A small paired organ, the adrenal gland, is responsible for vital processes in the body. Fifteen cubic centimeters of glandular tissue produce many of the most important hormones without which life is impossible: aldosterone, corticosterone, deoxycorticosterone, cortisol, androgens, adrenaline and norepinephrine. Blood pressure, inflammatory, allergic and immune reactions, and secondary sexual characteristics depend on the functioning of the adrenal glands.
Adrenocortical cancer is a fairly rare malignant tumor with an aggressive course. The tumor develops in the superficial layer - the cortex, where all hormones are synthesized, except adrenaline and norepinephrine - the medulla, covered by the cortex, is responsible for their production. Therefore, the tumor itself often begins to produce hormones in incorrect quantities, causing specific syndromes, sometimes obvious, sometimes hidden.
There are no exact statistics for adrenal cancer; it is grouped together with other tumors, but it is estimated that there are about two cases of cancer per million of the population. Without taking into account the size of the cancer tumor, about 40% survive five years, after radical treatment - 60% of patients. A small tumor of the adrenal gland, naturally, gives hope to almost seven out of ten patients to live a long time; with large cancer with metastases, no more than 10% survive the five-year mark. The tumor's ability to produce hormones negatively affects life expectancy.
The adrenal glands are a “factory” of hormones
The adrenal glands are small paired organs located, as the name suggests, above the kidneys. Their main task is to produce hormones - substances that regulate all vital processes in the body. For example, glucocorticoid hormones are responsible for metabolism, mineralocorticoid hormones are involved in water and salt metabolism, androgens and estrogens are analogs of sex hormones, adrenaline and norepinephrine are stress hormones. The adrenal glands are surrounded by a dense connective tissue capsule and are embedded in adipose tissue. Bundles of the capsule (trabeculae) penetrate into the internal parts of the gland, forming partitions that divide the organ into layers and zones. The adrenal glands are, in addition, surrounded by the renal fascia, to which they are connected very firmly. The right adrenal gland has the shape of a truncated cone, flattened from front to back. From the front it resembles a triangle with rounded corners - “Napoleon's tricorne”. The apex of the left adrenal gland is flattened and is shaped like a crescent. Front view of isolated right and left adrenal glands
How does oncology develop?
Cancer begins with the appearance in the body of just one altered cell, which is formed due to hereditary characteristics or various diseases, multiplies and creates a tumor. Most of these cells detect and destroy the immune system, but some of them manage to hide from the attention of our natural defenses or resist it. They enter the circulatory or lymphatic system. The lymphatic system complements the cardiovascular system. The lymph circulating in it - the intercellular fluid - washes all the cells of the body and delivers the necessary substances to them, taking away waste. Lymph nodes located throughout its network, acting as “filters,” identify and neutralize dangerous substances. systems., with their help they spread throughout the body, become established in other tissues and create metastases - additional foci of the disease.
What is the adrenal gland, why do we need it and how does oncology develop in it?
Each adrenal gland consists of two structures.
Outside the organ is the cortical layer
, in which most tumors arise. It produces important hormones:
- Cortisol
– helps the body cope with stress. - Aldosterone
– regulates blood pressure and the amount of salt in the blood. - Androgens
, which can be converted to other forms of hormones: - estrogens necessary for the proper functioning of the ovaries, uterus, vagina and mammary glands,
- as well as testosterone, which is involved in the production of sperm, affects the development of bone and muscle tissue in men.
In its inner part there is a medulla
, which is a continuation of the nervous system. It produces adrenaline, which helps us quickly respond to stress and extreme situations. When it is released, the pulse quickens, blood flow in the body is redistributed, minor vessels narrow, and important ones supplying the brain and heart expand. Dangerous neoplasms also arise in this area of the organ – neuroblastomas, which develop from nerve cells.
Doctors distinguish 2 types of adrenal cortex tumors:
- Adenomas
: benign, which means they do not grow into surrounding tissues and do not spread throughout the body. As a rule, their size does not exceed 5 centimeters in diameter, and most of their owners do not have any symptoms and are not aware of their disease. Some are discovered by chance during testing for other health problems. - Carcinomas
are cancers, which we will discuss in detail in this text.
All types of diagnostics are important - from examination to ultrasound
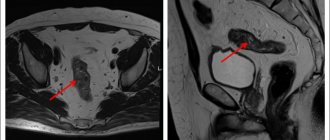
The diagnostic complex for studying the pathology of the adrenal glands should include: clinical examination, laboratory (clinical, biochemical, hormonal), instrumental and pathomorphological examination methods. A clinical examination and interview of patients is carried out to identify signs characteristic of various symptom complexes of adrenal pathology. In laboratory diagnostics to identify pathology of the adrenal glands, the levels of adrenocorticotropic hormone, cortisol, aldosterone, dehydroepiandrosterone sulfate (DHEA sulfate), the activity of renin and angiotensin in the blood plasma, and the daily excretion of adrenaline, norepinephrine and vanillylmandelic acid in the urine are most often determined. For the purpose of topical diagnosis, ultrasound with color Doppler scanning, computed X-ray tomography (), magnetic resonance imaging (MRI) is used; in complex cases, for the purpose of differential diagnosis - angiography or selective venography with separate blood sampling. In some cases, to verify the morphological structure of adrenal formations, aspiration puncture with a thin needle is performed under ultrasound or CT control with cytological examination.
Kidney ultrasound
- Cost: 2,700 rub.
More details
Why do “flies” fly before my eyes?
Clinical manifestations of primary hyperaldosteronism (PHA): arterial hypertension (headache, dizziness, appearance of “floaters” before the eyes); disorders of neuromuscular conduction and excitability (muscle weakness, parasthesia, convulsions, bradycardia); changes in renal function (polyuria, polydipsia, nocturia). These signs are not always present simultaneously; An oligosymptomatic and even asymptomatic course of the disease is often observed. Approximately two-thirds of all cases of PHA are caused by aldosteroma. Another possible cause of PHA is nonadenomatous bilateral adrenal hyperplasia, which occurs in one third of patients with symptoms of idiopathic primary hyperaldosteronism. The main treatment method for aldosteroma and nodular adrenal hyperplasia is surgery - removal of the altered adrenal gland along with the tumor (adrenalectomy). Performing organ-saving operations (tumor enucleation, adrenal resection) by most surgeons operating on endocrine organs is considered inappropriate due to the high rate of relapse of tumors in the remaining tissue (up to 50%). Already in the immediate postoperative period, in most cases, normalization of blood pressure, a decrease in the concentration of aldosterone in plasma, a gradual increase in renin activity, and normalization of potassium are noted.
How can we help with adrenal tumors?
- We offer compulsory medical insurance treatment in accordance with international standards. In each case, we hold a consultation with the participation of oncologists, surgeons, radiologists and chemotherapists to select effective treatment.
- We adhere to fasttrack surgery standards -
competent preparation for surgery to remove adrenal tumors, gentle intervention techniques, active recovery, individual selection of anesthesia. This shortens the recovery time and reduces the risk of complications.
"Crisis" tumor
Pheochromocytoma is a tumor of chromaffin cells that produces excess amounts of catecholamines (adrenaline, norepinephrine and dopamine). Pheochromocytoma may develop from chromaffin tissue of the adrenal medulla (90%) and may be non-adrenal in location. The disease occurs at any age. The main symptoms of the disease in the vast majority of patients are arterial hypertension, hypermetabolism and hyperglycemia. The classic clinical picture is considered to be periodic rises in blood pressure, accompanied by some vegetative symptoms, reminiscent of the effects of the administration of adrenaline or norepinephrine. In the initial period of the disease, these attacks, or crises, occur rarely - once every few months or even years. Over time, the frequency, duration, and severity of attacks usually increase. The onset of a crisis is quite often characterized by the appearance of unaccountable fear, sometimes a feeling of chilliness, paresthesia, marbling or pallor of the skin. Sometimes, on the contrary, there is pronounced redness of the facial skin, shiny eyes, dilated pupils, and frequent urge to urinate. A crisis can begin with paresthesia, convulsions, and vasoconstriction of the extremities. The crisis ends as suddenly and quickly as it began. Blood pressure returns to its original values, the pallor of the skin gives way to redness, and sometimes profuse sweating and excessive secretion of the salivary glands are observed. After an attack, general weakness and weakness persist for a long time. The diagnosis of pheochromocytoma is established when elevated amounts of catecholamines or their metabolites are detected in 24-hour urine. The most reliable is urine analysis collected within 3 hours after the attack. The accuracy of the method reaches 95%. It is recommended to conduct such studies several times. Tumor detection is usually carried out using ultrasound, CT and MRI. If the diameter of the tumor is more than 10 mm, then the sensitivity of these methods approaches 100%. Ultrasound is important in establishing the location of pheochromocytoma. However, its effectiveness largely depends on the experience of the specialist; Moreover, for tumors of extra-adrenal localization, the method is not very informative. Treatment of tumors that produce catecholamines is only surgical. However, surgical interventions for pheochromocytoma are classified as very complex, primarily due to the high degree of surgical risk associated with the likelihood of severe hemodynamic disturbances. In this regard, the cooperation of the surgeon and anesthesiologist and the choice of the most rational method of preoperative preparation and anesthesiological care are of particular importance. During preoperative preparation, the main attention should be paid to the prevention and relief of hypertensive crises. After surgery, hormone replacement therapy is often prescribed - a constant intake of adrenal hormones.
Survival prognosis
The level of postoperative survival directly depends on the degree of spread of the oncological process.
When treating stage 1-2 adrenal cancer, positive treatment results are achieved in approximately 80% of cases. But at stage 4 cancer, the prognosis is negative, because extensive metastasis occurs.
In general, the 5-year survival rate of cancer patients with stage 1 of this type of cancer is about 80%, with stage 2 – 50%, with stage 3 – 20%, and with stage 4 – 10%.
Adrenal carcinoma has a very unfavorable survival prognosis; such cancer patients live less than one and a half years. Even with early detection and treatment of the tumor, the life expectancy of such patients is very low.
Doctors at the Yusupov Hospital claim that adrenal cancer can be cured forever if you start treatment at an early stage of the disease, and for this you need to undergo a thorough diagnosis.
Extra pounds, hump and stretch marks...
The main and only treatment method for hypercortisolism caused by a tumor of the adrenal cortex or nodular hyperplasia of the adrenal cortex (Cushing syndrome) remains removal of the affected adrenal gland with the tumor. The clinical picture of hypercortisolism is very specific, therefore, in a significant proportion of patients, nosological diagnosis does not present any great difficulties. obesity, a “hump” on the back of the neck, wide purple “striae”, arterial hypertension, impaired carbohydrate metabolism and sexual function, osteoporosis and hypokalemia allow us to suspect overproduction of cortisol by the adrenal glands. At the next stage of diagnosis, especially in the absence of clear external clinical signs, the most important, and sometimes decisive, importance is the assessment of laboratory hormonal parameters. Ultrasound examination of the adrenal glands has relatively high sensitivity, it is non-invasive, relatively harmless, and accessible. The sensitivity of the ultrasound method in detecting adrenal tumors depends on their size and averages 50-90%. Corticosteroma is detected as a round formation of various sizes, with an indistinct capsule. Acoustic density appears to be slightly reduced compared to normal adrenal gland. CT is highly effective in diagnosing diseases of the adrenal glands. For adrenal adenomas, the sensitivity of the method reaches 98%. With benign corticosteromas, the prognosis is favorable. Already in the first 1.5-2 months after tumor removal, a gradual regression of clinical symptoms is noted: the patient’s appearance changes, metabolic processes are normalized, blood pressure decreases to normal, stretch marks and the face turn pale, sexual function is restored; diabetes mellitus observed before surgery disappears. In the first months after surgery, patients' body weight decreases significantly (sometimes by more than 20 kg); hirsutism usually disappears after 3-8 months. X-ray signs of bone tissue restoration are recorded after 10-12 months, but bone pain disappears within 1-2 months after surgery.
Algorithm for diagnosing adrenal adenoma
- If an adrenal tumor is detected, the first question that should be answered is “is it a benign adenoma or adrenocortical cancer?”
- The second question: “is there hormonal activity or not?”
This is where a computed tomograph comes to the rescue. It is important to use a multislice tomograph that makes at least 64 slices. The examination of the adrenal glands is performed with intravenous contrast. As a result of the study, it is necessary to obtain the size of the tumor and determine its density. A non-malignant adenoma has a small density, the contours are clearly visible, the size is not large - usually about 3 cm, sometimes larger. At the second stage, after the administration of a contrast agent, the tumor is examined in the venous or arterial phase to determine the rate of accumulation and washout of the contrast, which in a benign tumor occurs quickly and completely.
- Sometimes, to clarify diagnostic issues, it can be used, but less often than CT.
- If the task is to find out whether the adrenal gland is affected by a metastasis of a tumor that developed from another organ, an adrenal biopsy is performed. However, the method is traumatic and is rarely used.
- L are of great diagnostic value for hormonally active tumors.laboratory research
. The level of cortisol, as well as adrenocorticotropic hormone (ACTH) in the blood fluctuates throughout the day; it cannot be used to clearly determine how the adrenal glands are working. But determination of cortisol in daily urine gives an idea of their basic function.
- A small
dexamethasone test
reveals even vague manifestations of hormonal disorders in Itsenko-Cushing syndrome. The test is carried out within one day. First, the level of cortisol in the patient’s blood is determined. At 24 hours on the same day, 1 mg of dexamethasone is administered. The next morning, cortisol is again detected in the blood. A normal indicator (positive test) is a decrease in cortisol by 2 or more times. If this does not happen (negative test), then the tumor produces cortisol on its own, and this process is not controlled by the body. - Of great importance in the differential diagnosis between the syndrome and Itsenko-Cushing’s disease is large dexamethasone test
. It is carried out according to the same scheme as the small one, however, the dose of dexamethasone is not 1 mg, but 8 mg. If there is a cortisol-producing adrenal tumor, the test will be negative, and if it is Cushing's disease (pituitary adenoma), the test will be positive - cortisol will decrease by 2 or more times.
- Patients with adrenal adenoma should also have their blood tested for chromogranin A, calcitonin, parathyroid hormone, blood ions, adrenocorticotropic hormone, aldosterone and renin.
When a woman turns into a man...
Androsteroma is a tumor of the adrenal cortex that produces excessive amounts of androgens. These rather rare tumors (1-3% of all adrenal tumors) are detected in all age groups, but mainly in women under the age of 40 years. The rarity of androster detection in men may be associated with less distinct signs of virilization in them; Some of these tumors imitate hormonally inactive adrenal tumors. Symptoms of androsteroma are characterized by rapid virilization. Girls experience male-pattern pubic hair growth, enlargement of the clitoris during puberty, lack of breast growth and menstruation, increased muscle development, and the appearance of a male voice. Boys show signs of premature puberty. In women, the subcutaneous fat layer decreases, the muscles become more prominent, their mass increases, the voice becomes coarser and deepens. There is hair growth on the face, body and limbs, and hair loss on the head. Menstruation soon stops. The mammary glands become smaller. The clitoris is significantly enlarged. In most cases, there is increased libido. CT and MRI data are of decisive importance in making the diagnosis of androsteroma. Ultrasound helps to clarify the topographic relationship of the tumor with the kidney, aorta, inferior vena cava, spleen and liver, which is necessary for choosing surgical tactics. Androster treatment is only surgical - removal of the adrenal gland affected by the tumor. If the tumor is successfully removed, the symptoms of the disease quickly reverse. In advanced cases and in patients with inoperable tumors or distant metastases, treatment is symptomatic. The prognosis for early diagnosis and timely surgical treatment of benign androsterae is favorable. However, quite often children remain short in stature due to early closure of growth plates. In case of malignant androsteromas and the presence of distant metastases, the prognosis is unfavorable.
Causes
In general, malignant adrenal tumors can have a hereditary or sporadic etiology.
The following factors can trigger the oncological process:
- Consumption of carcinogenic substances, which are found in large quantities in some drinks and foods;
- Unhealthy habits such as using tobacco or alcohol;
- Age characteristics. Cancers of this nature primarily affect young children and older patients;
- Family predisposition, the presence of a genetic predisposition to adrenal cancer processes;
- Multiple endocrine tumors;
- The presence of hereditary pathologies such as Li-Fraumeni syndrome, hyperplastic polyposis, Beckwith-Wiedemann, etc.
It is quite difficult to definitively determine the causes of adrenal cancer, so the etiology of the disease often remains unknown.
... and a man into a woman
Corticoestroma is a hormonally active tumor of the adrenal cortex, emanating from the zona reticularis and zona fasciculata, excessively producing estrogens, and in some cases, glucocorticoids. Corticoestromas are most often malignant with pronounced expansive growth. Clinically, corticoestroma is characterized in males by the appearance of bilateral gynecomastia, redistribution of fatty tissue and female-type hair growth, testicular hypotrophy, increased timbre of voice, decreased potency up to its loss. Oligospermia is often observed. Some patients experience pigmentation of the areolas of the mammary glands and even discharge from the nipples when pressing on them. In boys, signs of the disease include gynecomastia and premature bone maturation. A feminizing tumor of the adrenal cortex in girls is accompanied by a clinical picture of premature puberty: enlargement of the mammary glands and external genitalia, pubic hair growth, accelerated body growth, premature skeletal maturation, vaginal bleeding. In women, this tumor does not manifest itself in any way and can only be accompanied by an increase in the level of estrogen in the blood. Adrenal tumors that manifest only pure feminization are extremely rare. Treatment is only surgical (removal of the tumor along with the affected adrenal gland). To prevent possible adrenal insufficiency in the postoperative period, glucocorticoid replacement therapy is prescribed.
Types and stages of adrenal tumors
There are benign and malignant tumors of the adrenal glands; in addition, they are hormonally active and hormonally inactive.
Neoplasms are distinguished by location:
- cortical layer - corticosteromes, corticoestromes, aldosteromes, androsteromes and others.
- medulla - pheochromocytomas and ganglioneuromas.
We treat all types of adrenal tumors, using innovative surgical techniques to reduce the risk of recurrence.
Incidentally discovered tumors
With the introduction of ultrasound examination and high-resolution radiological methods of topical diagnostics, such as computed tomography and magnetic resonance imaging, into medical practice, formations in the adrenal glands began to be detected in patients examined for various reasons, which had not previously manifested themselves clinically. In most cases, we are talking about relatively small neoplasms ranging in size from 0.5 to 6 cm in diameter. These tumors became known as incidentalomas. The incidental discovery of an adrenal tumor should prompt the physician to more carefully examine the patient for symptoms of adrenocortical, adrenomedullary disease, or malignancy. Tactics regarding adrenal incidentaloma depend, firstly, on whether it is a source of excess production of any hormone, and, secondly, whether it is a malignant tumor. Hypersecretory formations of the adrenal glands require specific therapy and, most often, surgical intervention. In general, the approach to adrenal incidentalomas is such that hypersecretory and malignant formations require removal, as well as tumors of large sizes (more than 5 cm) and suspicious for malignancy, while formations that have been proven to be benign, such as a simple adrenal cyst, myelolipoma and Adrenal hematoma requires only regular (every six months) CT monitoring.
What questions should you ask your doctor?
Which doctor should I see after discovering an adrenal mass?
After the first detection of any formation, the first step is to consult an endocrinologist. If after the examination it turns out that the formation is malignant, he will redirect you to an oncologist.
What should I do after I have been diagnosed with adrenal cancer?
After the malignancy of the formation is confirmed, it is necessary to assess the consequences of its presence in the body - to search for metastases. The range of studies when searching for metastases includes CT of the lungs, CT or MRI of the brain and abdominal cavity, scintigraphy and MRI of bones. To identify tumor thrombi, phlebography of the retroperitoneal vessels is performed.
When should I have surgery?
As soon as possible after confirming the diagnosis of cancer. The emphasis on the urgency of surgical intervention is associated with rapid progression of tumor size and a high probability of metastasis.
Is surgery to remove the adrenal glands dangerous?
Surgery to remove the adrenal glands is an absolute necessity when diagnosing adrenocortical cancer. Since the adrenal glands are glands that produce important hormones, an important task of the doctor is to correct hormonal imbalances that may have arisen before surgery due to the disease. As for the hormonal therapy itself, which is prescribed after removal surgery, it is mainly additional. So-called “replacement” therapy is prescribed in the case of bilateral removal of the adrenal glands - when bilateral damage occurs.
How often should I be tested after adrenal cancer removal?
Every 3 months it is necessary to undergo examinations to monitor the process.
Salvage adrenalectomy
In 2002, it was 10 years since Michel Gagner first described the experience of successful laparoscopic adrenalectomies in periodicals. In one decade, this minimally invasive surgical technique has rapidly spread throughout the world, developing and improving. Currently, due to its safety and practicality, endoscopic adrenalectomy has become firmly established in the arsenal of adrenal surgery. During the period from November 1996 to May 2004, we performed 152 endoscopic operations in patients with adrenal pathology. Over the past few years, we have preferred extraperitoneal (“posterior”) adrenalectomies, which are more difficult to perform for the surgeon, but much easier to tolerate by the patient. We have extensive experience in these operations. Most of our patients are discharged from the clinic 3-4 days after surgery, and after 2-3 weeks they are allowed full physical activity, which is impossible with “open” operations. Add to this the absence of a large scar, possible weakening of the muscles of the lumbar region in the postoperative period, and the advantages of endoscopic adrenalectomy will become undeniable. After one of the adrenal glands is removed, the second one takes on the entire load. In this case, the patient usually requires lifelong hormone replacement therapy, which should be prescribed by an endocrinologist. In the future, it is necessary to undergo a follow-up examination every six months and consult with a doctor, who will adjust the therapy depending on the test results and the patient’s health condition. Patients who have undergone adrenalectomy also need to avoid physical and mental stress, and not drink alcohol or sleeping pills.
Treatment of adrenal cancer in Moscow
Yusupov Hospital is a specialized center for the treatment of adrenal cancer in Moscow and the Moscow region. It employs leading oncologists and endocrinologists. Many doctors have scientific titles and the highest medical category. The cost of operations at the Yusupov Hospital is lower than in other clinics in Moscow. The price of examination and treatment corresponds to the quality of the services provided.
If you have signs that resemble those of adrenal cancer, call the Yusupov Hospital. You will be scheduled for an appointment with an endocrinologist-oncologist at a time convenient for you. After the examination, professors and doctors of the highest category will make a collegial decision on treatment tactics.
Make an appointment