual selection of drugs, under the constant supervision of a doctor. Therapy for complicated generalized forms can last for a month, and rehabilitation can take several years.
Meningococcal infection and vaccination
The main group of people subject to vaccination against meningococcal infection are children living in closed communities, as well as those going on vacation to organized summer holiday camps. Polysaccharide meningococcal vaccines, such as Meningo A+C or Mencevax, are widely used in medical practice.
These vaccines are intended for immunization of children from 2 years of age and adults using a single dose of vaccine, followed by revaccination after 2 to 3 years.
Thus, meningococcal infection is certainly one of the diseases against which it is easier and cheaper to vaccinate in order to protect yourself from possible unpleasant complications. Naturally, the feasibility and safety of each vaccination must first be discussed with your attending physician, and, if necessary, with a specialist, an immunologist.
Meningococcus is not only in Africa
This infection is widespread throughout the world. And in Africa there is even a so-called “meningitis” or “meningococcal belt”:
However, this disease does not only exist somewhere far away, on other continents; unfortunately, it is also close to us. Outbreaks of meningococcal infection are recorded every now and then in different regions of Russia.
For example, in Novosibirsk in 2021, 25 cases of the disease were registered in less than two weeks. And this is very characteristic of this infection: usually long periods of well-being (10-15 years) are interrupted by sharp increases in incidence, which have a focal outbreak nature.
The increase in incidence can be explained by the widespread carriage of meningococcal bacteria. As the number of susceptible individuals increases, the number of cases increases. And declines are ensured by an increase in the immune layer as a result of latent immunization as bacterial carriage spreads among the population of a given territory.
You need to understand that during recession years the infection does not disappear: 50% of diseases occur in children under 5 years of age; 20% - for children aged 6-14 years. As age increases, incidence rates decrease, but carriage rates increase. The age group of 15-20 years is also subject to a high degree of susceptibility, because its representatives - students, military personnel - communicate intensively in schools, dormitories, barracks, etc. First of all, those who come from remote areas get sick, i.e. not previously in contact with the pathogen.
Why are doctors sometimes unable to identify meningococcal infection in the early stages of the disease and provide timely assistance? The fact is that the first symptoms of the disease are similar to the onset of a regular acute respiratory viral infection, and later medicine turns out to be powerless against the lightning-fast course of the disease. Moreover, during periods of prosperity, cases of the disease are so rare that the alertness of even experienced doctors, not to mention young novice doctors, gradually decreases.
One of the features that can also be canceled is that meningococcal infection is characterized by a winter-spring seasonality with the maximum number of diseases in February – April.
There are many real stories about how this can happen, here is one of them (a video from our partners - Sanofi Pasteur):
Latest epidemics
It is estimated that 80-85% of all cases in the meningitis belt are caused by group A meningococcus, and epidemics occur every 7-14 years. The highest rates of the disease are found in the meningitis belt of sub-Saharan Africa, stretching from Senegal in the west to Ethiopia in the east.
During the 2009 epidemic season, a total of 88,199 suspected cases, of which 5,352 were fatal, were reported in 14 African countries conducting enhanced surveillance. This is the largest number of victims since the 1996 epidemic.
Diagnostics
The initial diagnosis of meningococcal meningitis can be made by clinical examination followed by a spinal tap to identify purulent cerebrospinal fluid. Sometimes bacteria can be seen when cerebrospinal fluid is examined under a microscope. The diagnosis is supported or confirmed by growing bacteria from cerebrospinal fluid or blood samples based on an agglutination test or polymerase chain reaction (PCR). To determine infection control measures, it is important to identify serogroups and perform antibiotic susceptibility testing.
What complications may there be?
As mentioned above, if meningococcal infection is detected late, there is a high probability of death. However, even if treatment was prescribed on time, often the disease does not go away harmlessly. The consequences can lead to a variety of complications, ranging from hearing loss, vision and speech disorders, to amputation of limbs, paralysis, epilepsy and hydrocephalus. And here is another video (video by our partners - Sanofi Pasteur) with a girl who, at the age of 5, suffered a meningococcal infection and was left deaf for the rest of her life:
Epidemiological surveillance
Surveillance, from case detection to investigation and laboratory confirmation, is critical to the control of meningococcal meningitis. Main objectives of surveillance:
- detection and confirmation of disease outbreaks;
- detection and confirmation of disease outbreaks;
- assessing the burden of disease;
- monitoring antibiotic resistance profiles;
- monitoring the circulation, spread and evolution of individual meningococcal strains (clones);
- assessing the effectiveness of strategies to control meningitis, in particular preventive vaccination programs.
General information
Meningococcal disease is potentially fatal and should always be treated as a medical emergency. Causes meningococcal meningitis - this is a bacterial form of meningitis - and is a serious purulent infection of the membranes surrounding the brain and spinal cord.
Meningitis is caused by a number of different bacteria. One such bacteria that can cause epidemics is Neisseria meningitidis. Twelve serogroups of N. meningitidis have been identified, six of which (A, D, C, W135 and X) can cause epidemics.
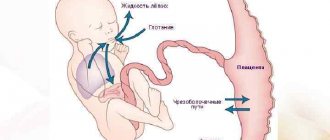
The bacterium is transmitted from person to person through droplets of secretions from the respiratory tract or throat of the carrier. Close and prolonged contact, such as kissing, sneezing, coughing toward another person, or living in close proximity to an infected person (for example, in a shared bedroom or sharing utensils), helps spread the disease. Bacteria can be carried in the throat, and sometimes, for reasons that are not entirely clear, by overwhelming the body's defenses, the infection spreads through the bloodstream to the brain.
Despite remaining gaps in our knowledge, it is estimated that 10–20% of the population are carriers of N. meningitidis at any given time. However, in epidemic situations the number of carriers may be higher. In an epidemiological sense, carriers are the most dangerous, since there are 1200-1800 carriers per one sick person.