Classifications of precocious puberty
An attempt to systematize individual varieties of this pathological condition made it possible to identify two main forms of premature puberty
:
1. True,
or
premature puberty of central origin
, the development of which is associated with premature activity of the pituitary gland and hypothalamus. In this case, an increase in the production of sex hormones by the gonads occurs due to the stimulation of the internal sex glands by gonadotropic hormones produced by the pituitary gland and hypothalamus.
2. False,
or
peripheral precocious puberty
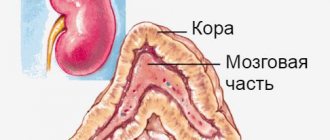
, which is caused by enzymatic defects in the synthesis of steroid hormones by the adrenal cortex or tumors of the gonads, which leads to an increase in the production of sex hormones, and is not associated with the level of gonadotropins.
3. Precocious puberty associated with gene code disorders
, leading to autonomous activation of the activity of the gonads, independent of the level of gonadotropins.
There is no clear boundary between true and false forms of precocious puberty; they can transform into one another or occur in combination, however, for the convenience of diagnosis and choice of treatment tactics, a working version of the classification of precocious puberty has been developed, according to which the following forms are distinguished:
1. True precocious puberty
, which includes:
- idiopathic premature puberty;
- cerebral precocious puberty, which developed due to tumors, as well as non-tumor lesions of the central nervous system (hamartomas, gliomas, encephalitis, hydrocephalus, meningitis, toxoplasmosis, radiation, surgery, arachnoiditis). Cerebral precocious puberty can also be caused by congenital syndromes such as neurofibromatosis, tuberous sclerosis and a number of others;
- true premature puberty, developing as a result of prolonged exposure to sex hormones due to untimely correction of congenital dysfunction of the adrenal cortex, or late removal of tumors that produce hormones.
2. False precocious puberty
which occurs:
- in male patients due to testicular tumors, neoplasms located in and outside the skull that produce chorionic gonadotropic hormone, adrenal tumors and congenital dysfunction of the adrenal cortex;
- in female patients - as a result of malignant neoplasms of the ovaries, adrenal tumors, or the presence of ovarian follicular cysts.
3. Gonadotropin-independent forms of precocious puberty
:
- McCune-Albright syndrome;
- testotoxicosis.
4. Incomplete forms of premature puberty
:
— accelerated pubarche (hair growth);
- early thelarche (enlargement of the mammary glands).
All of the listed forms of premature puberty are characterized by the main signs of progression of puberty, namely, the appearance of secondary sexual characteristics, an increase in the volume of the external genitalia, accelerated growth and maturation of bone tissue.
Depending on the completeness of clinical manifestations, the full form of precocious puberty
, in which all of the above clinical signs can be identified, and
an incomplete form of precocious puberty
, which is characterized by the development of only premature pubarche (secondary hair growth) or thelarche (increase in the size of the mammary glands).
In addition, there are forms of precocious puberty that do not fit into any of the above, for example, precocious puberty that developed against the background of uncompensated primary hypothyroidism.
When your stomach hurts
In healthy girls, menstruation is usually regular; for them, menstrual irregularities are quite rare. Such disorders are manifested by a reduction or lengthening of the time interval between menstruation, an increase in the duration of menstruation itself, the amount of blood lost and pain.
Dysmenorrhea is pain before and during menstruation that occurs due to uterine contractions under the influence of prostaglandins. A high level of prostaglandins leads to increased contractile activity of the uterus, vasospasm, and ischemia, which causes pain. A similar mechanism of action of prostaglandins is also triggered during childbirth. Therefore, girls suffering from severe dysmenorrhea need serious attention, since they go through a mini-birth during menstruation.
In some cases, dysmenorrhea occurs when the uterus is in an incorrect position, when a bend in the cervical canal is formed. In this case, the uterine muscle has to make strong contractions to expel the contents from the cavity in order to push the blood through. Other causes of dysmenorrhea may be pelvic inflammatory disease, endometriosis, and uterine fibroids. Therefore, if you have dysmenorrhea, you should consult a doctor, which will allow you to establish the true cause of this suffering and eliminate it.
By the way, there is an opinion that several decades ago women saved themselves from pain in the lower abdomen... by washing the floor with a rag in their hands, without a mop...
Causes of premature puberty
True, or gonadotropin-dependent precocious puberty is due to the fact that the activation of the pulsed secretion of gonadotropin-releasing hormone produced by the hypothalamus occurs earlier than expected. An increase in the secretion of this GnRH leads to an increase in the production of luteinizing and follicle-stimulating hormones of the pituitary gland, which are gonadotropic. These, in turn, activate the production of sex hormones in the gonads, thereby leading to the development of secondary sexual characteristics that change the appearance of the child. The most common cause of true precocious puberty is hypothalamic hamartoma.
The cause of false precocious puberty is most often a disruption in the enzymatic processes of production of steroid hormones in the adrenal cortex, less often - tumors of the gonads and adrenal glands that produce sex hormones.
The cause of the development of forms of precocious puberty, independent of the level of gonadotropin, is considered to be genetic mutations that lead to the constant activation of the production of sex hormones by the cells of the male and female gonads without the participation of gonadotropic hormones.
Sources
- Ge W., Wang H.L., Shao H.J., Liu H.W., Xu R.Y. Evaluation of serum makorin ring finger protein 3 (MKRN3) levels in girls with idiopathic central precocious puberty and premature thelarche. // Physiol Res - 2021 - Vol69 - N1 - p.127-133; PMID:31852205
- Varimo T., Huttunen H., Miettinen PJ., Kariola L., Hietamäki J., Tarkkanen A., Hero M., Raivio T. Precocious Puberty or Premature Thelarche: Analysis of a Large Patient Series in a Single Tertiary Center with Special Emphasis on 6- to 8-Year-Old Girls. // Front Endocrinol (Lausanne) - 2021 - Vol8 - NNULL - p.213; PMID:28878739
- Sømod ME., Vestergaard ET., Kristensen K., Birkebæk NH. Increasing incidence of premature pregnancy in the Central Region of Denmark - Challenges in differentiating girls less than 7 years of age with premature pregnancy from girls with precocious puberty in real-life practice. // Int J Pediatr Endocrinol - 2021 - Vol2016 - NNULL - p.4; PMID:26909102
- Özgen İT., Torun E., Bayraktar-Tanyeri B., Durmaz E., Kılıç E., Cesur Y. The relation of urinary bisphenol A with kisspeptin in girls diagnosed with central precocious puberty and premature thelarche. // J Pediatr Endocrinol Metab - 2021 - Vol29 - N3 - p.337-41; PMID:26565542
- Asci A., Durmaz E., Erkekoglu P., Pasli D., Bircan I., Kocer-Gumusel B. Urinary zearalenone levels in girls with premature thelarche and idiopathic central precocious puberty. // Minerva Pediatr - 2014 - Vol66 - N6 - p.571-8; PMID:25336100
- Bizzarri C., Spadoni GL., Bottaro G., Montanari G., Giannone G., Cappa M., Cianfarani S. The response to gonadotropin releasing hormone (GnRH) stimulation test does not predict the progression to true precocious puberty in girls with onset of premature death in the first three years of life. // J Clin Endocrinol Metab - 2014 - Vol99 - N2 - p.433-9; PMID:24297793
Clinical signs of precocious puberty
In true forms of precocious puberty, girls experience enlargement of the mammary glands and external genitalia. In most cases, pubertal hair develops, but its intensity is significantly less than in girls during normal puberty. Other androgen-dependent symptoms of puberty, such as acne, oily seborrhea, and increased functioning of the sweat glands, are also uncharacteristic. These symptoms in girls with early puberty develop after 6–7 years of age because physiological activation of androgen function of the adrenal glands occurs during this period.
With high activity of the pathological process, menstruation begins, which is regular. For example, in girls with hypothalamic hamartoma, menstruation begins extremely early - several months after the noticeable enlargement of the mammary glands. However, half of girls with true precocious puberty may not menstruate for several years after the appearance of secondary sexual characteristics.
In patients with false forms of premature puberty, menstruation can be observed along with breast enlargement. In this case, the discharge is erratic, there is no cyclicity, it can be copious or spotting.
With isolated thelarch in children under two years of age, the only secondary sexual characteristic is enlargement of the mammary glands; after three years, a milder version of true early puberty is observed.
With isolated adrenarche, girls develop hair growth in the pubic and sometimes axillary areas. In boys, there is an increase in the size of the testicles and penis, secondary sexual characteristics quickly develop, such as sexual hair growth, acne, deepening of the voice, increased muscle mass, increased sweating with a specific odor.
False forms of precocious puberty in boys are characterized by unchanged testicular volume against the background of rapidly developing secondary sexual characteristics. With testotoxicosis, the gonads can significantly increase in volume, but there are options for the course of the pathological process in which the enlargement of the testicles is insignificant compared to the development of secondary sexual characteristics.
In girls and boys with all forms of early puberty, growth acceleration of up to 10-15 cm per year is observed, which is characteristic of a growth spurt during physiological puberty, and it may precede the development of secondary sexual characteristics. Skeletal bones also undergo early differentiation, leading to premature closure of growth plates, which can lead to a significant reduction in final height.
Menstruation
According to the encyclopedic definition, menstruation is the cyclic shedding of the thickened layer of the endometrium (the lining of the uterus) and the release of blood from the uterus, which occurs monthly in women of reproductive age.
Menstruation comes monthly - a very conventional concept. The normal length of the menstrual cycle (the period from the first day of one menstruation to the first day of the next) ranges from 21 to 35 days. In healthy women and girls with an established menstrual cycle, there are almost no deviations in its duration or they do not exceed 3-4 days. If the duration of the cycle is more than 35 days or less than 21, this is a reason to contact a gynecologist to find out the reasons and prescribe treatment. However, often with climate change, in the spring months, and stress (for example, passing exams, especially graduation and entrance exams), the duration of the menstrual cycle can change significantly. You should definitely consult a doctor if your menstruation is delayed by three months or more.
All processes in a woman’s life occur cyclically, that is, with a certain periodicity, and menstruation is the most striking manifestation of the end of one cycle and the beginning of another. And it indicates that fertilization of the egg has not occurred and the reproductive system begins a new cycle of preparing the woman’s body for pregnancy.
Methods for diagnosing premature puberty
At the first stage of treatment of patients with precocious puberty, the form of the disease should be determined and the nature of activation of gonadotropic function should be identified. The next step is to determine the source of the increased production of gonadotropic and sex hormones. To go through all these stages, a series of diagnostic studies should be carried out.
When collecting anamnesis, attention should be paid to the nature of sexual development in relatives. Early puberty among males on the paternal or maternal side often becomes evidence of testotoxicosis. If, when collecting anamnesis, a specialist receives information about the presence of brothers and sisters in the family with signs of premature puberty, this suggests that the patient has congenital dysfunction of the adrenal cortex. Hypothalamic hamartoma usually manifests itself with an early onset of the disease and the rapid development of secondary sexual characteristics.
The physical examination involves a clinical assessment of sexual development based on the Tanner-Marshall classification, which assesses the degree of development of the mammary glands, external genitalia, menstruation, and body type in girls. In boys, attention is paid to the volume and consistency of the testicles, the size of the penis, the presence and frequency of erections, the degree of development of the muscular system, changes in voice, the presence of acne on the skin, as well as the degree of pubic and axillary hair. In addition, growth dynamics are determined in patients of both sexes.
During an external examination, you should also pay attention to the presence of symptoms of diseases accompanied by clinical signs of premature puberty. For example, the presence of large spots with uneven borders on the skin may indicate the presence of McCune-Albright-Braitsev syndrome, and a large number of small pigment spots and subcutaneous nodules are characteristic of neurofibromatosis.
Laboratory diagnosis of precocious puberty consists primarily of determining the level of sex hormones, although this type of study does not reveal the form of early puberty. Another laboratory method for diagnosing the disease is to determine the content of dehydroepiandrosterone sulfate, an increased level of which is observed in androgen-producing adrenal tumors. Measurement of 17-hydroxyprogesterone concentration provides evidence of the presence of congenital adrenal dysfunction in patients. If patients are suspected of having tumors that produce chorionic gonadotropic hormone, it is recommended to determine its content in the blood, which, in the presence of a tumor, exceeds normal levels tens of times.
Experts consider the test with luliberin to be an informative method for laboratory diagnosis of premature puberty, which allows one to obtain objective information about the state of gonadotropins. To carry it out, a natural luliberin preparation can be used, which is administered intravenously at a dose of 50-100 mcg or its artificial analogues of daily action - diferelin or buserelin. When administering luliberin intravenously, before its administration, as well as half an hour, an hour, one and a half and two hours after, blood samples are taken, in which the maximum rise of luteinizing hormone is recorded at 30 minutes, and follicle-stimulating hormone - an hour and a half after administration of the drug.
Since buserelin is administered through the nose, test results may be falsely negative if the patient has swelling or atrophy of the nasal mucosa, so its use is limited. More reliable results can be obtained with subcutaneous administration of daily action of diferelin, while measurements of the level of luteinizing and follicle-stimulating hormones are carried out in blood samples taken one hour and four hours after administration of the drug.
In the case of a true form of precocious puberty, the level of maximum concentration of luteotropic hormone is characteristic. In false gonadotropin-independent forms of early puberty, the level of luteotropic hormone is reduced to minimally detectable values. Incomplete forms of precocious puberty syndrome are characterized by levels of the above hormone that correspond to the norm. In the case of isolated thelarche, an increase in the level of follicle-stimulating hormone is observed against the background of a slight increase in the level of luteinizing hormone.
Instrumental methods for studying patients with precocious puberty include radiographic examination of the bones of the hands to determine bone age. In patients with incomplete forms of precocious puberty, bone age coincides with chronological age. Tumors of the hypothalamus, testotoxicosis, congenital dysfunction of the adrenal cortex due to high concentrations of sex hormones lead to a sharp increase in bone age, which is clearly observed on x-rays.
To exclude neoplasms of the central nervous system, computer and magnetic resonance imaging methods are used. Ultrasound examination in girls makes it possible to assess the degree of enlargement of the ovaries and uterus, to identify the presence of follicular cysts and space-occupying formations of the ovaries. In boys, ultrasound can be used to diagnose testicular tumors and adenomas characteristic of testotoxicosis, as well as to identify tumors in the adrenal glands.