Symptoms and manifestations
In the early stages of cervical cancer and with precancerous changes, the woman is not worried about anything. Typically, the occurrence of symptoms indicates that the tumor has already grown into neighboring organs.
Manifestations of the disease are nonspecific and can occur in other pathologies, for example, urogenital infections:
- Heavy, prolonged periods. This symptom is important if your periods have recently changed, if they were previously normal.
- Vaginal bleeding between periods, after sexual intercourse, after menopause.
- Unusual vaginal discharge: copious, pink, with an unpleasant odor.
- Pelvic pain during sexual intercourse.
In most cases, these manifestations are not caused by cancer. But there is always a risk, albeit small, so if the first symptoms occur, you should visit a doctor.
In later stages, the listed symptoms are joined by such signs as sudden causeless weight loss, pain in the lower back and legs, a constant feeling of fatigue, pathological bone fractures (a sign of bone metastases), and urine leakage from the vagina.
Complications after surgery
- a woman is unable to become pregnant (except for intervention in the form of conization);
- possible inability to have sexual intercourse;
- deterioration of condition due to chemotherapy and radiation therapy;
- hormonal imbalance, if the doctor is forced to remove the ovaries.
Complications in case of refusal of surgery:
- bleeding;
- fistulas between organs;
- thrombosis;
- compression of the ureters with subsequent impairment of renal function.
Causes
It is difficult to name the exact causes of cervical cancer. But there are known risk factors that increase the likelihood of cervical cancer.
The most significant risk factor is human papillomavirus infection. According to various sources, up to 99% of cervical cancer cases are associated with human papillomaviruses (HPV). Up to 80% of women become infected with this pathogen during their lifetime. There are about 100 types of HPV, of which 30–40 are sexually transmitted, and only 165 increase the risk of cancer. But this does not mean that they are guaranteed to cause cancer. Virus types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56 and 58 are classified as highly oncogenic, 6, 11, 42, 43 and 44 as low-oncogenic. The most common causes of cervical cancer are HPV types 16 and 18. The transformation zone is most vulnerable to them (see below). In addition to cervical cancer, HPV causes malignant tumors of other organs of the reproductive system, pharynx, oral cavity, and anal canal.
Other risk factors:
- Weakened immune system
. If a woman’s immunity works normally, her body gets rid of the papilloma virus within 12–18 months. But if the defenses are weakened, the infection persists longer and increases the risk of cancer. - Promiscuous sexual intercourse.
Frequently changing partners increases the likelihood of contracting HPV. - Obstetric history . If a woman has had three or more pregnancies, or if her first pregnancy was before age 17, the risk is doubled.
- Heredity . If a woman's mother or sibling is diagnosed with cervical cancer, her risk is 2-3 times higher.
- Smoking . A bad habit also doubles your risks.
- Use of oral contraceptives for 5 years or longer. Once you stop taking them, the risks decrease over several years.
Types of cervical cancer
To understand the classification of cervical cancer, first of all you need to understand a little about its anatomical and histological structure. The cervix is 2–3 cm long and consists of two parts:
- The vaginal part (exocervix) protrudes into the vagina; this is what the gynecologist sees on the speculum during an examination. The mucous membrane of the endocervix consists of stratified squamous epithelium.
- The cervical canal (endocervix) is located inside and connects the vagina to the uterus. It is lined with columnar epithelium.
The border between the vaginal part and the cervical canal is called the transformation zone.
In 70–90% of cases, malignant tumors of the cervix are squamous cell carcinoma. It develops from stratified squamous epithelium. Most often, malignant degeneration occurs in the transformation zone. Depending on how the tumor tissue looks under a microscope, squamous cell carcinoma of the cervix is divided into keratinizing and non-keratinizing:
- Keratinizing squamous cell carcinoma of the cervix
is so called because the cells that make it up tend to become keratinizing. They are large, irregular in shape, and have a relatively low division intensity. Microscopic examination reveals formations called keratohyaline granules and “cancer pearls.” - In nonkeratinizing squamous cell carcinoma of the cervix,
the cells are not prone to keratinization. They are large, have the shape of an oval or polygon, and reproduce more intensively.
Depending on how much the cancer cells differ from normal ones, malignant tumors of the cervix are divided into highly, moderately and poorly differentiated. The latter behave the most aggressively. Squamous cell keratinizing carcinoma is classified as a mature form and occurs in approximately 20% of cases. Non-keratinizing cancers are tumors of medium maturity, they account for 60-70%. The immature form is a poorly differentiated cancer.
In other cases, cervical cancer is represented by adenocarcinoma. It develops from glandular cells that produce mucus. This type of malignant tumor has become more common over the past 20–30 years.
Adenosquamous carcinomas are much less common These tumors combine features of squamous cell carcinoma and adenocarcinoma. To determine the type of malignant tumor, a biopsy must be performed.
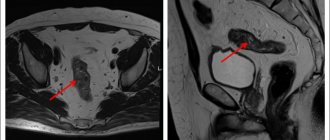
Distribution in the body
As cervical cancer grows, it spreads to neighboring organs. First of all, regional lymph nodes and surrounding tissue (parametrium) are affected.
The upper third of the vagina is often affected, which is not surprising, since it is in direct contact with the cervix. The spread of cancer cells occurs directly when a tumor grows into the vagina, lymphogenously (through lymphatic vessels), by contact implantation - where the vaginal wall comes into contact with the tumor. The body of the uterus is also involved.
The spread of tumor cells into the rectum, bladder and ureters, as a rule, occurs by contact.
Distant metastases most often occur in the retroperitoneal lymph nodes, lungs, bones, and liver. In less than 1% of cases, metastasis occurs in the spleen, kidneys, and brain.
Price list
*Note:
Prices are indicated for foreign citizens. Citizens of the Republic of Belarus can receive medical services without charging a fee. Read more...
*Prices in Bel. rub. *You can view all types of services and exact prices on the page
| Procedure name | Price in Belarusian rubles |
| Wide local excision of vulvar tumor | 466 |
| Wide local excision of vaginal tumor | 708 |
| Unilateral adnexectomy | 578 |
| Bilateral adnexectomy | 1 025 |
| Bilateral adnexectomy, omentectomy | 1 156 |
| Bilateral adnexectomy, resection of the greater omentum, surgical staging | 1 268 |
| Subcutaneous vulvectomy | 727 |
| Separate diagnostic curettage | 186 |
| Hysterectomy without appendages | 1 454 |
| Panhysterectomy | 1 752 |
| Panhysterectomy, omentectomy | 2 181 |
| Panhysterectomy, pelvic peritonectomy, omentectomy | 4 362 |
| Wertheim operation (panhysterectomy with pelvic lymphadenectomy) | 3 206 |
| Wertheim operation with omentectomy | 3 486 |
| Wertheim operation (panhysterectomy with pelvic lymphadenectomy) with retroperitoneal lymphadenectomy | 4 362 |
| Vulvectomy with femoroinguinal lymphadenectomy through separate incisions | 3 095 |
| Vulvectomy with femoroinguinal-iliac lymphadenectomy through separate incisions | 3 542 |
| Monoblock vulvectomy with bilateral femoral-inguinal lymphadenectomy with vulvar plastic surgery using a combined method | 4 921 |
| Vulvectomy with femoroinguinal lymphadenectomy through separate incisions and vulvar plastic surgery with bilateral island infero-gluteal flaps | 4 921 |
| Vulvectomy with femoroinguinal lymphadenectomy through separate incisions and vulvar plastic surgery with a TRAM flap | 4 940 |
| Operation Sturmdorf | 1 025 |
| Knife biopsy of the cervix | 130 |
Diagnosis of cervical cancer
High mortality rates from cervical cancer are associated with late detection of the disease: in 35–40% of cases in Russia, the diagnosis is first made to patients with stages III–IV of the disease.
Since cervical cancer can be asymptomatic for a long time, timely diagnosis is only possible with regular special examinations by a gynecologist.
According to research by scientists from Keele University (UK), there is no age limit for regular screening for cervical cancer. Contrary to popular belief, women remain at risk of developing a tumor even after 65 years of age, since the human papillomavirus, which in the vast majority of cases causes cancer, can enter the body during the period of sexual activity, “dormant” for a long time and lead to to the development of cancer.
Tests for human papillomavirus
Carrying out a PCR analysis for the presence of human papillomavirus can only detect the presence of the corresponding virus in the body. To determine its ability to provoke the development of cervical cancer (oncogenicity) and the degree of activity of the virus in the body, additional studies, also carried out by PCR, are required.
But even identifying HPV of high oncogenic risk does not turn cervical cancer into something fatal. Firstly, the disease may not develop at all. Secondly, modern technologies make it possible to identify this form of cancer at the earliest stages and successfully treat it, preventing its transformation precancerous changes into cancer itself. Therefore, positive HPV test results should only be considered as a basis for regular follow-up with a gynecologist familiar with effective management algorithms for patients at risk.
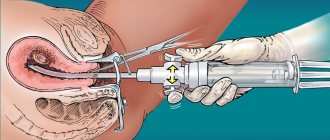
Gynecological examination with colposcopy
Sometimes cervical cancer is detected directly during an examination in a gynecological chair. However, this is how, as a rule, an advanced oncological process is determined. In contrast, the early stages of the disease usually pass without any noticeable changes, so additional tests are used to diagnose cervical cancer in a timely manner. During a colposcopy, the vaginal part of the cervix is examined using a colposcope, an instrument that resembles binoculars with a light source.
Cytological smear (PAP test, Papanicolaou test)
The classic method of cytological examination of the cervix, or PAP test, involves carefully “scraping” the material with a special spatula from the surface of the organ and “smearing” it on a glass slide. This method was developed at the beginning of the last century, in 1923. For its time, the Pap test showed excellent results, but years of use revealed a number of shortcomings of the method. The selectivity of cell capture and their uneven distribution on the glass can significantly distort the results of cytological analysis. Thus, the sensitivity of the method is only 85–95%, and in the early stages of the disease, characterized by a small number of cancer cells, this figure may be even lower.
Liquid cytology method
The liquid cytology method involves the use of a special “brush”, which allows you to obtain material for research from the entire surface of the cervix, and not from its individual fragments, as happens during a Pap test.
Then the material from the “brush” goes into a special solution, is processed in a special apparatus, and only after that is evenly applied to a glass slide. All this increases the sensitivity of the method to almost 100% and eliminates the possibility of errors typical of the Pap test.
Make an appointment with an oncologist-gynecologist
Also, the material obtained during this analysis can be used to determine HPV activity, which is an important prognosis factor and can influence treatment tactics. And finally, the solution with the cells in it is suitable for analysis to determine a special protein (P16ink4a), which appears in the cells even before the oncological process begins. Thus, the liquid cytology method can not only detect cervical cancer, but also warn about an increased risk of its development. After one single procedure, the doctor has the results of three accurate and informative tests at his disposal, allowing him to determine the tactics and strategy for managing a particular patient.
For preventive purposes (in the absence of complaints), these tests are recommended to be carried out once a year.
Cervical cancer treatment
Based on the clinic’s experience, it is possible to preserve the uterus and the possibility of childbearing with precancerous changes in the cervix. For cervical cancer, radiation therapy and surgical treatment - extended extirpation of the uterus and appendages - are equally widely used.
Treatment depends on the stage of the disease. In the early stages of cervical cancer, surgical treatment is preferred. During the operation, the uterus is removed. Sometimes the operation must be supplemented by removal of the pelvic lymph nodes. The issue of removing the ovaries is decided individually; with an early stage of the tumor in young women, it is possible to leave the ovaries. No less important is radiation treatment. Radiation therapy can either complement surgical treatment or be an independent method. In the early stages of cervical cancer, the results of surgical and radiation treatment are almost the same. Chemotherapy can be used to treat cervical cancer, but unfortunately, chemotherapy options for this disease are significantly limited.
At stage 0
Cancer cells do not spread beyond the surface layer of the cervix. Sometimes this stage is even considered a precancerous condition. Such a tumor can be removed in different ways, but with organ-preserving interventions, the risk of recurrence remains in the future, so regular cytological smears are indicated after surgery.
Treatment options for squamous cell carcinoma of the cervix, stage 0:
- Cryosurgery is the destruction of a tumor using low temperature.
- Laser surgery.
- Conization of the cervix - excision of a cone-shaped area.
- Loop electroconization of the cervix.
- Hysterectomy. It is also used in case of relapse of a malignant tumor after the above interventions.
Treatment methods for cervical adenocarcinoma, stage 0:
- Hysterectomy.
- In some cases, if a woman plans to have children, conization may be performed. In this case, an important condition is a negative resection margin according to biopsy data. Subsequently, the woman should be observed by a gynecologist, and after childbirth a hysterectomy is performed.
The choice of treatment method is always made individually by the attending physician.
At stage 1a
- microinvasive cervical cancer - extirpation of the uterus and appendages is performed.
In cases where the tumor grows into the blood and lymphatic vessels, removal of the pelvic lymph nodes is also indicated. If a woman plans to have children, organ-conserving surgery is possible. In stage Ib
—the cancer is limited to the cervix—external or intracavitary irradiation (brachytherapy) is performed, followed by extended extirpation of the uterus and appendages. In some cases, surgery is initially performed, followed by external gamma radiotherapy.
At stage 2
cervical cancer - involvement of the upper part of the vagina, possible transfer to the body of the uterus and infiltration of the parametrium without transfer to the pelvic wall - the main method of treatment is radiation therapy. Chemotherapy may also be prescribed, usually with the drug cisplatin or its combination with fluorouracil. In this case, surgical treatment is rarely performed.
In the 3rd stage of cervical cancer - transition to the lower part of the vagina, infiltration of the parametrium with transition to the pelvic bones - radiation therapy is indicated.
At stage 4
(transition of cancer to the bladder, rectum or distant metastasis) only palliative radiation is used. In patients with advanced stages of cervical cancer with metastases, treatment is palliative, and chemotherapy may be used. In most cases, the chemotherapy regimen involves using one of the platinum drugs (carboplatin or cisplatin) in combination with gemcitabine (Gemzar), paclitaxel (Taxol), or topotecan.
Indications for referral to colposcopy
- High degree of abnormalities detected by cytology.
- Persistent low grade or unsatisfactory cytology results.
- Cytology showed the presence of AGUS (atypical glandulocytes of undetermined significance).
- Suspicious appearance of the cervix during visual examination.
Basic instruments for colposcopy
- Colposcope with 6-16 times magnification
- Bright lighting with adjustable position
- Focal length 250mm for instruments
- Solutions:
- saline solution, 3-5% acetic acid, Lugol's solution
Colposcopic picture
Prevention
One of the main risk factors for cervical cancer is the human papillomavirus. Therefore, preventive measures should primarily be aimed at preventing infection:
- Promiscuous sexual intercourse is undesirable , especially with men who have had many partners. This does not protect against infection 100%, but it still helps greatly reduce the risks.
- Condoms will help protect not only from HPV, but also from HIV infection . They also do not provide one hundred percent protection, because they cannot completely eliminate contact with infected skin.
- HPV vaccines are a good means of prevention, but they only work if the woman is not yet infected. If the virus has already entered the body, the vaccine will not help. Girls begin to be vaccinated at the age of 9–12 years.
The second risk factor that is associated with lifestyle and which can be influenced is smoking. If you suffer from this bad habit, it is better to give it up. Screening is of great importance - it helps to detect precancerous changes and cervical cancer in the early stages. You need to regularly visit your gynecologist for examinations, undergo a PAP test and get tested for HPV.
The main prognostic factor for the survival of patients with cervical cancer is the extent of the process. Therefore, the most effective remedy against the development of cancer is regular preventive examinations by specialists.
HPV PAP tests
To increase the effectiveness of cervical screening, especially after 30 years, it is recommended to simultaneously perform an HPV test and a PAP test (co-testing), the so-called HPV-PAP test.
- HPV-PAP test (set of tests: HPV extended with determination of the amount and type of virus + PAP test)
- HPV-PAP test liquid (set of tests: HPV extended with determination of the amount and type of virus + PAP test liquid)
In terms of information content, the liquid HPV-PAP test has an advantage.
Forecast
The approximate forecast is determined based on statistics. Among women diagnosed with cervical cancer, the percentage of survivors is calculated over a specified period of time, usually five years. This figure is called five-year survival rate. It depends on the stage at which the cancer was detected. The earlier cancer is diagnosed and treatment started, the better the prognosis:
- For localized tumors (cancer does not spread beyond the cervix, corresponds to stage I), the five-year survival rate is 92%.
- For tumors that have spread to nearby structures (stages II, III and IVA) - 56%.
- For metastatic cancer (stage IVB) - 17%.
- The average five-year survival rate for all stages of cervical cancer is 66%.
Despite low five-year survival rates, metastatic cancer is not a reason to give up. There are treatment methods that help slow down the progression of the disease, prolong life, and cope with painful symptoms. Doctors from the Euroonko clinic network know how to help.