In medicine, a dislocation of the hip joint is a displacement of the head of the femur, accompanied by damage to the joint capsule. In adults, the cause of pathology is injury, in children – hip dysplasia.
Do not confuse a dislocation with a subluxation of the hip joint. With the latter, the head of the femur is incorrectly oriented in space, but does not extend beyond the acetabulum.
Causes of hip dislocation in adults
In adults, dislocations of the hip joint are rare. This is explained by the fact that the head of the femur is firmly fixed in the acetabulum, and the joint itself is strengthened by ligaments and muscles. In order for the femur to move from its place, a high-velocity traumatic factor is needed.
Possible reasons for the displacement:
- car crashes;
- natural disasters;
- landslides;
- falling from a height;
- disasters.
Dislocation occurs due to the indirect action of an external force placed directly on the femur . The latter acts as a lever. The impact of a traumatic factor on the hip joint itself usually leads to fractures of the femoral neck or pelvic bones.
In some cases, dislocation may be accompanied by pinching of the obturator nerves, compression of the femoral vessels, contusion of the sciatic nerve and fractures of the bones that form the acetabulum. If not treated in a timely manner, these complications can lead to the death of the soft tissues of the limb or even complete paralysis of the leg.
Fracture of the right (left) acetabulum on x-ray.
Hip joint dislocations usually occur in men and women under 50 years of age. Elderly people suffer from osteoporosis. The disease makes bones very fragile, making them easy to break. Therefore, at older ages, fractures of the femoral neck occur much more often.
Table 1. Classification of dislocations
| View | Description | Development mechanism |
| Suprapubular | The femoral head is located anterior to the ilium. The patient's leg is extended and turned outward. A convex formation is visible in the groin area, and the buttock on the side of the injured limb looks flattened | A sharp fall from a height onto an abducted, bent and turned outward leg |
| Obturator | The head of the femur is located next to the pubis. The lower limb is strongly turned outward, bent at the knee and hip joints | Similar to previous |
| Iliac | The femur is located behind the ilium. The leg is bent and turned inward. There is a protrusion in the buttock area, and a recess in the groin. On examination, shortening of the leg is noticeable. | Sudden bending or rotation of the leg at the knee and hip joint, which usually occurs in an accident |
| Sciatic | The head of the femur is located near the ischium. The deformity is more pronounced than with iliac dislocation | Similar to previous |
Main causes, symptoms and diagnosis of hip joint diseases
Pathological conditions in the hip most often develop against the background of:
- mechanical damage to joint elements;
- a tendency to diseases of the articular tissue of the hip area at the genetic level;
- functional impairment due to infection;
- systemic diseases in connective tissue;
- damage to the integrity of the joint due to degenerative-dystrophic transformations.
Any disease of the hip joint is characterized by the appearance of common symptoms:
- pain on the inner or outer thigh surface and in the groin area is of an acute, aching or pulling nature;
- motor activity is impaired, movements become limited;
- the skin becomes inflamed, the local temperature rises to subfebrile levels.
To correctly determine hip disease, a high-quality biochemical study is required. In addition, to accurately establish the diagnosis, instrumental diagnostic methods are shown:
- CT and MRI;
- Radiography;
- Ultrasound;
- Scintigraphy.
Let's consider the most common clinical diseases of the hip joint.
Hip dysplasia
This clinical disease is a congenital disorder or inferiority of the joint tissue, which increases the risk of subluxation or dislocation of the femoral head. The maximum number of cases of inadequate development of hip joints is observed in those areas where socio-economic policy is stable.
In the Scandinavian countries, the congenital anomaly is 4%, in Germany – 2%, and in the USA – 1-1.5%.
In the Russian Federation and post-Soviet countries, congenital dysplasia is diagnosed in 50-250 newborns out of 1000 (approximately 5%). According to medical experts, this is due to the unfavorable environmental situation in the states that were formerly part of the Soviet Union.
For the most part, the congenital disease is detected in female infants (in 80% of cases), as well as in families where one or both parents suffer from “congenital dysplasia.”
This congenital orthopedic anomaly can develop due to:
- breech presentation of the unborn baby;
- medical correction of pregnancy, which is complicated by toxicosis;
- large fruit.
A baby can develop dysplasia if he is swaddled too tightly to straighten his legs.
Since 1975, the Japanese have refused to tightly swaddle newborns. This has reduced the number of hip dislocations in infants.
Dysplasia in infants is manifested by the following clinical signs:
- asymmetrical skin folds on the legs;
- pronounced shortening of the thigh;
- restrictions in abduction and adduction of the hip joint.
A characteristic sign due to which one can suspect the presence of congenital dysplasia in a newborn is the Marx-Ortolani symptom. If you abduct the hip joint towards the surface where your baby is lying, you may hear a typical clicking sound in the joint area. This indicates that the femoral head is slipping into the acetabulum area.
The only effective therapy is to use a corrective orthopedic orthosis, thanks to which the baby’s legs can remain in a bent and abducted position at the required angle for a long time. Over time, the newborn is recommended to undergo massage, perform therapeutic exercises with constant supervision by an orthopedist. If treatment is started on time, the child can most often be cured.
Arthritis of the hip joint
Arthritis (coxitis) is a disease characterized by the development of an inflammatory process in the tissues of the hip joint. The disease occurs in acute (primary manifestations), protracted (2-12 months) or chronic form, which lasts more than a year.
Arthritic damage to the tissue system in the hip joint is divided into groups. It happens:
- infectious (septic coxitis) – inflammation that forms against the background of damage to the synovial fluid by an agent of a fungal, parasitic, infectious-allergic or viral nature;
- reactive arthritis - an immune-inflammatory pathology that manifests itself in the process or as a complication of infection of the joint tissue;
- rheumatoid arthritis is an autoimmune disease caused by the formation and spread of granulation tissue in the cavity of the synovial capsule. Because of this, articular cartilage and subchondral bone are destroyed;
- psoriatic arthritis is a rare autoimmune disease of the hip joint, manifested as a result of damage to joint tissue by psoriasis.
Symptoms, signs and treatment of hip coxitis
The causes, symptoms and therapeutic measures for arthritis of the hip joint depend on the nature of the disease.
The development of septic (infectious) arthritis is observed as a complication against the background of severe infection, which penetrates into the joint tissues through the bloodstream. This form of pathology is accompanied by joint pain, limitation of motor activity in the joint, redness and swelling in the problem area, hyperthermia within 39-40 degrees.
For therapeutic purposes, for infectious coxitis, anti-inflammatory drugs are prescribed for intramuscular, intravenous and intra-articular administration, as well as antiseptic and antipyretic drugs. In some cases, surgical treatment of the hip joints is required, which can be performed in Moscow in specialized centers. Failure to contact specialists in a timely manner is fraught with negative consequences; sometimes this disease causes the death of the patient.
The cause of reactive arthritis is an intestinal or urogenital infection. Pathology can also be caused by ureaplasma, streptococci and other microorganisms. This form of coxitis is characterized by the appearance of:
- pain in the hip joint;
- increased temperature;
- hyperemia and swelling of soft tissue in the damaged area;
- pain while walking or other activities.
Which medications will be prescribed for therapeutic purposes for reactive coxitis depends on the type of pathogen. The disease is easily treatable, the patient fully recovers after six months of drug therapy. In this case, the joint tissue is not destroyed.
The exact cause of the development of rheumatoid arthritis has not yet been determined. According to doctors, this is due to immunogenetic disorders in the body. This type of disease is accompanied by stiffness and pain in the joint in the morning, hyperthermia to low-grade levels (37-38 degrees). For rheumatoid arthritis, pharmacological agents of the antirheumatic, anti-inflammatory and hormonal group are indicated in the form of a course of treatment. It is not possible to completely cure coxitis of the rheumatoid form, but regular use of medications helps relieve the main pain syndromes of the pathology.
The psoriatic form of coxitis is a rather rare disease; it develops against the background of a skin pathology – psoriasis. With this disease, soft tissues become covered with dry red plaques, swelling forms, the temperature rises, and aches in the joints. Non-steroidal anti-inflammatory drugs are prescribed for therapeutic purposes. The outcome of the disease is determined by the severity of the condition.
Arthrosis (coxarthrosis)
Pain in the hip joint is often a sign of arthrosis of the hip joint. This is a chronic inflammatory disease, against the background of which dystrophic destruction is observed in the articular tissue of the hip joint.
Due to a lack of lubricating fluid, friction between the bones increases. This leads to the formation of growths on the head of the joint, which makes the functional activity of the joint tissue difficult.
If coxarthrosis of the hip joint is not treated in time, the patient will certainly lose the ability to move.
How to recognize pathology
Acquired dislocation of the hip joint in adults has pronounced symptoms that cannot be confused with anything else. Therefore, pathology is diagnosed without additional research methods. To exclude fractures of the femur or pelvic bones, a person is given an x-ray of the hip joint in two projections. If doctors have doubts about the diagnosis, they may order an MRI.
Symptoms of hip dislocation:
- unbearable pain at the site of projection of the hip joint;
- severe deformation in the joint area;
- unnatural position of the lower limb;
- increased pain in the hip joint when trying to move the leg;
- inability to walk and bend the leg at the hip;
- hemorrhages in the buttock or groin area.
Elena Malysheva about the injury:
Depending on the time of occurrence, dislocations can be fresh (less than 3 days), stale (3 days - 3 weeks) and old. The latter are characterized by thickening of the hip capsule and proliferation of connective tissue in the space around the joint. Such dislocations are very difficult to treat, and they can only be eliminated surgically.
With an old dislocation of the hip joint, the patient experiences the same symptoms, but they are less pronounced. The pain in the hip and groin becomes less pronounced, and the deformity becomes less obvious. A person gradually learns to walk with a dislocated joint, but this causes him to have other problems. Due to the asymmetry of the lower extremities, pelvic distortion and spinal curvature occur.
If you suspect a dislocated hip joint, seek medical help immediately. Don't try to treat yourself or hope that the problem will go away on its own. A fresh dislocation can be reduced, but an old one will have to be treated surgically.
Diagnostics
Hip dislocation on an x-ray
The main method for detecting a dislocation is ultrasound and x-ray of the affected area in frontal and lateral projection. Research allows us to understand how and to what extent bone structures are displaced. When studying the results, you can find associated fractures. A medical examination also plays a significant role in the diagnosis of injury.
If there is doubt, an MRI is prescribed. When symptoms of dislocation are detected in a child, you should contact a pediatric orthopedist. Diagnosis is carried out within 3 months after birth.
Treatment of hip dislocation in adults
Fresh traumatic dislocations require immediate medical attention. The victims are immediately hospitalized in a surgical hospital, where they are thoroughly examined. In the absence of fractures or other severe complications, the dislocation is reduced, and the hip joint is fixed with a plaster. After the fixator is removed, the patient undergoes rehabilitation, which usually lasts 2-3 months.
Providing first aid to the victim
The patient must be taken to the hospital as quickly as possible. It is better to do this not with an ordinary passenger car, but with a special machine. Therefore, the first thing to do if you suspect a dislocation is to call an ambulance. While waiting for paramedics to arrive, you can apply an ice pack or a piece of cloth soaked in cold water to the affected joint.
Arriving medical workers administer painkillers to the patient and perform transport immobilization of the injured limb. The leg is always fixed in the position in which it is located. After this, the person is taken to the trauma department as quickly as possible.
Reduction of a fresh dislocation
The manipulation is performed in an operating room. Since the procedure is very painful, it is done under general anesthesia . Dislocation of the hip joint is always accompanied by a strong reflex muscle contraction. Successful reduction is impossible without muscle relaxants . These drugs relieve muscle spasm, which allows the head of the femur to return to its place.
Reduction of the dislocation is performed by a trauma surgeon with the help of an assistant. During the manipulation, the specialist repeats in reverse order the movements that the femur made during the injury.
- Kocher reduction
. Used only for suprapubic dislocations. During the manipulation, the patient lies on his back. The surgeon's assistant firmly fixes the patient's pelvis with his hands. The doctor himself bends the leg at the knee and hip, then pulls it up, while simultaneously turning it inward. The appearance of a characteristic click indicates successful reduction; - reduction according to Dzhanelidze
. Applies in all other cases. The patient is placed on his stomach with the affected leg hanging down. The assistant holds the patient's pelvis with his hands. The doctor bends the dangling leg and places his knee on the popliteal fossa. By applying pressure, he simultaneously turns the person’s leg outward. The traumatologist completes the actions immediately after the click.
To make sure that the head of the femur is in place, the patient is given an x-ray. Only after this the patient is given a plaster cast.
How to avoid dislocations: a list of prevention rules
An artificial analogue of hip joints can serve efficiently for 15-30 years, but only under the condition of conscientious compliance with lifelong requirements. It is necessary to clearly understand that dislocations often occur due to the fault of the patient himself, who violated the principles of proper lifestyle and physical activity. So, to prevent postoperative consequences, including its relapse, it is necessary:
- regularly take control photographs of the operated area (for the first time they are taken after 3 months, then 6 and 12 months after the operation, then once annually);
- do exercise therapy daily – 1-2 times a day;
- avoid jumping, crossing legs, squatting, any sudden body maneuvers, overloading the section, twisting in the pelvic girdle area;
- sit on chairs of normal height with level back support, keep your spine straight while sitting;
- take all precautions to prevent traumatic situations;
- wear comfortable shoes with orthopedic soles, avoid high-heeled shoes and high-platform shoes;
- eat a balanced diet, monitor your weight (if your body weight is higher than normal, consult a nutritionist for help in losing weight);
- do not lift heavy objects and do not allow work associated with heavy physical labor;
- If you experience supporting and motor discomfort, pain, or swelling in the area of the endoprosthesis, immediately consult a doctor;
- if the problem persists, fully recover after the reduction of the head of the joint is performed in a medical facility.
Attention! To prevent dislocations, doctors recommend a special set of exercises aimed at effectively working out and increasing the endurance of the hip and gluteal muscles. It is extremely important to strengthen these muscle groups, because they are the main regulators of movement and stabilizers of the implant joint.
Therapeutic measures in the postoperative period
After making sure that the dislocation has been successfully reduced, doctors apply a plaster splint to the lower limb. It fixes the ankle, knee, hip joints and reaches the lower back. The patient is then placed on bed rest for three to four weeks. After getting out of bed, a person walks with crutches for another month and a half to two months. The plaster is removed no earlier than 2-3 months after the injury.
In some cases, the patient undergoes skeletal traction for 3-4 weeks. To do this, a special needle is inserted into the tibia under anesthesia, onto which a weight is attached.
High-quality treatment for hip dislocation in adults must include rehabilitation . It includes a course of massage, therapeutic exercises and physiotherapeutic procedures. Complete rehabilitation helps restore normal functions of the lower limb and gives a person the opportunity to return to normal life.
First aid
If you suspect a hip dislocation, you should immediately seek medical help. The doctor performs reduction of a dislocated hip only under anesthesia. It is forbidden to try to straighten the joint yourself. Making the slightest mistake can aggravate the situation and even cause disability. However, first aid to the victim is necessary:
- Give an intramuscular injection of anesthetic.
- Keep the leg stationary. To do this, use bandages, sticks, reinforcement, etc. You can tape the diseased limb to the healthy one. The basic rule is that the leg should be in the same position as after the injury.
- Apply a cold compress to the hip joint.
After the described actions, you need to wait for the ambulance to arrive, since it is undesirable to transport the patient yourself - you can aggravate the situation.
Treatment of old and complicated dislocations of the hip joint
If health care workers are unable to reduce the dislocation using a closed method, they perform an open reduction of the dislocation. During the operation, the doctor makes an incision through which he gains access to the joint. He manually resets the femoral head and sutures the wound. Surgical intervention is also required for ligament ruptures, massive soft tissue injuries and chronic dislocations.
Video about patients after surgery:
Even timely and adequate treatment of injury does not always lead to complete recovery. Some patients develop deforming osteoarthritis over time due to damage to articular cartilage. The disease leads to severe pain when walking and deformation of the hip joint. The pathology can be cured only with the help of endoprosthetics - replacing a joint with an artificial prosthesis.
Complications after hip joint dislocation
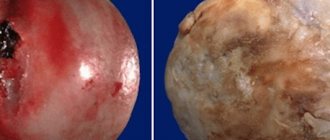
Aseptic necrosis develops when the blood supply to the joint is disrupted.
Since hip dislocation is a serious injury, severe complications can occur after it, even with proper and timely treatment. 20% of patients develop late osteoarthritis, which progresses over the years.
In advanced cases, when dislocations become old, the risk of damage to blood vessels increases, which leads to disruption of the nutrition of the femoral head. From 10 to 40% of patients who have undergone hip replacement experience hip necrosis and damage to synovial tissue.
Complications include sciatic nerve rupture, as well as lameness and disability. The head of the bone may protrude from the capsule, damaging the acetabulum, which can trigger inflammatory arthritis.
Hip dislocation in children
Hip dysplasia is a common pathology of the musculoskeletal system in newborns, accounting for about 3% of all orthopedic diseases. It occurs due to improper formation of the joint in the prenatal period. According to statistics, unilateral dislocations occur seven times more often than bilateral ones, and in girls the pathology is detected five times more often than in boys.
50% of all hip dysplasia develops in children born in breech presentation. However, the nature of obstetric care and the mechanism of labor itself do not in any way affect the occurrence of pathology. This confirms the presence of hip deformity in babies born by caesarean section.
The group of hip dysplasias in children includes preluxation, subluxation, dislocation and radiologically immature hip joint. Diseases are usually diagnosed in early childhood through routine examinations by a pediatrician and orthopedist. Sometimes the pathology is detected much later, when the child begins to walk.
Traumatologist of the highest category Sumin A.I:
Symptoms indicating hip dysplasia in a newborn:
- visible shortening of the affected leg;
- asymmetrical arrangement of the gluteal, femoral and popliteal folds;
- external rotation of the limb, especially noticeable during sleep;
- the appearance of a characteristic crunch when the legs are abducted;
- inability to abduct a limb bent at the hip joint by more than 70-90 degrees;
- displacement of the femoral head when palpated.
In children over 1 year of age, congenital pathology manifests itself as an unsteady gait and lameness. The child has a curvature of the spine in the lumbar region. Sick children usually start walking later than healthy ones.
Treatment of dislocations and subluxations of the hip joint in children begins in the first weeks of life. To combat pathology, wide swaddling, Pavlik stirrups, and special therapeutic splints are used. Along with this, the child is prescribed physiotherapeutic procedures, massage, and physical therapy. If conservative therapy is ineffective, the baby undergoes open reduction with arthroplasty.
The most suitable age for surgical intervention in a child is considered to be 2-3 years of age.
Anatomical features
The hip joint is a nut-shaped joint with three degrees of freedom of movement around three main axes: in the frontal plane – adduction and abduction, in the sagittal plane – flexion and extension, in the horizontal plane – rotational movements.
Despite such a motor load on the hip joint, dislocations in it do not occur so often compared to the shoulder and elbow joints.
This can be explained by the fact that the joint has a deep socket, five strong ligaments and a well-developed muscle layer overlying the joint.