Movies often depict how the pregnant heroine suddenly bursts out with amniotic fluid. After which the birth itself inevitably begins. Reality is often not so epic, and everything is not so fleeting. For some expectant mothers, water rather flows slowly and in a thin stream, and labor begins only after some time. Here we will tell you about how your water breaks and what happens next. There is definitely no need to panic - your doctor will also tell you how this happens and what follows.
Amniotic fluid: what happens when it breaks
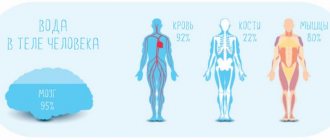
During pregnancy, the fetus is surrounded by amniotic fluid in the amniotic sac, which protects it from external factors. Amniotic fluid promotes the development of the baby's lungs and gastrointestinal tract, and also maintains a constant temperature. During the second half of pregnancy, amniotic fluid consists primarily of the baby's urine, but it also contains nutrients, hormones and antibodies that help fight infections. At the beginning of contractions or during them, and sometimes before the onset of contractions, the membranes of the membranes rupture. This stage of labor is referred to as “the water has broken.” Often this is how the onset of labor manifests itself at an early stage. Doctors do not know what exactly causes the bladder to rupture.
Treatment
Treatment is aimed at eliminating the cause that caused the change in the amount of water. Complex therapy for feto-placental insufficiency is usually carried out, since it almost always occurs with both oligohydramnios and polyhydramnios.
If an infection is detected, antibiotic treatment is prescribed. With this pathology, antibiotic treatment can be prescribed even if no infection is detected (which often causes confusion among expectant mothers). The fact is that it is impossible to examine all existing microorganisms, and if the doctor does not see any other causes of polyhydramnios, treatment is carried out against infection, since this is the most common cause of polyhydramnios.
If fetal malformations incompatible with life are detected before 28 weeks, the woman is offered termination of pregnancy.
If other causes are identified (increased blood pressure in the mother, diabetes mellitus, Rh conflict, etc.), the underlying disease is treated.
An increase or decrease in fluid intake does not affect the amount of amniotic fluid.
How the water breaks: sensations
All expectant mothers' water breaks differently. Even if you already have children, this time may be different. The sensations may be different: water may flow in a thin stream or flow out in a sharp stream. Sometimes a faint pop is felt, and sometimes the liquid comes out in portions when changing position. The way the water drains is influenced, for example, by the position of the baby's head, which closes the cervix like a plug. When the head moves, fluid comes out. Also, water leaks during contractions, and this process continues until the baby is born. If your water begins to break and you are going to the hospital by car, take with you an absorbent diaper or towel to sit on.
As a rule, amniotic fluid is clear or pale yellow in color and odorless. The most fluid accumulates inside the bladder by the 36th week of pregnancy - about 950 milliliters, and then the water level gradually decreases.
How do you know if your water has broken? Sometimes it may not be clear whether your water has broken, or, for example, you are simply leaking urine (when you feel an occasional thin stream or your laundry gets wet). There is no need to be tormented by doubts; consult your supervising doctor. You can determine whether your water has broken during an examination or with the help of an ultrasound.
Complete rupture of water: signs
The most important sign of water breaking is the release of a large amount of fluid from the perineum.
Some women clearly feel cotton inside the abdomen, which is accompanied by further leakage of water. In rare cases, there may be a nagging, paroxysmal pain in the lower abdomen. First, the so-called “anterior” fluid is discharged, thanks to which the baby begins to move along the birth canal. For some women, the bladder ruptures while taking a shower. After the amniotic fluid is released, the contractions intensify and the woman enters the second stage of labor.
What happens after your water breaks?
If you think your water is breaking, record the time. You can also note the frequency of contractions if you start having contractions. Contractions often begin a short time after your water breaks.
How soon will I give birth? You might be wondering. It is difficult to answer accurately, because the duration of contractions and childbirth is individual and depends on many other factors: the time the waters break, whether this is the first birth or not, whether there are any complications. At this moment, concentrate on the main thing: months of waiting are behind you, very soon you will see your baby for the first time!
The phenomenon in which the waters break before the onset of labor, regardless of the stage of pregnancy, is called premature rupture of membranes (PROM). This happens in 8-10 percent of pregnant women. Most often, the water breaks during contractions. If your water breaks but you are not having contractions, your doctor may recommend inducing labor. Stimulating contractions will reduce the likelihood of infection, which increases over time.
If you are in doubt whether labor has begun or not, contact your supervising doctor, who will be able to determine exactly what is happening to you.
Clinic of low and polyhydramnios
With polyhydramnios, the size of the abdomen increases. Because of this, stretch marks occur more often, and the venous pattern on the abdomen is enhanced. During the examination, the doctor has difficulty palpating parts of the fetus, and the heartbeat is not clearly heard. The fetus easily changes its position (unstable fetal position). A woman with severe polyhydramnios may experience difficulty breathing, heaviness, and increased heart rate.
With polyhydramnios, an abnormal position of the fetus is often observed: transverse or oblique position, or breech presentation. Excessively free movement of the fetus in large amounts of fluid can lead to the entanglement of the umbilical cord around the neck or body of the fetus. Due to the strong stretching of the membranes, premature rupture of amniotic fluid and premature birth more often occur. Due to the strong stretching of the uterus, its contractile activity deteriorates, which can lead to weakness of labor. In severe cases, when there is a lot of water, due to the pressure of the enlarged uterus on the lungs and difficulty breathing, the mother may experience hypoxia (lack of oxygen in the blood), which causes or aggravates fetal hypoxia.
With oligohydramnios, the size of the abdomen lags behind the norm. The motor activity of the fetus may decrease, as the baby is “cramped”. Sometimes fetal movements can cause pain to the woman.
With oligohydramnios, a complication may occur such as compression of the umbilical cord between the fetus and the walls of the uterus, which can lead to acute oxygen deficiency and fetal death. Since with a small amount of water the fetus is more tightly squeezed in the uterus and its movement is difficult, the newborn more often has a curvature of the spine, problems with the hip joints, torticollis, and clubfoot. If oligohydramnios appears already in the second trimester of pregnancy, intrauterine fetal death often occurs.
The lower pole of the amniotic sac during oligohydramnios is flat and cannot perform its function as a hydraulic wedge during childbirth; on the contrary, it delays the advancement of the head, so weakness of labor occurs.
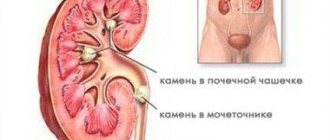
Usually the amount of amniotic fluid is determined by ultrasound. Ultrasound determines such indicators as the vertical pocket (VP) and the amniotic fluid index (AFI). The vertical pouch is the maximum area of free fluid between the fetus and the anterior abdominal wall. Normally, it is 5-8 cm. AFI is a more accurate indicator; it is the sum of the values of the vertical pockets in the four quadrants of the uterus (the uterus is conventionally divided into 4 parts, and the maximum vertical pocket is measured in each). The norms of this index are different for each stage of pregnancy (they may differ slightly on different devices). On average, the normal IAF is 5-24 cm.
VC and IAF are not 100% methods for diagnosing polyhydramnios and oligohydramnios. Sometimes errors may occur.
Since both polyhydramnios and oligohydramnios can be signs of fetal developmental abnormalities, fetal anatomy is studied especially carefully using ultrasound. If, in addition to the “wrong” amount of water, some other signs of chromosomal abnormalities are detected, the woman is sent for cordocentesis - a blood test from the umbilical cord, which determines the genotype of the fetus.
When to see a doctor
If you are pregnant full term and your water breaks, stay calm and contact your doctor or maternity hospital to find out when you need to leave. You should also consult a doctor in the following cases:
- The waters broke before the 37th week
of pregnancy
, - Contractions don't start
although the waters have already broken. In this case, your doctor may recommend inducing labor.
In case the doctor recommends that you go to the maternity hospital immediately, you should have a bag packed with all the necessary things.
“The doctor always sees whether a woman has given birth or not”
►How does having a baby affect your breasts?
– Within a year after lactation, the mammary gland usually restores its shape. But there are other problems: women are sometimes bothered by colostrum discharge from the nipples even after cessation of lactation - lactorrhea. This happens because the elevated level of the hormone prolactin remains, and the milk ducts of the glands remain dilated.
Here the right thing to do would be to visit a mammologist and perform an ultrasound of the mammary glands. If, as a result of the diagnosis, no cysts were found that could be the cause of lactorrhea, you can sleep peacefully. In rare cases, drug therapy is indicated.
►Is it true that the vagina expands after childbirth and does not return to its previous shape?
– Yes, the baby passes through the natural birth canal, it certainly changes. The vagina is becoming wider; nowadays there is even a special medical term - relaxed vagina syndrome, “wide vagina syndrome” in common parlance.
Every woman and man has their own concept of comfort and norm, and if an intimate situation does not suit a woman, then a gynecologist and fitness center will help her with an emphasis on training the pelvic floor muscles. At home, it is possible to perform the same Kegel exercises, but it is important to do it correctly, completely eliminating the work of the anterior abdominal muscle. A gynecologist can teach you these exercises. 90% of the patients I work with do them, unfortunately, incorrectly.
Nowadays there are also many vaginal devices to solve the problem of a relaxed vagina. By the way, excellent Belarusian “gadgets” are also registered in our country.
Another simple solution to the problem is laser vaginal remodeling. This is already a field of aesthetic gynecology in which only certain laser energy is used: the equipment must be certified to work with the bladder and vaginal mucosa.
►A gynecologist always sees whether a woman has given birth or not?
- Yes. For us, obstetricians-gynecologists, there are obvious signs that allow us to distinguish a woman who has given birth from a nulliparous woman, and they remain with the woman forever. One of the main ones is the state of the uterine pharynx: in those who have given birth, it becomes slit-like, the cervix takes on a cylindrical shape (in those who have not given birth, it is conical), and the folding of the vaginal mucosa also changes.
►How do pregnancy and childbirth affect the spine?
– If a woman was somatically healthy before pregnancy, she will be healthy after. The birth of a child does not have a bad effect on the condition of the spinal cord, spinal column and nerve endings.
►What about your weight? Many people get fat and then can’t lose weight.
– Women who are lactating try to eat more protein foods and generally eat more so that the baby gets more nutrients and amino acids. At the same time, they usually move less, paying more attention to the baby, and accordingly, they take on certain shapes.
But, as soon as lactation ends, the hormonal balance in the body is restored. When a woman tries to pay more attention to herself, goes to the gym or does exercises at home, her weight gradually returns to normal. You need to put in effort and effort, the kilograms won’t go away on their own. And at the same time, there are exceptions, for example constitutional features.
►They also often say that teeth suffer a lot.
- A controversial issue. If a woman took calcium supplements, vitamins, or foods with sufficient trace elements and calcium during pregnancy, there should be no problems, as dentists say.
But there were no cases of tooth loss in my practice. Even at the stage of pregnancy planning, a woman is recommended to treat chronic foci of infection, that is, to sanitize the oral cavity.
TEST PRINCIPLE
A sample of vaginal discharge, taken with a vaginal swab, is placed in a test tube with a solvent. The solvent extracts the sample from the swab for 1 minute, after which the swab is discarded. An AmniSure test strip (dipstick, lateral flow device) is then immersed in the tube. The sample contents move from the immersion area to the test area of the strip. The test result is visually read after 5-10 minutes by the presence of one or two bands.
The test uses the principle of immunochromatography to detect human placental α1-microglobulin (PAMG-1, placental α1-microglobulin). PAMG-1 was chosen for this purpose due to its unique characteristics: high content in amniotic fluid, low level in the blood and extremely low (50-220 pg/ml) concentration in the secretion of the vagina and cervix with intact membranes.
The test uses highly sensitive monoclonal antibodies that detect even the smallest amount of protein that appears in the vagina after water leakage begins. To minimize the frequency of false negative results, the test uses a specially selected combination of two monoclonal antibodies, which ensures the test sensitivity threshold is optimally low. The background level of PAMG-1 in vaginal secretions is extremely low (0.05 - 0.005 mg per drop). The threshold concentration of PAMG-1, which can be determined using this combination of antibodies, is 50 - 220 pg (i.e. 0.05 - 0.22 ng) in 1 ml of vaginal secretion. The sensitivity threshold of the test was specially increased 20 times to 5 - 7 ng/ml, which increased the accuracy of the test to 99% by eliminating false positive and false negative results.
During the procedure, PAMG-1 from the sample sequentially binds to monoclonal antibodies A (A-Mab), conjugated to a label, and then to monoclonal antibodies B (B-Mab), immobilized on an insoluble carrier. When A-Mab antibodies come into contact with PAMG-1 in the immersion zone, they capture PAMG-1 and transport it to the test zone. The dipstick test zone has a strip where the immobilized B-Mab antibodies are located. B-Mab antibodies “meet” PAMG-1 brought by mobile A-Mab antibodies from the immersion zone. This encounter immobilizes the PAMG-1/A-Mab complex, resulting in a brownish-yellow coloration in the area of the test strip. This staining results from the presence of gold dye attached to the A-Mab antibodies. The presence of such staining indicates leakage of amniotic fluid. The second (control) strip is made in order to check whether the test system “works” correctly. This line appears when rabbit immunoglobulin G against mouse antigens combines with mouse antibodies with gold dye. If a reaction occurs, a control line appears.
Interference Research
Vaginal infections or urine do not affect the results of the AmniSure test. Careful study and analysis showed that during vaginal infections, the concentration of PAMG-1 in the vagina never exceeded 3 ng/ml. The sensitivity level of AmniSure is 5-7 ng/ml, excluding interference due to infections. The concentration of PAMG-1 in sperm does not exceed 4 ng/ml. The PAMG-1 concentration of sperm in the vagina is even lower due to the effect of reducing the concentration by 4 times when sperm enters the vagina. Therefore, no interference with sperm was observed during the development and testing of the AmniSure test. The same applies to urine. Fifteen urine samples were tested for PAMG-1 concentrations by ELISA. The sensitivity of the ELISA was 0.5 ng/ml. The AmniSure test was used in parallel. Samples were obtained from pregnant women between 25 and 40 weeks' gestation. Both methods gave negative results. PAMG-1 was not detected in any case.
LIMITATIONS OF THE TEST
- The AmniSure kit is intended for in vitro diagnostics of the human amniotic fluid protein PAMG-1 in the vaginal secretions of pregnant women. The test should be used to evaluate women with suspected leakage of amniotic fluid or clinical symptoms of conditions accompanied by leakage of membranes.
- To ensure proper operation of the test system, all provisions of this instruction must be strictly followed.
- Each test kit is a single use kit and should not be reused.
- The results of this test are qualitative. It should not be used for quantitative interpretation of results.
- If there is heavy bleeding (the polyester end of the swab is red), the test may not work properly and is not recommended for use in such cases. If only trace amounts of blood are present (the swab is pinkish), the test functions normally.
- In extremely rare cases, when the sample is taken 12 hours or more after the rupture, false negative results may occur.
- The test should be used no earlier than 6 hours after removing any disinfectant solutions or medications from the vagina.
“No one will tell you in advance what awaits you”
►Are all the consequences of childbirth reversible?
– Almost everything, but it depends on the woman’s personal aspirations. After all, if, for example, a woman has stretch marks on the skin of her abdomen and chest and they do not bother the woman, then there is no question. But it is clear that they will not disappear on their own. A wide vagina will also not correct itself, the mammary glands will not become what they were before.
►Does the presence of complications depend on the woman’s health status or on her behavior during pregnancy?
– 50% depend on physical health before pregnancy and 50% depend on how the pregnancy and postpartum period proceed. After giving birth, a woman is recommended to definitely come to an appointment with an obstetrician-gynecologist in two weeks. The doctor will assess the condition of the woman’s birth canal, perineum, sutures, cervix, vaginal walls, and, if necessary, perform an ultrasound of the uterus and appendages.
It is also important and necessary to visit a doctor two months after giving birth.
►Is it possible to find out in advance what the consequences are?
– Medicine is the most exact science after theology. No one can know what will happen. It is important for a woman to listen to the recommendations of her doctor and her body.
►What to do to minimize the chances of complications?
– Consciously plan your pregnancy, visit your doctor regularly, eat a balanced diet, play sports, practice special exercises for the pelvic floor muscles, go for walks, treat yourself to spa treatments, massages, read interesting literature and just love yourself. I would like you to understand: pregnancy is not a disease, it is a physiological state of the female body.
Sources
- Cobo T., Aldecoa V., Holeckova M., Andrys C., Filella X., Jacobsson B., Kacerovsky M. A Rapid Amniotic Fluid Interleukin-6 Assessment for the Identification of Intra-Amniotic Inflammation in Women with Preterm Labor and Intact Membranes // Fetal Diagn Ther - 2021 - Vol - NNULL - p.1-6; PMID:33902036
- Song B., Cheng Y., Cao D., Liu N., Guan H., Du L., Zhang H., Liang Y., Xian J., Sun X. Generation of induced pluripotent stem cell line GZHMCi006-A from amniotic fluid-derived cells with deletion 14q syndrome. // Stem Cell Res - 2021 - Vol53 - NNULL - p.102315; PMID:33894549
- Sánchez JM., Gómez-Redondo I., Browne JA., Planells B., Gutiérrez-Adán A., Lonergan P. MicroRNAs in amniotic fluid and maternal blood plasma associated with sex determination and early gonad differentiation in cattle. // Biol Reprod - 2021 - Vol - NNULL - p.; PMID:33889937
- Bicocca MJ., Qureshey EJ., Chauhan SP., Hernandez-Andrade E., Sibai BM., Nowlen C., Stafford I. Semiquantitative Assessment of Amniotic Fluid Among Individuals With and Without Diabetes Mellitus. // J Ultrasound Med - 2021 - Vol - NNULL - p.; PMID:33885190
- Antounians L., Catania VD., Montalva L., Liu BD., Hou H., Chan C., Matei AC., Tzanetakis A., Li B., Figueira RL., da Costa KM., Wong AP., Mitchell R., David AL., Patel K., De Coppi P., Sbragia L., Wilson MD., Rossant J., Zani A. Fetal lung underdevelopment is rescued by administration of amniotic fluid stem cell extracellular vesicles in rodents. // Sci Transl Med - 2021 - Vol13 - N590 - p.; PMID:33883273
- Singh P., Kumar M., Basu S. Gastric Lavage for Prevention of Feeding Intolerance in Neonates Delivered Through Meconium-Stained Amniotic Fluid: A Systematic Review and Meta-Analysis. // Indian Pediatr - 2021 - Vol - NNULL - p.; PMID:33864449
- Matsunaga S., Masuko H., Takai Y., Kanayama N., Seki H. Fibrinogen may aid in the early differentiation between amniotic fluid embolism and postpartum haemorrhage: a retrospective chart review. // Sci Rep - 2021 - Vol11 - N1 - p.8379; PMID:33863968
- Martins JG., Kawakita T., Gurganus M., Baraki D., Jain P., Papageorghiou AT., Abuhamad AZ. The influence of maternal body mass index on interobserver variability of fetal ultrasound biometry and amniotic fluid assessment in late pregnancy. // Ultrasound Obstet Gynecol - 2021 - Vol - NNULL - p.; PMID:33836119
- Nuge T., Liu X., Tshai KY., Lim SS., Nordin N., Hoque ME., Liu Z. Accelerated wound closure: Systematic evaluation of cellulose acetate effects on biologically active molecules release from amniotic fluid stem cells. // Biotechnol Appl Biochem - 2021 - Vol - NNULL - p.; PMID:33826152
- Mitrani MI., Bellio MA., Sagel A., Saylor M., Kapp W., VanOsdol K., Haskell G., Stewart D., Abdullah Z., Santos I., Milberg J., Arango A., Mitrani A ., Shapiro G.C. Case Report: Administration of Amniotic Fluid-Derived Nanoparticles in Three Severely Ill COVID-19 Patients. // Front Med (Lausanne) - 2021 - Vol8 - NNULL - p.583842; PMID:33816515
“In fact, the number of postpartum depressions is negligible”
►When does the menstrual cycle return?
– This is very individual. If a woman lactates regularly and breastfeeds the baby on a schedule every 3-6 hours, the menstrual cycle may resume only after the end of lactation. This is due to high levels of prolactin and low levels of pituitary hormones.
►Is it normal if after the birth of a child you don’t want sex for a long time?
– This is not normal, but it is due to the peculiarity of a woman’s endocrine changes during the postpartum period. A high level of prolactin in the blood suppresses gonadotropins, and the limbic system works according to its own rules, and it is the one responsible for pleasure.
That is, the instinct of motherhood suppresses the instinct of intimacy, and a woman has a different dominant. The end of this period and the return of intimacy is often associated with the fact that children are growing up and need less attention, but in fact she does not want sex not because she is tired, but for endocrine reasons. Evidence-based endocrinology explains this.
And this can last up to three years or more, but the return of libido will definitely happen, the time for each woman is individual.
►What if it doesn’t go away for a very long time?
– Then it is necessary to perform a series of studies and contact a gynecologist-endocrinologist or gynecologist-esthetician to find the problem and solve it.
►Women often change their taste preferences during pregnancy. Is it normal if they do not recover after the birth of a child?
– Everything is restored to normal, I don’t really want chalk and cucumbers. Typically, all food fads end by 16 weeks of pregnancy, when a sufficient amount of the hormone, placental lactogen, is formed.
If a woman has given birth and her previous preferences have not returned, she should consult a psychotherapist and gastroenterologist.
►Lately, people are increasingly talking about postpartum depression. Does pregnancy often have such a bad effect on your psychological state?
– Minor state, sadness, fatigue, stress are often masked by postpartum depression. In fact, the number of postpartum depressions in the population is negligible. I have had such patients, and this condition cannot be compared with anything else: women give up, they are helpless, and this helplessness does not depend on the woman herself. Her hormonal metabolism and the amount of endorphins change. This is a profound change at the level of the neuroendocrine system, but fortunately it is a rare complication.
During lactation, the trust hormone oxytocin is produced. And when a woman is lactating, she produces more endorphins, and she is protected by nature from depression. But, of course, if a woman is constantly alone, she does not have the support of her husband or family, if she is constantly tired, she is not given attention, the usual hypochondriacal syndrome develops, which can lead to depression.
Stability of results
AmniSure is a test system, the results of which must be read 5 - 10 minutes after immersing the test strip in the tube. The stability of the test was studied in a lot containing 1000 sets. Purified PAMG-1 was used at concentrations ranging from 10 to 5 ng/ml in saline. Duration and stability of results were also determined. After the result became visible (stripes appeared in the test area), it remained stable for at least 5 minutes. The stability of the test was observed even at very low concentrations of PAMG-1 (5-10 ng/ml). If the concentrations were higher, the strips remained stable for hours after the test. Therefore, the stability of the test is 5 minutes and the test time is 10 full minutes.
Table 1
Stability study results
| Concentration of purified PAMG-1 in saline (ng/ml) | Time elapsed before color appears in the test area |
| 10 | ~2.5 min |
| 5 | ~5.5 min |