Acute leukemia is a cancer of the blood and hematopoietic organ - the red bone marrow, in which normal leukocytes are gradually replaced by immature (blast) cells that are unable to perform their function. As a result, the patient develops inflammation and bleeding of internal organs, which significantly worsens his condition, immunity sharply decreases, and the nervous system is affected. In the absence of qualified medical care, an unfavorable outcome inevitably occurs. The disease is characterized by high aggressiveness: mutated cells quickly spread throughout the body, and their number grows at high speed.
Types of disease
Oncohematologists, depending on the nature of the cell pathology, distinguish two main types of acute blood leukemia.
- Lymphoblastic. Accounts for approximately 15-20% of cases. First, malignant cells affect the bone marrow, then spread to the lymph nodes, thymus gland and spleen, and then throughout the body. A characteristic feature is that mutated cells lack lipids, esterase, and peroxidase. It most often develops in children aged from one to six years and in adults after forty years. In turn, it is divided into two types: B-form with a favorable prognosis for a third of adults and two-thirds of sick children, and T-form with an extremely severe course and a sad outcome.
- Myeloblastic. The disease usually develops in adulthood and affects men and women equally. The treatment prospects are quite optimistic: partial remission can be achieved for 80% of patients, complete recovery occurs in at least 20%.
The full classification of acute leukemia includes many subtypes that differ in morphological, genetic and other characteristics that require specific treatment.
Hematology. ACUTE LEUKEMIA: CLASSIFICATION, DIAGNOSIS AND TREATMENT
Acute leukemia is divided into lymphoblastic (ALL) and myeloblastic (AML). It is believed that the occurrence of acute leukemia can be caused by the following factors:
- unidentified (most often);
- hereditary:
- Down syndrome
- Bloom's syndrome
- Fanconi anemia
- ataxia-telangiectasia
- Klinefelter's syndrome
- osteogenesis imperfecta
- Wiskott-Aldrich syndrome
- leukemia in twins
- chemical:
- benzene
- alkylating agents (chlorambucil, melphalan)
- radiation exposure
- predisposing hematological disorders (myelodysplasia, aplastic anemia)
- HTLV-I viruses, which cause T-cell leukemia and lymphoma in adults.
In recent decades, significant advances have been made in the treatment of acute leukemia. Five-year survival depends on the type of leukemia and the age of the patients:
- ALL in children - 65 - 75%;
- ALL in adults - 20 - 35%;
- AML in patients under 55 years of age - 40 - 60%;
- AML in patients over 55 years of age - 20%.
Classification
The differences between ALL and AML are based on the morphological, cytochemical and immunological features of these types of leukemia. Accurate determination of the type of leukemia is of paramount importance for therapy and prognosis. Both ALL and AML, in turn, are divided into several variants according to the FAB classification (French-American-British). Thus, there are three variants of ALL - L1, L2, L3 and seven variants of AML:
- M0 - undifferentiated AML;
- M1 - myeloblastic leukemia without cell maturation;
- M2 - myeloblastic leukemia with incomplete cell maturation;
- M3 - promyelocytic leukemia;
- M4 - myelomonocytic leukemia;
- M5 - monoblastic leukemia;
- M6 - erythroleukemia;
- M7 - megakaryoblastic leukemia.
In accordance with the expressed antigens, ALL is divided into T-cell and B-cell types, which, depending on the degree of maturity, include several subtypes (pre-T-cell, T-cell, early pre-B-cell, pre-B-cell , B-cell). There is no clear correlation between morphological and immunophenotypic variants, except that L3 morphology is characteristic of B-cell leukemia. With regard to AML, immunophenotyping (i.e., determination of expressed antigens) does not always help distinguish between M0 and M5 variants. For this purpose, special cytochemical staining is additionally used. To make a diagnosis of erythroleukemia (M6) and megakaryoblastic leukemia (M7), immunophenotyping is sufficient.
Prevalence
ALL most often occurs at the age of 2-10 years (peak at 3-4 years), then the prevalence of the disease decreases, but after 40 years there is a repeated rise. ALL accounts for about 85% of leukemias occurring in children. AML, in contrast, is most common in adults, and its incidence increases with age.
Clinical manifestations
Clinical manifestations of leukemia are caused by blast infiltration of the bone marrow and internal organs. Anemia is manifested by pallor, lethargy, and shortness of breath. Neutropenia leads to various infectious complications. The main manifestations of thrombocytopenia are spontaneous formation of hematomas, bleeding from the nose, uterus, injection sites, and gums. Bone pain, lymphadenopathy, and hepatosplenomegaly are also characteristic. Possible difficulty breathing due to the presence of mediastinal masses, enlarged testicles, and meningeal symptoms. Gingival hypertrophy occurs in AML.
Patient examination
Complete blood count: possible decrease in hemoglobin level and platelet count; leukocyte content - from less than 1.0 • 109/l to 200 • 109/l, their differentiation is impaired, blasts are present. The coagulogram can be changed, especially in promyelocytic leukemia, when blast cells contain granules containing procoagulants. A biochemical blood test with high leukocytosis may indicate renal failure. A chest x-ray reveals mediastinal masses, which occur in 70% of patients with T-cell leukemia. Bone marrow puncture: hypercellularity with a predominance of blasts. Immunophenotyping is a defining method in distinguishing between ALL and AML. Cytogenetic and molecular studies can detect chromosomal abnormalities, for example the Philadelphia chromosome (a translocation product of part of chromosome 9 to 22; determines a poor prognosis in ALL). Lumbar puncture is used to detect damage to the central nervous system (neuroleukemia).
Treatment
All patients with suspected or established leukemia should be sent for examination and treatment to specialized hospitals as quickly as possible. Maintenance therapy includes transfusions of platelets, red blood cells, fresh frozen plasma, and antibiotic therapy for infectious complications.
| Factors | ALL | AML |
| Age | Less than 1 year or more than 10 years | Over 60 years |
| Floor | Male | Male or female |
| Leukocytosis | More than 50 • 109/l | More than 50 • 109/l |
| CNS damage | Blasts in the cerebrospinal fluid | Blasts in the cerebrospinal fluid |
| Remission | Not achieved after induction therapy | More than 20% of blasts in the bone marrow after the 1st course of treatment |
| Cytogenetics | Philadelphia chromosome | Deletions or monosomy of chromosomes 5 or 7; multiple chromosomal abnormalities |
The goal of chemotherapy is to induce remission (less than 5% of blasts in the bone marrow) and subsequent elimination of residual blast cells through consolidation therapy. Chemotherapy drugs disrupt the ability of malignant cells to divide, and combining two or three drugs increases the effectiveness of therapy and reduces the risk of blasts developing resistance to therapy. For the prevention and treatment of neuroleukemia, endolumbar injections of methotrexate and cranial irradiation are used. Bone marrow transplantation (BMT). Allogeneic BMT can be used in case of poor prognosis in ALL, in AML in first remission, and in relapsed leukemia. However, due to the shortage of compatible donors, this option is not available to all patients. Factors that determine a poor prognosis for acute leukemia are presented in the table.
Toxicity of therapy
Early toxicity includes nausea, vomiting, mucositis, hair loss, neuropathies, liver and kidney failure, and severe inhibition of hematopoiesis. Late toxicity can manifest itself as damage to various organs:
- heart - arrhythmias, cardiomyopathy;
- lungs - fibrosis;
- endocrine system - growth retardation, hypothyroidism, infertility;
- kidneys - decreased glomerular filtration;
- psyche - emotional and intellectual disorders;
- secondary tumors;
- cataract.
All patients with acute leukemia should be followed up for at least 10 years after completion of treatment. Problems such as growth retardation and endocrine dysfunction in children require special attention.
Literature:
Liesner RJ, Goldstone AH. The acute leukaemias. BMJ 1997;314:733-6.
Symptoms
The first signs by which one can suspect the onset of the disease are the same for all its forms.
- Noticeable weight loss not associated with food restriction or exercise.
- Fatigue, deterioration in general health.
- Constant weakness, apathy, drowsiness.
- A feeling of heaviness after eating, often concentrated in the left hypochondrium and independent of the amount and calorie content of what was eaten.
- Frequent infectious diseases.
- Increased sweating, especially at night.
- Increased body temperature.
As malignant cells grow in the blood, the symptoms of acute leukemia become more pronounced.
- Pale skin, shortness of breath due to lack of oxygen carried by the blood, anemia.
- Frequent bleeding from the nose and gums, bruising on the skin and mucous membranes, in women - heavy periods.
- Dysfunction of the affected internal organs with its own specific manifestations.
- Severe pain in bones and joints.
- Increased size of the spleen and liver.
- Constant swelling of the hands and face.
Clinical signs are not differentiated in accordance with the classification of acute leukemia, so the form of the disease can only be determined using laboratory tests.
What is the cause of cancer?
Unfortunately, there is no answer to this question yet. Although the mechanism of tumor formation has been sufficiently studied, scientists have not yet been able to accurately determine the cause that starts the oncological process. However, some factors that can trigger the disease are known, while others are “under suspicion.”
Help Malignant tumors arise as a result of the transformation of normal cells, which begin to multiply uncontrollably. If the body's immune system does not recognize such a transformation in time, the tumor begins to grow and metastasize (spread) over time. Metastases can form in all organs and tissues without exception. Metastases most often occur in the bones, liver, brain and lungs.
Heredity
Certain genetic mutations can significantly increase the risk of developing malignant tumors. A classic example is some forms of breast cancer, which are hereditary.
Fact
Article on the topic
Corporate conspiracy or personal decision?
Expert on mastectomy, Jolie and cancer American actress Angelina Jolie had both mammary glands and ovaries removed due to the high risk of cancer. Since several of Jolie's close relatives died from breast cancer, the actress decided to undergo genetic testing. It turned out that due to mutations of certain genes, Jolie's risk of breast and/or ovarian cancer was more than 80%.
Bad habits
For example, the connection between cancer and smoking has been well studied, and we are talking not only about lung cancer, but also about some other tumors. Of course, this does not mean that all smokers will certainly get cancer, but in general, the risk for owners of this bad habit is significantly higher.
Fact
One of the famous cigarette brands chose a brave cowboy as the image for its advertising campaign. Four actors who starred in commercials over the years died of lung cancer.
Excess weight
There is no exact explanation for the connection between obesity and cancer, there are only theories.
According to one of them, the reason lies in hormonal imbalance, which can be caused by excess weight.
In addition, type 2 diabetes is more common in obese people, which is also one of the increased risk factors for cancer.
Fact
It has been proven that people with increased body weight are at risk for 13 types of cancer.
Age
As you age, your risk of getting cancer increases. Over the years, various “breakdowns” accumulate in the body, which can lead to the formation of a tumor; it is no coincidence that many experts consider cancer to be a faithful companion of aging. But, alas, youth is not a 100% guarantee of protection against cancer, because malignant tumors also occur in children.
Fact
It happens that unborn children get cancer - a malignant tumor can form already at the stage of embryonic development. Now such babies have a chance to survive - doctors already know how to perform intrauterine operations to remove the tumor.
Stress
There are theories that link stress to cancer. However, none of them have received rigorous evidence.
Fact
It is impossible to find a person who has never experienced stress. In addition, it is quite difficult to select universal criteria for assessing the amount of stress. After all, we all react to difficult situations differently. Some people remain relatively calm in truly critical circumstances, while others become acutely aware of the slightest trouble.
Sitting in cages. The Nobel laureate named the cause of cancer Read more
Causes and risk factors
The etiological factors that inevitably become the “trigger” for malignant cell mutation have not yet been precisely established. However, the risks of developing acute leukemia increase significantly if:
- radiation exposure to which a person is exposed;
- infection with certain viruses that suppress the immune system (Epstein-Barr disease, T-lymphotropic virus, etc.);
- unfavorable heredity;
- smoking tobacco;
- prolonged exposure to certain chemical compounds, including medications;
- stress, depression;
- environmental pollution.
Is it true?
There are many misconceptions associated with cancer. Let's look at the most common of them.
Myth . Young people develop cancer faster than older people.
The rate of cancer development in most cases depends on the type of tumor, and not on the age of the patient or the characteristics of his body. Moreover, some types of tumors behave differently in people of different ages. For example, low-grade glioma in children often resolves without any treatment or with minimal intervention, but in adults it can be fatal.
Myth . If a person has one cancer, he is insured against other types of cancer.
Alas, this is not true . It happens that one patient is diagnosed with several cancer diseases at once. Conversely, it is impossible to say that if a person has a certain type of cancer, he has a higher risk of developing other tumors.
Myth . Cancer is contagious.
No . You cannot become infected with cancer. It is true that some viruses increase the risk of cancer. For example, the human papillomavirus can lead to cervical cancer, and the hepatitis virus can lead to liver cancer. But this is a complex relationship; a minority of HPV carriers will develop cervical cancer.
Myth . Mobile phones and microwave ovens increase the risk of developing tumors.
The connection between radiation from cell phones and microwaves and the appearance of malignant tumors has not been proven.
Myth . Cancer can be cured through fasting.
This statement is based on the fact that cancer cells require a lot of nutrients to divide. But the cancer cell will receive its “portion” of nutrition in any case, even if the person completely refuses food. But dietary restrictions can negatively affect the general condition of the body, so doctors advise cancer patients to eat well.
How to reduce the risk of cancer? 9 anti-cancer principles Read more
Stages
Oncohematologists distinguish the following stages of acute leukemia.
- Initial. It proceeds secretly and lasts from several months to several years. Diagnosed only by bone marrow examination, as blood tests show only minor abnormalities in the white blood cell count and there are no symptoms.
- Expanded. The number of immature cells in the blood increases sharply, which leads to a deterioration in health and the appearance of initial symptoms of the disease.
- Remission. Manifestations of oncopathology decrease, however, a certain number of blast cells remain in the bone marrow (with complete remission - no more than 5%).
- Relapse. The number of immature cells in the patient's bone marrow and blood increases, and his condition worsens.
- Terminal. The most severe stage of the disease, which is characterized by numerous complications of acute leukemia: vital internal organs are affected, extensive bleeding, ulceration and tissue necrosis occur.
Symptoms of leukemia in the second stage of the disease
A condition such as sweating will surprise few people, especially in the hot season. However, if a person sweats constantly, although this has not been observed before, then this is a reason to think about his condition. In case of a malignant blood anomaly, it is sweating that is that alarming “bell” that cannot be ignored. This problem is especially relevant at night. The reason is damage to the central nervous system.
If you start cancer treatment abroad at this stage, you can count on good results.
In addition to sweating, enlarged lymph nodes should also alert you.
The first to suffer are:
- inguinal;
- axillary;
- clavicular
With leukemia, leukocytes are affected, therefore, their immature forms will accumulate in large quantities in the nodes, which will begin to actively increase.
If you notice a lymph node that is more than 2 cm in diameter, you should immediately consult a doctor.
As a rule, no more negative manifestations of the disease can be noticed at the second stage. Sometimes bruises and bruises make themselves known, but this happens rarely. In addition, these are attributed to accidental blows and bruises.
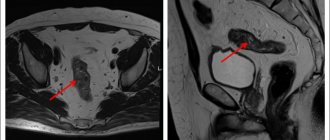
Diagnostics
A patient with symptoms resembling acute leukemia is prescribed:
- blood tests - general, biochemical, coagulogram;
- removal of bone marrow from the ilium or sternum, followed by cytochemical analysis, immunophenotyping, and morphological analysis of cells;
- puncture of bone marrow and cerebrospinal fluid for cytological and histological examination;
- instrumental studies of internal organs - ultrasound, radiography, CT, MRI to assess the extent of their damage by malignant cells;
- consultations with a neurologist, otolaryngologist, ophthalmologist and other specialists.
Treatment
Since the list of the most aggressive malignant diseases includes acute leukemia, treatment should begin immediately after diagnosis. The patient is placed in an oncohematology hospital in a ward with special ventilation to remove pathogenic microflora. The main method, as a rule, is chemotherapy, which is supported by transfusion of blood components, detoxification therapy, and prevention of infections. The treatment regimen consists of the main stages:
- induction of remission - exposure to chemotherapy that destroys blast cells in order to achieve the maximum possible remission;
- consolidation - consolidation of achieved results;
- prevention of relapse - preventing the return of the disease.
In certain forms of the disease, bone marrow stem cell transplantation, performed after destruction of blasts using chemotherapy and radiation therapy, has a good effect.
The first stage of treatment takes from 4 to 6 weeks, during which time the patient receives massive therapy. At the consolidation stage, two or three courses of treatment are carried out, after which maintenance measures continue for several years, which are necessary to prevent relapses. Complete remission is achieved when the clone of pathological cells is destroyed and the normal hematopoietic process is restored.
Diet for leukemia
There is no special diet for leukemia. Nutrition must be nutritious, since the pathological process occurring in the body leads to a weakening of the immune system. In order for the bone marrow to produce healthy blood cells, it needs large quantities of protein, carbohydrates, fats, vitamins, micro- and macroelements. Therefore, a child’s daily diet should include fruits, berries and vegetables. Freshly squeezed juices from pomegranate, carrots and beets are beneficial.
Due to anemia, you need to eat foods rich in iron. It is advisable to limit:
- fatty fish;
- fatty dairy products (can lead to metabolic disorders);
- baked goods, sweets;
- fried and smoked.
Replace pork with turkey or chicken.
Rehabilitation
The list of clinical recommendations for acute leukemia during the rehabilitation period includes:
- measures to improve immunity;
- balanced diet;
- detoxification therapy;
- restoration of intestinal microflora;
- anti-stress psychotherapy;
- improving sleep quality.
During the recovery period, it is important to follow all the orders of the attending oncologist and complete the recommended treatment courses on time and in full.
Celebrities who beat cancer
Actor Michael Douglas . Laryngeal cancer. The diagnosis was made in 2010. Two years later, the actor returned to cinema.
Singer Kylie Minogue . Breast cancer. Doctors discovered a tumor in 2005. After a course of treatment, the singer returned to the stage.
Actor Robert De Niro . Prostate cancer. The diagnosis was made in 2003. Treatment took about 2 months, then the actor returned to work.
Singer Rod Stewart . Thyroid cancer, prostate cancer. In 2000, the singer underwent surgery to remove a thyroid tumor, and three years ago he announced that he was diagnosed with prostate cancer. Meanwhile, in 2021, Rod released his new album.
Writer Daria Dontsova . Breast cancer. The tumor was discovered in 1998. Now she is actively helping women who are faced with this disease.
Singer Laima Vaikule . Breast cancer. The diagnosis was made in 1991. Now she continues to perform on stage.
Mission Possible. Russian stars who managed to defeat cancer Read more